| [1] |
CHEN SC, ZHU JF, SUN LQ, et al. LincRNA-EPS alleviates severe acute pancreatitis by suppressing HMGB1-triggered inflammation in pancreatic macrophages[J]. Immunology, 2021, 163( 2): 201- 219. DOI: 10.1111/imm.13313. |
| [2] |
BARRETO SG, HABTEZION A, GUKOVSKAYA A, et al. Critical thresholds: Key to unlocking the door to the prevention and specific treatments for acute pancreatitis[J]. Gut, 2021, 70( 1): 194- 203. DOI: 10.1136/gutjnl-2020-322163. |
| [3] |
HU XY, YANG ZY, ZHAO CJ, et al. Research progress in acute pancreatitis scoring systems in predicting the severity of disease[J/OL]. Chin J Hepatic Surg(Electronic Edition), 2024, 13( 2): 239- 243. DOI: 10.3877/cma.j.issn.2095-3232.2024.02.021. |
| [4] |
HARSHIT KUMAR A, SINGH GRIWAN M. A comparison of APACHE II, BISAP, Ranson’s score and modified CTSI in predicting the severity of acute pancreatitis based on the 2012 revised Atlanta Classification[J]. Gastroenterol Rep, 2018, 6( 2): 127- 131. DOI: 10.1093/gastro/gox029. |
| [5] |
DI MY, LIU H, YANG ZY, et al. Prediction models of mortality in acute pancreatitis in adults: A systematic review[J]. Ann Intern Med, 2016, 165( 7): 482- 490. DOI: 10.7326/M16-0650. |
| [6] |
SILVA-VAZ P, ABRANTES AM, CASTELO-BRANCO M, et al. Multifactorial scores and biomarkers of prognosis of acute pancreatitis: Applications to research and practice[J]. Int J Mol Sci, 2020, 21( 1): 338. DOI: 10.3390/ijms21010338. |
| [7] |
KUMARI R, KUMAR S, KANT R. An update on metabolic syndrome: Metabolic risk markers and adipokines in the development of metabolic syndrome[J]. Diabetes Metab Syndr, 2019, 13( 4): 2409- 2417. DOI: 10.1016/j.dsx.2019.06.005. |
| [8] |
ZHAO CL, SHANG DF, ZHOU C, et al. Mechanism of lipid metabolism mediated by hepatokines and adipokines in nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2023, 39( 1): 168- 174. DOI: 10.3969/j.issn.1001-5256.2023.01.026. |
| [9] |
YIN JY, WANG Q. Progress on adipokines in non-alcoholic fatty liver disease[J/CD]. Chin J Liver Dis(Electronic Version), 2023, 15( 1): 1- 5. DOI: 10.3969/j.issn.1674-7380.2023.01.001. |
| [10] |
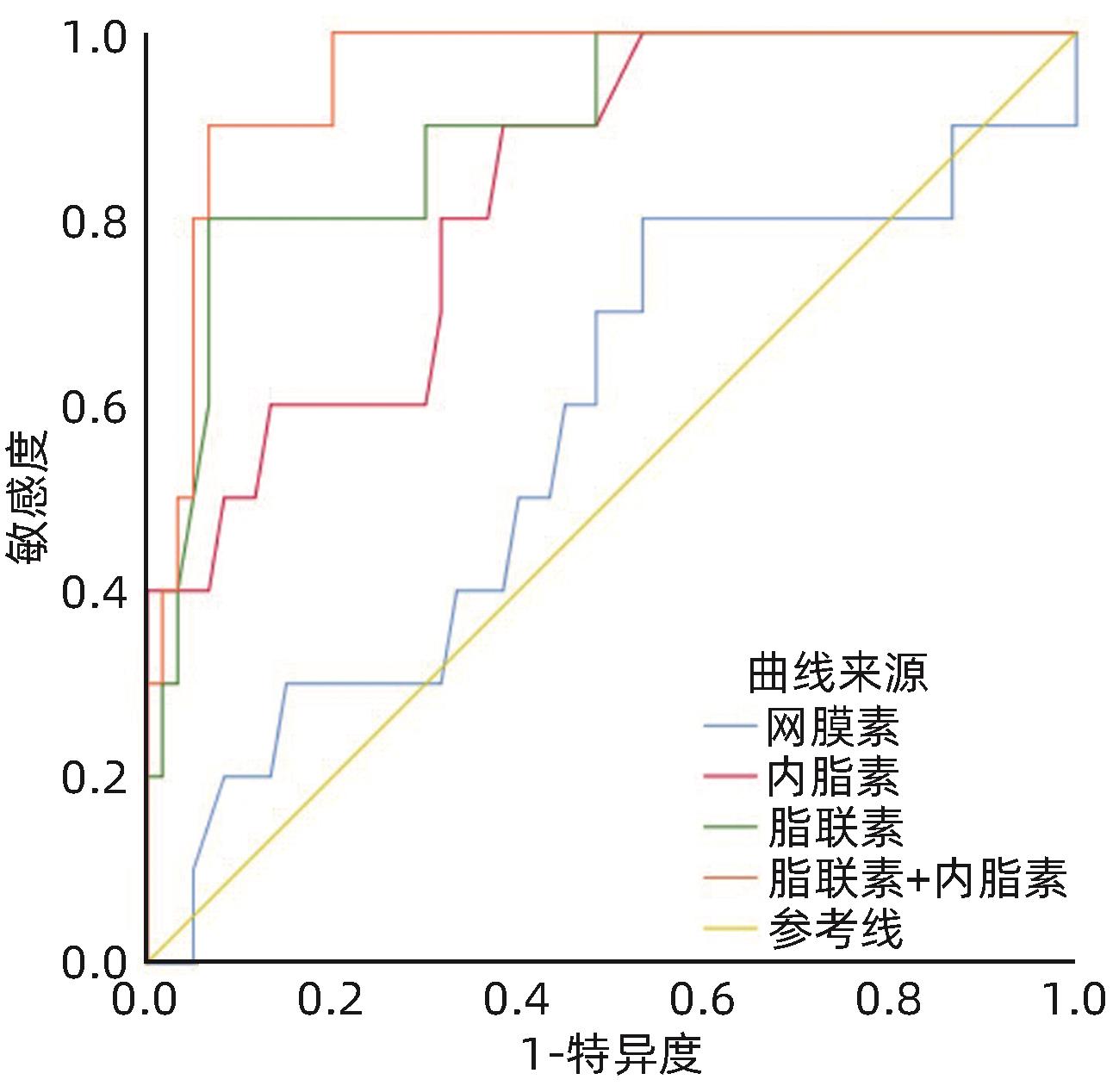
SCHÄFFLER A, LANDFRIED K, VÖLK M, et al. Potential of adipocytokines in predicting peripancreatic necrosis and severity in acute pancreatitis: Pilot study[J]. J Gastroenterol Hepatol, 2007, 22( 3): 326- 334. DOI: 10.1111/j.1440-1746.2006.04364.x. |
| [11] |
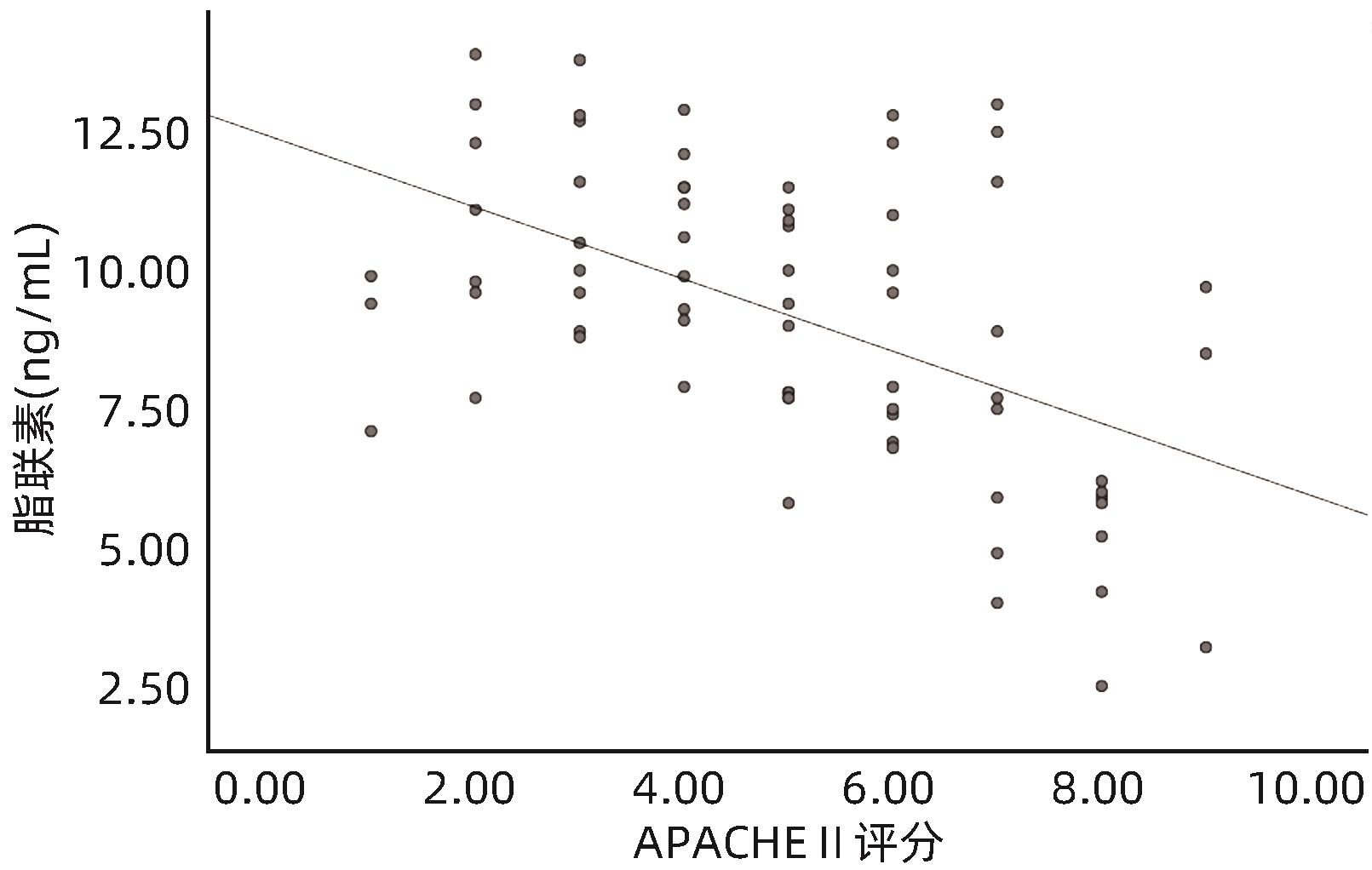
SHARMA A, MUDDANA V, LAMB J, et al. Low serum adiponectin levels are associated with systemic organ failure in acute pancreatitis[J]. Pancreas, 2009, 38( 8): 907- 912. DOI: 10.1097/MPA.0b013e3181b65bbe. |
| [12] |
KARPAVICIUS A, DAMBRAUSKAS Z, GRADAUSKAS A, et al. The clinical value of adipokines in predicting the severity and outcome of acute pancreatitis[J]. BMC Gastroenterol, 2016, 16( 1): 99. DOI: 10.1186/s12876-016-0514-4. |
| [13] |
Group of Pancreatic Surgery, Surgery Society of Chinese Medical Association. Guidelines for diagnosis and treatment of acute pancreatitis in China(2021)[J]. Chin J Surg, 2021, 59( 7): 578- 587. DOI: 10.3760/cma.j.cn112139-20210416-00172. |
| [14] |
LI CR, LI X, LIU LX. Research progress of adipokine and acute pancreatitis[J]. Adv Clin Med, 2023, 13( 7): 11609- 11614. DOI: 10.12677/acm.2023.1371624. |
| [15] |
YAVUZ N, UNAL E, MEMISOGLU K, et al. Plasma leptin levels in rats with pancreatitis[J]. Tohoku J Exp Med, 2004, 204( 4): 243- 248. DOI: 10.1620/tjem.204.243. |
| [16] |
SCHERER PE, WILLIAMS S, FOGLIANO M, et al. A novel serum protein similar to C1q, produced exclusively in adipocytes[J]. J Biol Chem, 1995, 270( 45): 26746- 26749. DOI: 10.1074/jbc.270.45.26746. |
| [17] |
KARPAVICIUS A, DAMBRAUSKAS Z, SILEIKIS A, et al. Value of adipokines in predicting the severity of acute pancreatitis: Comprehensive review[J]. World J Gastroenterol, 2012, 18( 45): 6620- 6627. DOI: 10.3748/wjg.v18.i45.6620. |
| [18] |
WATANABE T, WATANABE-KOMINATO K, TAKAHASHI Y, et al. Adipose tissue-derived omentin-1 function and regulation[J]. Compr Physiol, 2017, 7( 3): 765- 781. DOI: 10.1002/cphy.c160043. |
| [19] |
RAO SS, HU Y, XIE PL, et al. Omentin-1 prevents inflammation-induced osteoporosis by downregulating the pro-inflammatory cytokines[J]. Bone Res, 2018, 6: 9. DOI: 10.1038/s41413-018-0012-0. |
| [20] |
LIU HP, WU JF, WANG HY, et al. Association of serum omentin-1 concentrations with the presence and severity of preeclampsia[J]. Ann Clin Biochem, 2015, 52( 2): 245- 250. DOI: 10.1177/0004563214541247. |
| [21] |
ALI S, ALAM R, AHSAN H, et al. Role of adipokines(omentin and visfatin) in coronary artery disease[J]. Nutr Metab Cardiovasc Dis, 2023, 33( 3): 483- 493. DOI: 10.1016/j.numecd.2022.11.023. |
| [22] |
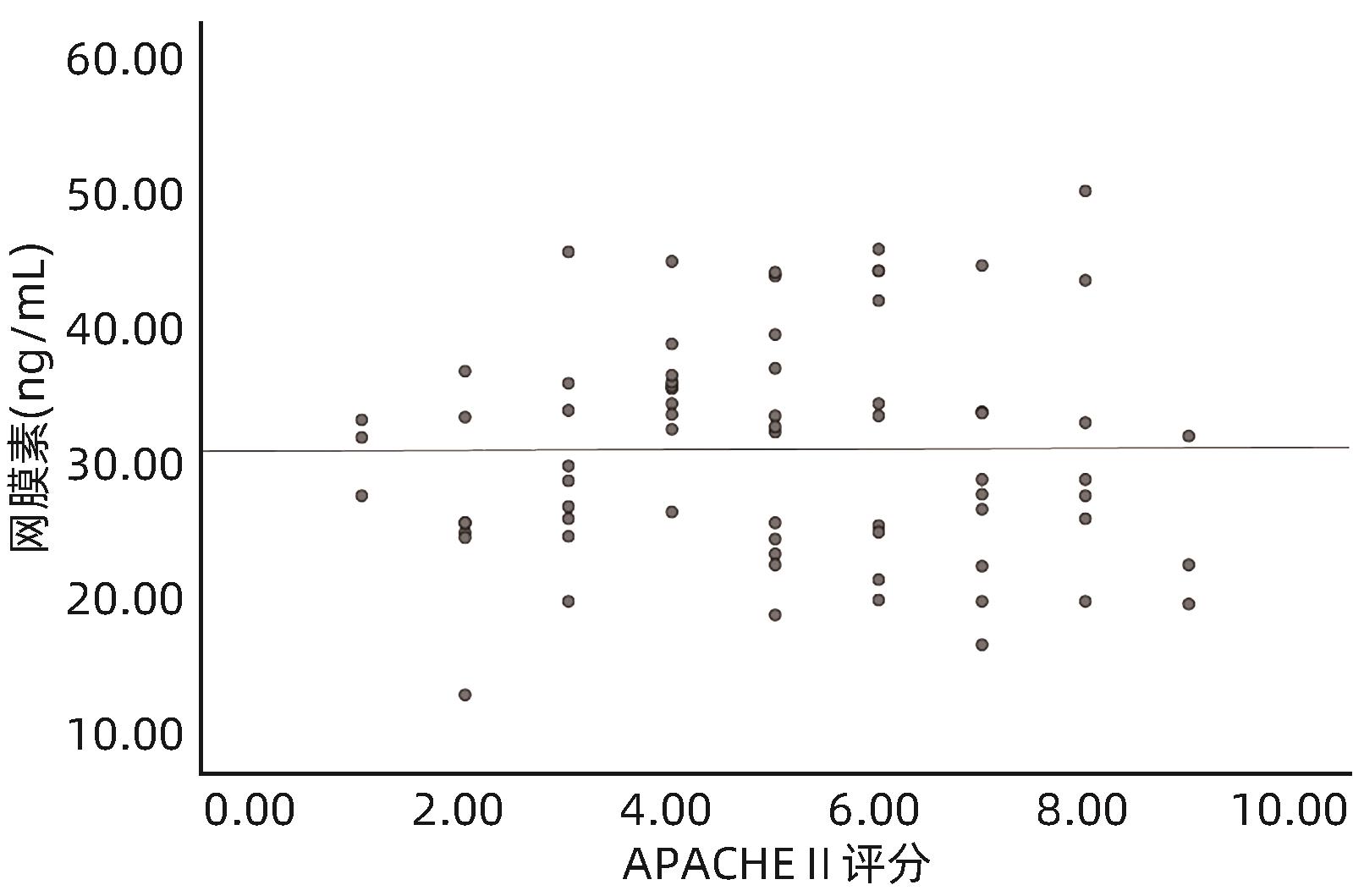
SIT M, AKTAS G, YILMAZ EE, et al. Effects of the inflammatory response on serum omentin levels in early acute and chronic pancreatitis[J]. Clin Ter, 2014, 165( 2): e148- e152. DOI: 10.7471/CT.2014.1699. |
| [23] |
MOSCHEN AR, KASER A, ENRICH B, et al. Visfatin, an adipocytokine with proinflammatory and immunomodulating properties[J]. J Immunol, 2007, 178( 3): 1748- 1758. DOI: 10.4049/jimmunol.178.3.1748. |
| [24] |
SAWICKA K, MICHALSKA-JAKUBUS M, POTEMBSKA E, et al. Visfatin and chemerin levels correspond with inflammation and might reflect the bridge between metabolism, inflammation and fibrosis in patients with systemic sclerosis[J]. Postepy Dermatol Alergol, 2019, 36( 5): 551- 565. DOI: 10.5114/ada.2018.79104. |
| [25] |
LU Y, TAO DX, HE ML. Expression of serum adipocytokines, lactones and IL-33 in patients with inflammatory bowel disease and their correlation with intestinal flora[J]. Mod Dig Interv, 2021, 26( 1): 85- 90. DOI: 10.3969/j.issn.1672-2159.2021.01.018. |
| [26] |
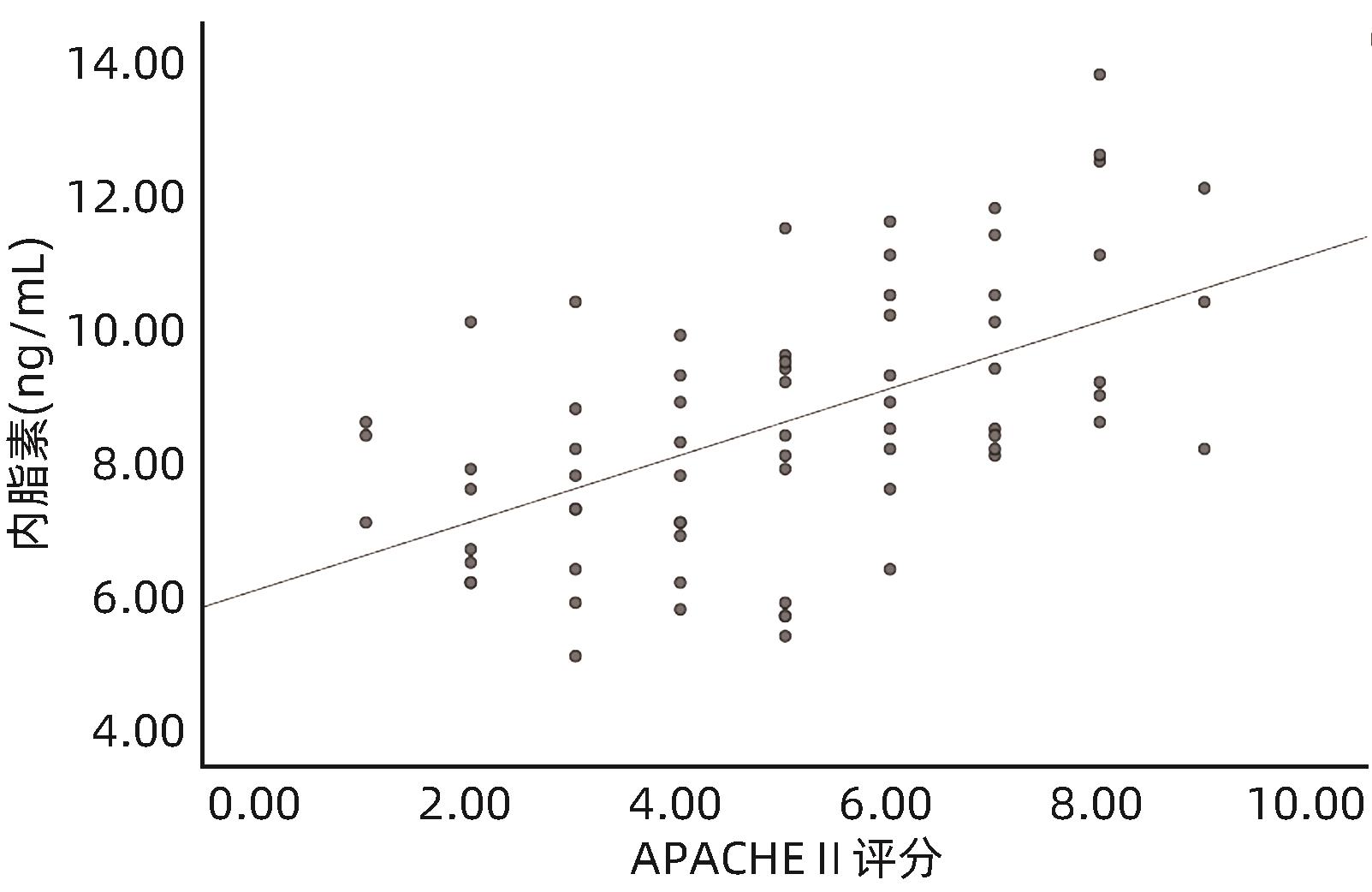
SCHÄFFLER A, HAMER OW, DICKOPF J, et al. Admission visfatin levels predict pancreatic and peripancreatic necrosis in acute pancreatitis and correlate with clinical severity[J]. Am J Gastroenterol, 2011, 106( 5): 957- 967. DOI: 10.1038/ajg.2010.503. |
| [27] |
MEI PF, HUANG MF, KONG H, et al. Study on the correlation between serum visfatin changes and illness in patients with acute pancreatitis[J]. Chin J Pancreatol, 2015, 15( 1): 44- 45. DOI: 10.3760/cma.j.issn.1674-1935.2015.01.011. |







 DownLoad:
DownLoad: