| [1] |
FERLAY J, COLOMBET M, SOERJOMATARAM I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods[J]. Int J Cancer, 2019, 144( 8): 1941- 1953. DOI: 10.1002/ijc.31937. |
| [2] |
AN L, ZHENG RS, ZHANG SW, et al. Hepatocellular carcinoma and intrahepatic cholangiocarcinoma incidence between 2006 and 2015 in China: Estimates based on data from 188 population-based cancer registries[J]. Hepatobiliary Surg Nutr, 2023, 12( 1): 45- 55. DOI: 10.21037/hbsn-21-75. |
| [3] |
SIEGEL RL, MILLER KD, WAGLE NS, et al. Cancer statistics, 2023[J]. CA A Cancer J Clin, 2023, 73( 1): 17- 48. DOI: 10.3322/caac.21763. |
| [4] |
WEI WQ, ZENG HM, ZHENG RS, et al. Cancer registration in China and its role in cancer prevention and control[J]. Lancet Oncol, 2020, 21( 7): e342- e349. DOI: 10.1016/S1470-2045(20)30073-5. |
| [5] |
|
| [6] |
KNITTER S, RASCHZOK N, HILLEBRANDT KH, et al. Short-term postoperative outcomes of lymphadenectomy for cholangiocarcinoma, hepatocellular carcinoma and colorectal liver metastases in the modern era of liver surgery: Insights from the StuDoQ|Liver registry[J]. Eur J Surg Oncol, 2024, 50( 4): 108010. DOI: 10.1016/j.ejso.2024.108010. |
| [7] |
LI ML, LIU FT, ZHANG F, et al. Genomic ERBB2/ ERBB3 mutations promote PD-L1-mediated immune escape in gallbladder cancer: A whole-exome sequencing analysis[J]. Gut, 2019, 68( 6): 1024- 1033. DOI: 10.1136/gutjnl-2018-316039. |
| [8] |
SAHU S, SUN WJ. Targeted therapy in biliary tract cancers-current limitations and potentials in the future[J]. J Gastrointest Oncol, 2017, 8( 2): 324- 336. DOI: 10.21037/jgo.2016.09.16. |
| [9] |
TOLEDO B, DEIANA C, SCIANÒ F, et al. Treatment resistance in pancreatic and biliary tract cancer: Molecular and clinical pharmacology perspectives[J]. Expert Rev Clin Pharmacol, 2024, 17( 4): 323- 347. DOI: 10.1080/17512433.2024.2319340. |
| [10] |
COSGROVE DP, REESE ES, FULCHER NM, et al. Real-world outcomes among patients with advanced or metastatic biliary tract cancers initiating second-line treatment[J]. Cancer Med, 2023, 12( 4): 4195- 4205. DOI: 10.1002/cam4.5282. |
| [11] |
SATO K, HAYASHI M, ABE K, et al. Pembrolizumab-induced sclerosing cholangitis in a lung adenocarcinoma patient with a remarkable response to chemotherapy: A case report[J]. Clin J Gastroenterol, 2020, 13( 6): 1310- 1314. DOI: 10.1007/s12328-020-01178-5. |
| [12] |
MAWSON AR, CROFT AM, GONZALEZ-FERNANDEZ F. Liver damage and exposure to toxic concentrations of endogenous retinoids in the pathogenesis of COVID-19 disease: Hypothesis[J]. Viral Immunol, 2021, 34( 6): 376- 379. DOI: 10.1089/vim.2020.0330. |
| [13] |
HU YF, LI SX, LIU HL, et al. Precirrhotic primary biliary cholangitis with portal hypertension: Bile duct injury correlate[J]. Gut Liver, 2024, 18( 5): 867- 876. DOI: 10.5009/gnl230468. |
| [14] |
XIE LJ, RUAN DD, ZHANG JH, et al. Mutational analysis of a familial adenomatous polyposis pedigree with bile duct polyp phenotype[J]. Can J Gastroenterol Hepatol, 2021, 2021: 6610434. DOI: 10.1155/2021/6610434. |
| [15] |
OVERI D, CARPINO G, CRISTOFERI L, et al. Role of ductular reaction and ductular-canalicular junctions in identifying severe primary biliary cholangitis[J]. JHEP Rep, 2022, 4( 11): 100556. DOI: 10.1016/j.jhepr.2022.100556. |
| [16] |
LIN CA, WANG YW, LIU CY, et al. Regulatory T cells in inflamed liver are dysfunctional in murine primary biliary cholangitis[J]. Clin Exp Immunol, 2024, 215( 3): 225- 239. DOI: 10.1093/cei/uxad117. |
| [17] |
ARREAZA-GIL V, ESCOBAR-MARTÍNEZ I, MUGUERZA B, et al. The effects of grape seed proanthocyanidins in Cafeteria diet-induced obese Fischer 344 rats are influenced by faecal microbiota in a photoperiod dependent manner[J]. Food Funct, 2022, 13( 16): 8363- 8374. DOI: 10.1039/d2fo01206e. |
| [18] |
FARSHBAFNADI M, AGAH E, REZAEI N. The second brain: The connection between gut microbiota composition and multiple sclerosis[J]. J Neuroimmunol, 2021, 360: 577700. DOI: 10.1016/j.jneuroim.2021.577700. |
| [19] |
SOTTAS C, SCHMIEDOVÁ L, KREISINGER J, et al. Gut microbiota in two recently diverged passerine species: Evaluating the effects of species identity, habitat use and geographic distance[J]. BMC Ecol Evol, 2021, 21( 1): 41. DOI: 10.1186/s12862-021-01773-1. |
| [20] |
GU SM, XIE Q, CHEN C, et al. Gut microbial signatures associated with peanut allergy in a BALB/c mouse model[J]. Foods, 2022, 11( 10): 1395. DOI: 10.3390/foods11101395. |
| [21] |
KIM JK, CHOI MS, KIM JY, et al. Ginkgo biloba leaf extract suppresses intestinal human breast cancer resistance protein expression in mice: Correlation with gut microbiota[J]. Biomed Pharmacother, 2021, 140: 111712. DOI: 10.1016/j.biopha.2021.111712. |
| [22] |
VERHAAR BJH, MOSTERD CM, COLLARD D, et al. Sex differences in associations of plasma metabolites with blood pressure and heart rate variability: The HELIUS study[J]. Atherosclerosis, 2023, 384: 117147. DOI: 10.1016/j.atherosclerosis.2023.05.016. |
| [23] |
MIHAJLOVIC J, LEUTNER M, HAUSMANN B, et al. Combined hormonal contraceptives are associated with minor changes in composition and diversity in gut microbiota of healthy women[J]. Environ Microbiol, 2021, 23( 6): 3037- 3047. DOI: 10.1111/1462-2920.15517. |
| [24] |
SAAB M, MESTIVIER D, SOHRABI M, et al. Characterization of biliary microbiota dysbiosis in extrahepatic cholangiocarcinoma[J]. PLoS One, 2021, 16( 3): e0247798. DOI: 10.1371/journal.pone.0247798. |
| [25] |
LIU XJ, CHENG Y, ZANG D, et al. The role of gut microbiota in lung cancer: From carcinogenesis to immunotherapy[J]. Front Oncol, 2021, 11: 720842. DOI: 10.3389/fonc.2021.720842. |
| [26] |
LI T, WANG PL, YUAN ZB, et al. Changes in intestinal flora in patients with extrahepatic cholangiocarcinoma[J]. J Clin Hepatol, 2021, 37( 12): 2883- 2889. DOI: 10.3969/j.issn.1001-5256.2021.12.029. |
| [27] |
HUANG H, ZHONG W, WANG XJ, et al. The role of gastric microecological dysbiosis in gastric carcinogenesis[J]. Front Microbiol, 2023, 14: 1218395. DOI: 10.3389/fmicb.2023.1218395. |
| [28] |
MADSEN C. The role of oral health in gastrointestinal malignancies[J]. J Gastrointest Oncol, 2021, 12( Suppl 2): S311- S315. DOI: 10.21037/jgo.2020.02.03. |
| [29] |
LIU TY, GUO ZX, SONG XL, et al. High-fat diet-induced dysbiosis mediates MCP-1/CCR2 axis-dependent M2 macrophage polarization and promotes intestinal adenoma-adenocarcinoma sequence[J]. J Cell Mol Med, 2020, 24( 4): 2648- 2662. DOI: 10.1111/jcmm.14984. |
| [30] |
FAN XY, JIN YL, CHEN G, et al. Gut microbiota dysbiosis drives the development of colorectal cancer[J]. Digestion, 2021, 102( 4): 508- 515. DOI: 10.1159/000508328. |
| [31] |
CUI H, LIAN J, XU BG, et al. Identification of a bile acid and bile salt metabolism-related lncRNA signature for predicting prognosis and treatment response in hepatocellular carcinoma[J]. Sci Rep, 2023, 13( 1): 19512. DOI: 10.1038/s41598-023-46805-6. |
| [32] |
CAMILLERI M. Bile acid detergency: Permeability, inflammation, and effects of sulfation[J]. Am J Physiol Gastrointest Liver Physiol, 2022, 322( 5): G480- G488. DOI: 10.1152/ajpgi.00011.2022. |
| [33] |
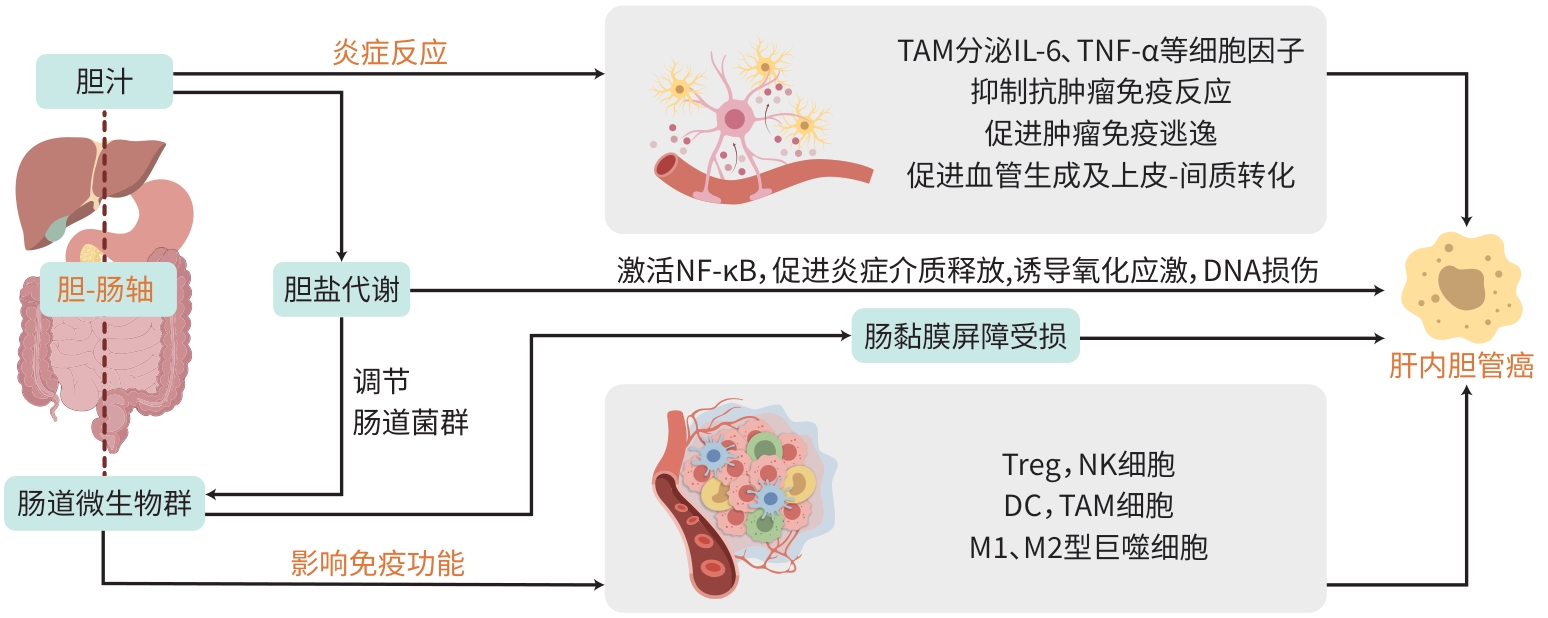
WANG N, YU XH, XU L. Intestinal flora and cholangiocarcinoma: Research progress[J]. Chin J Microecol, 2018, 30( 11): 1339- 1342. DOI: 10.13381/j.cnki.cjm.201811024. |
| [34] |
BRUNEAU A, HUNDERTMARK J, GUILLOT A, et al. Molecular and cellular mediators of the gut-liver axis in the progression of liver diseases[J]. Front Med(Lausanne), 2021, 8: 725390. DOI: 10.3389/fmed.2021.725390. |
| [35] |
WANG DH, ZHANG XS, DU HW. Inflammatory bowel disease: A potential pathogenic factor of Alzheimer’s disease[J]. Prog Neuropsychopharmacol Biol Psychiatry, 2022, 119: 110610. DOI: 10.1016/j.pnpbp.2022.110610. |
| [36] |
ZOU ZJ, LIN HF, LI MS, et al. Tumor-associated macrophage polarization in the inflammatory tumor microenvironment[J]. Front Oncol, 2023, 13: 1103149. DOI: 10.3389/fonc.2023.1103149. |
| [37] |
LI LH, YU R, CAI TG, et al. Effects of immune cells and cytokines on inflammation and immunosuppression in the tumor microenvironment[J]. Int Immunopharmacol, 2020, 88: 106939. DOI: 10.1016/j.intimp.2020.106939. |
| [38] |
SAHOO DK, BORCHERDING DC, CHANDRA L, et al. Differential transcriptomic profiles following stimulation with lipopolysaccharide in intestinal organoids from dogs with inflammatory bowel disease and intestinal mast cell tumor[J]. Cancers(Basel), 2022, 14( 14): 3525. DOI: 10.3390/cancers14143525. |
| [39] |
VIGNJEVIĆ PETRINOVIĆ S, MILOŠEVIĆ MS, MARKOVIĆ D, et al. Interplay between stress and cancer-a focus on inflammation[J]. Front Physiol, 2023, 14: 1119095. DOI: 10.3389/fphys.2023.1119095. |
| [40] |
AL-RAJABI R, SUN WJ. Immunotherapy in cholangiocarcinoma[J]. Curr Opin Gastroenterol, 2021, 37( 2): 105- 111. DOI: 10.1097/MOG.0000000000000715. |
| [41] |
WITSCHEN PM, CHAFFEE TS, BRADY NJ, et al. Tumor cell associated hyaluronan-CD44 signaling promotes pro-tumor inflammation in breast cancer[J]. Cancers(Basel), 2020, 12( 5): 1325. DOI: 10.3390/cancers12051325. |
| [42] |
TAN ZF, XUE HB, SUN YL, et al. The role of tumor inflammatory microenvironment in lung cancer[J]. Front Pharmacol, 2021, 12: 688625. DOI: 10.3389/fphar.2021.688625. |
| [43] |
LIU GL, DOU J, MENG HJ, et al. Value of immune-inflammatory factors in predicting intrahepatic cholangiocarcinoma[J]. J Clin Hepatol, 2023, 39( 9): 2231- 2236. DOI: 10.3969/j.issn.1001-5256.2023.09.030. |
| [44] |
SCIMECA M, ROVELLA V, PALUMBO V, et al. Programmed cell death pathways in cholangiocarcinoma: Opportunities for targeted therapy[J]. Cancers(Basel), 2023, 15( 14): 3638. DOI: 10.3390/cancers15143638. |
| [45] |
CHEN S, WANG J. Advances in tumor microenvironment and immunotherapy of Cholangiocarcinoma[J]. J Clin Hepatol, 2022, 38( 10): 2428- 2432. DOI: 10.3969/j.issn.1001-5256.2022.10.044. |
| [46] |
XIA T, LI KY, NIU N, et al. Immune cell atlas of cholangiocarcinomas reveals distinct tumor microenvironments and associated prognoses[J]. J Hematol Oncol, 2022, 15( 1): 37. DOI: 10.1186/s13045-022-01253-z. |
| [47] |
ALVISI G, TERMANINI A, SOLDANI C, et al. Multimodal single-cell profiling of intrahepatic cholangiocarcinoma defines hyperactivated Tregs as a potential therapeutic target[J]. J Hepatol, 2022, 77( 5): 1359- 1372. DOI: 10.1016/j.jhep.2022.05.043. |
| [48] |
ZHANG ZJ, HUANG YP, LIU ZT, et al. Identification of immune related gene signature for predicting prognosis of cholangiocarcinoma patients[J]. Front Immunol, 2023, 14: 1028404. DOI: 10.3389/fimmu.2023.1028404. |
| [49] |
ZHOU GY, LIESHOUT R, van TIENDEREN GS, et al. Modelling immune cytotoxicity for cholangiocarcinoma with tumour-derived organoids and effector T cells[J]. Br J Cancer, 2022, 127( 4): 649- 660. DOI: 10.1038/s41416-022-01839-x. |
| [50] |
GRETEN TF, SCHWABE R, BARDEESY N, et al. Immunology and immunotherapy of cholangiocarcinoma[J]. Nat Rev Gastroenterol Hepatol, 2023, 20( 6): 349- 365. DOI: 10.1038/s41575-022-00741-4. |
| [51] |
CAZZETTA V, FRANZESE S, CARENZA C, et al. Natural killer-dendritic cell interactions in liver cancer: Implications for immunotherapy[J]. Cancers(Basel), 2021, 13( 9): 2184. DOI: 10.3390/cancers13092184. |
| [52] |
CHEN ZM, CHEN JH. Advances in precision diagnosis and treatment of cholangiocarcinoma[J]. Chin J Clin Pharmacol Ther, 2025, 30( 2): 159- 170. DOI: 10.12092/j.issn.1009-2501.2025.02.002. |
| [53] |
YU XZ, ZHU LL, WANG T, et al. Immune microenvironment of cholangiocarcinoma: Biological concepts and treatment strategies[J]. Front Immunol, 2023, 14: 1037945. DOI: 10.3389/fimmu.2023.1037945. |
| [54] |
CHIANG NJ, HOU YC, TAN KT, et al. The immune microenvironment features and response to immunotherapy in EBV-associated lymphoepithelioma-like cholangiocarcinoma[J]. Hepatol Int, 2022, 16( 5): 1137- 1149. DOI: 10.1007/s12072-022-10346-3. |
| [55] |
KIDA A, MIZUKOSHI E, KITAHARA M, et al. Effects of adoptive T-cell immunotherapy on immune cell profiles and prognosis of patients with unresectable or recurrent cholangiocarcinoma[J]. Int J Cancer, 2024, 154( 4): 738- 747. DOI: 10.1002/ijc.34716. |






 DownLoad:
DownLoad: