| [1] |
LI L, LIU DW, YAN HY, et al. Obesity is an independent risk factor for non-alcoholic fatty liver disease: Evidence from a meta-analysis of 21 cohort studies[J]. Obes Rev, 2016, 17( 6): 510- 519. DOI: 10.1111/obr.12407. |
| [2] |
WORETA TA, van NATTA ML, LAZO M, et al. Validation of the accuracy of the FAST™ score for detecting patients with at-risk nonalcoholic steatohepatitis(NASH) in a North American cohort and comparison to other non-invasive algorithms[J]. PLoS One, 2022, 17( 4): e0266859. DOI: 10.1371/journal.pone.0266859. |
| [3] |
CHO EEL, ANG CZ, QUEK J, et al. Global prevalence of non-alcoholic fatty liver disease in type 2 diabetes mellitus: An updated systematic review and meta-analysis[J]. Gut, 2023, 72( 11): 2138- 2148. DOI: 10.1136/gutjnl-2023-330110. |
| [4] |
SANYAL AJ, van NATTA ML, CLARK J, et al. Prospective study of outcomes in adults with nonalcoholic fatty liver disease[J]. N Engl J Med, 2021, 385( 17): 1559- 1569. DOI: 10.1056/NEJMoa2029349. |
| [5] |
ALON L, CORICA B, RAPARELLI V, et al. Risk of cardiovascular events in patients with non-alcoholic fatty liver disease: A systematic review and meta-analysis[J]. Eur J Prev Cardiol, 2022, 29( 6): 938- 946. DOI: 10.1093/eurjpc/zwab212. |
| [6] |
BISACCIA G, RICCI F, KHANJI MY, et al. Cardiovascular morbidity and mortality related to non-alcoholic fatty liver disease: A systematic review and meta-analysis[J]. Curr Probl Cardiol, 2023, 48( 6): 101643. DOI: 10.1016/j.cpcardiol.2023.101643. |
| [7] |
WANG L, SINNOTT-ARMSTRONG N, WAGSCHAL A, et al. A MicroRNA linking human positive selection and metabolic disorders[J]. Cell, 2020, 183( 3): 684- 701. e 14. DOI: 10.1016/j.cell.2020.09.017. |
| [8] |
ZHAO XR, JIN Y, LI L, et al. MicroRNA-128-3p aggravates doxorubicin-induced liver injury by promoting oxidative stress via targeting Sirtuin-1[J]. Pharmacol Res, 2019, 146: 104276. DOI: 10.1016/j.phrs.2019.104276. |
| [9] |
SHI RF, JIN YP, HU WW, et al. Exosomes derived from mmu_circ_0000250-modified adipose-derived mesenchymal stem cells promote wound healing in diabetic mice by inducing miR-128-3p/SIRT1-mediated autophagy[J]. Am J Physiol Cell Physiol, 2020, 318( 5): C848- C856. DOI: 10.1152/ajpcell.00041.2020. |
| [10] |
HAN JN, HAO WJ, MA YP, et al. MiR-128-3p promotes the progression of deep venous thrombosis through binding SIRT1[J]. Phlebology, 2023, 38( 8): 540- 549. DOI: 10.1177/02683555231190268. |
| [11] |
Diabetes Society of Chinese Medical Association. Guideline for the prevention and treatment of type 2 diabetes mellitus in China(2020 edition)[J]. Chin J Diabetes, 2021, 13( 4): 315- 409. DOI: 10.3760/cma.j.cn115791-20210307-00135. |
| [12] |
National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association, Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: A 2018 update[J]. J Clin Hepatol, 2018, 34( 5): 947- 957. DOI: 10.3969/j.issn.1001-5256.2018.05.007. |
| [13] |
WANG XS, JIANG LJ, SHAO XN. Association analysis of insulin resistance and osteoporosis risk in Chinese patients with T2DM[J]. Ther Clin Risk Manag, 2021, 17: 909- 916. DOI: 10.2147/TCRM.S328510. |
| [14] |
ANGULO P, HUI JM, MARCHESINI G, et al. The NAFLD fibrosis score: A noninvasive system that identifies liver fibrosis in patients with NAFLD[J]. Hepatology, 2007, 45( 4): 846- 854. DOI: 10.1002/hep.21496. |
| [15] |
TARGHER G, COREY KE, BYRNE CD, et al. The complex link between NAFLD and type 2 diabetes mellitus—Mechanisms and treatments[J]. Nat Rev Gastroenterol Hepatol, 2021, 18( 9): 599- 612. DOI: 10.1038/s41575-021-00448-y. |
| [16] |
STEFAN N, CUSI K. A global view of the interplay between non-alcoholic fatty liver disease and diabetes[J]. Lancet Diabetes Endocrinol, 2022, 10( 4): 284- 296. DOI: 10.1016/S2213-8587(22)00003-1. |
| [17] |
SONG SJ, LAI JCT, WONG GLH, et al. Can we use old NAFLD data under the new MASLD definition?[J]. J Hepatol, 2024, 80( 2): e54- e56. DOI: 10.1016/j.jhep.2023.07.021. |
| [18] |
MANTOVANI A, CSERMELY A, TAVERNA A, et al. Association between metabolic dysfunction-associated fatty liver disease and supraventricular and ventricular tachyarrhythmias in patients with type 2 diabetes[J]. Diabetes Metab, 2023, 49( 2): 101416. DOI: 10.1016/j.diabet.2022.101416. |
| [19] |
NI XT, TONG C, HALENGBIEKE A, et al. Association between nonalcoholic fatty liver disease and type 2 diabetes: A bidirectional two-sample Mendelian randomization study[J]. Diabetes Res Clin Pract, 2023, 206: 110993. DOI: 10.1016/j.diabres.2023.110993. |
| [20] |
ISMAIL MH, ARGAN R AL, ELAMIN Y, et al. Automated fibrosis-4 index: Simplifying non-alcoholic fatty liver disease for diabetologists[J]. Medicina(Kaunas), 2024, 60( 8): 1278. DOI: 10.3390/medicina60081278. |
| [21] |
|
| [22] |
UDDIN A, CHAKRABORTY S. Role of miRNAs in lung cancer[J]. J Cell Physiol, 2018. DOI: 10.1002/jcp.26607.[ Online ahead of print] |
| [23] |
YANG JN, JIANG TL, ZHU FB, et al. Research progress in effect of miRNA on podocyte injury in diabetic nephropathy and its mechanism[J]. J Jilin Univ(Med Edit), 2023, 49( 6): 1677- 1682. DOI: 10.13481/j.1671-587X.20230637. |
| [24] |
WEI HF, NI ZQ, WEI YH, et al. Effects of miR-126 over-expression and ADAM9 gene silencing on biological behavior of gastric cancer SGC-7901 cells and their mechanisms[J]. J Jilin Univ(Med Edit), 2024, 50( 2): 310- 319. DOI: 10.13481/j.1671-587X.20240203. |
| [25] |
SUN T, WANG C, HUO L, et al. Serum cortistatin level in type 2 diabetes mellitus and its relationship with nonalcoholic fatty liver disease[J]. Int J Gen Med, 2023, 16: 631- 639. DOI: 10.2147/IJGM.S396315. |
| [26] |
HIRANO T, SATOH N, ITO Y. Specific increase in small dense low-density lipoprotein-cholesterol levels beyond triglycerides in patients with diabetes: Implications for cardiovascular risk of MAFLD[J]. J Atheroscler Thromb, 2024, 31( 1): 36- 47. DOI: 10.5551/jat.64271. |
| [27] |
BI TB. Relationship between thyroid hormone levels and metabolic dysfunction associated steatotic liver disease in patients with type 2 diabetes: A clinical study[J]. Medicine(Baltimore), 2024, 103( 26): e38643. DOI: 10.1097/MD.0000000000038643. |
| [28] |
ZHANG XD, CHEN YM, YE HY, et al. Correlation between thyroid function, sensitivity to thyroid hormones and metabolic dysfunction-associated fatty liver disease in euthyroid subjects with newly diagnosed type 2 diabetes[J]. Endocrine, 2023, 80( 2): 366- 379. DOI: 10.1007/s12020-022-03279-2. |
| [29] |
HEIANZA Y, XUE QC, ROOD J, et al. Circulating thrifty microRNA is related to insulin sensitivity, adiposity, and energy metabolism in adults with overweight and obesity: The POUNDS lost trial[J]. Am J Clin Nutr, 2023, 117( 1): 121- 129. DOI: 10.1016/j.ajcnut.2022.10.001. |
| [30] |
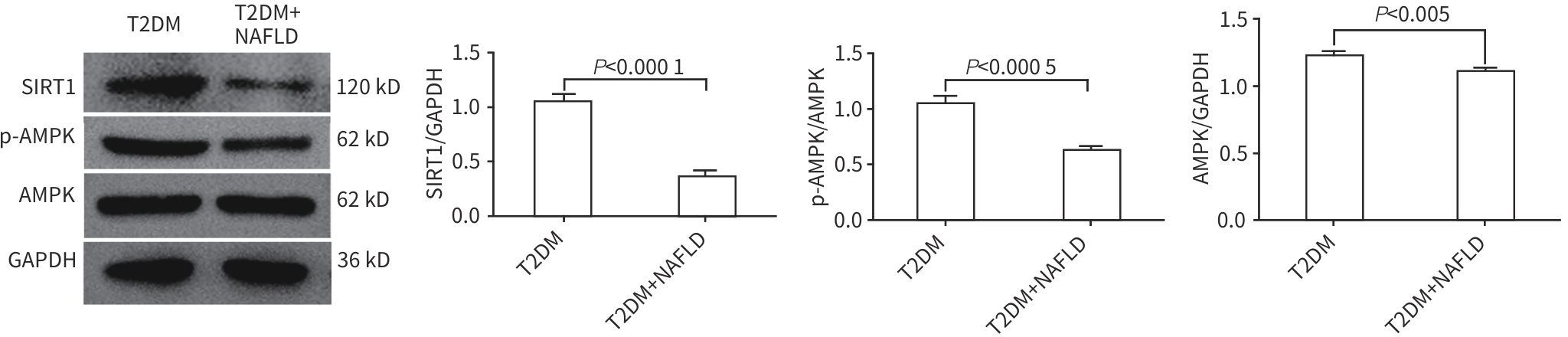
CHANG E. Vitamin D mitigates hepatic fat accumulation and inflammation and increases SIRT1/AMPK expression in AML-12 hepatocytes[J]. Molecules, 2024, 29( 6): 1401. DOI: 10.3390/molecules29061401. |
| [31] |
XIAO Q, ZHANG SJ, YANG C, et al. Ginsenoside Rg1 ameliorates palmitic acid-induced hepatic steatosis and inflammation in HepG2 cells via the AMPK/NF-κB pathway[J]. Int J Endocrinol, 2019, 2019: 7514802. DOI: 10.1155/2019/7514802. |
| [32] |
WU LZ, ZHANG GR, GUO CB, et al. MiR-128-3p mediates TNF-α-induced inflammatory responses by regulating Sirt1 expression in bone marrow mesenchymal stem cells[J]. Biochem Biophys Res Commun, 2020, 521( 1): 98- 105. DOI: 10.1016/j.bbrc.2019.10.083. |
| [33] |
SAMY AM, KANDEIL MA, SABRY D, et al. Exosomal miR-122, miR-128, miR-200, miR-298, and miR-342 as novel diagnostic biomarkers in NAFL/NASH: Impact of LPS/TLR-4/FoxO3 pathway[J]. Arch Pharm(Weinheim), 2024, 357( 4): e2300631. DOI: 10.1002/ardp.202300631. |






 DownLoad:
DownLoad: