| [1] |
ROBERTS SE, MORRISON-REES S, JOHN A, et al. The incidence and aetiology of acute pancreatitis across Europe[J]. Pancreatology, 2017, 17( 2): 155- 165. DOI: 10.1016/j.pan.2017.01.005. |
| [2] |
LIN HH, CHANG HY, CHIANG YT, et al. Smoking, drinking, and pancreatitis: A population-based cohort study in Taiwan[J]. Pancreas, 2014, 43( 7): 1117- 1122. DOI: 10.1097/MPA.0000000000000209. |
| [3] |
GRAJALES-FIGUEROA G, DÍAZ HERNÁNDEZ HA, CHACÓN PORTILLO MA, et al. Increased mortality from extrapancreatic infections in hospitalized patients with acute pancreatitis[J]. Gastroenterol Res Pract, 2019, 2019: 2789764. DOI: 10.1155/2019/2789764. |
| [4] |
JIN JL, SUN D, CAO YX, et al. Intensive genetic analysis for Chinese patients with very high triglyceride levels: Relations of mutations to triglyceride levels and acute pancreatitis[J]. EBioMedicine, 2018, 38: 171- 177. DOI: 10.1016/j.ebiom.2018.11.001. |
| [5] |
REID GP, WILLIAMS EW, FRANCIS DK, et al. Acute pancreatitis: A 7 year retrospective cohort study of the epidemiology, aetiology and outcome from a tertiary hospital in Jamaica[J]. Ann Med Surg(Lond), 2017, 20: 103- 108. DOI: 10.1016/j.amsu.2017.07.014. |
| [6] |
HONG WD, ZIMMER V, BASHARAT Z, et al. Association of total cholesterol with severe acute pancreatitis: A U-shaped relationship[J]. Clin Nutr, 2020, 39( 1): 250- 257. DOI: 10.1016/j.clnu.2019.01.022. |
| [7] |
Expert group of emergency expert consensus on diagnosis and treatment of hypertriglyceridemic acute pancreatitis. Emergency expert consensus on diagnosis and treatment of hypertriglyceridemic acute pancreatitis[J]. Chin Gen Pract, 2021, 24( 30): 3781- 3793. DOI: 10.12114/j.issn.1007-9572.2021.02.028. |
| [8] |
TENNER S, BAILLIE J, DEWITT J, et al. American college of gastroenterology guideline: Management of acute pancreatitis[J]. Am J Gastroenterol, 2013, 108( 9): 1400- 1415. DOI: 10.1038/ajg.2013.218. |
| [9] |
BERGLUND L, BRUNZELL JD, GOLDBERG AC, et al. Evaluation and treatment of hypertriglyceridemia: An endocrine society clinical practice guideline[J]. J Clin Endocrinol Metab, 2012, 97( 9): 2969- 2989. DOI: 10.1210/jc.2011-3213. |
| [10] |
JI RG, ZHU GL, ZHANG B, et al. Association between dyslipidemia and acute pancreatitis: A prospective cohort study[J]. J Clin Hepatol, 2019, 35( 7): 1536- 1540. DOI: 10.3969/j.issn.1001-5256.2019.07.023. |
| [11] |
WANG GD, SONG L, ZHAO HL, et al. Predictive value of cumulative blood pressure exposure to stroke events[J]. Chin J Hypertens, 2017, 25( 8): 773- 778. DOI: 10.16439/j.cnki.1673-7245.2017.08.026. |
| [12] |
WANG JR, HU YQ, SHI HJ, et al. Study on the assiociation between cumulative uric acid and brachial-ankle pulse velocity[J]. Chin J Rheumatol, 2019, 4( 23): 220- 227. DOI: 10.3760/cma.j.issn.1007-7480.2019.04.002. |
| [13] |
WU SL, HUANG ZR, YANG XC, et al. Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a northern Chinese industrial city[J]. Circ Cardiovasc Qual Outcomes, 2012, 5( 4): 487- 493. DOI: 10.1161/CIRCOUTCOMES.111.963694. |
| [14] |
ZHU GL, CHEN SH, FAN XD, et al. A prospective cohort study on BMI levels and risk of acute pancreatitis[J]. Chin J Epidemiol, 2021, 42( 12): 2131- 2137. DOI: 10.3760/cma.j.cn112338-20201027-01286. |
| [15] |
ZHANG B, ZHU GL, SUN Q, et al. Baseline fasting glucose and risk of acute pancreatitis: A prospective cohort study[J]. Chin Gen Pract, 2021, 24( 1): 60- 64. DOI: 10.12114/j.issn.1007-9572.2020.00.602. |
| [16] |
Writing Group of 2018 Chinese Guidelines for the Management of Hypertension, Chinese Hypertension League, Chinese Society of Cardiology, et al. Chinese guidelines for the management of hypertension(2018 revised edition)[J]. Chin J Cardiovasc Med, 2019, 24( 1): 24- 56. DOI: 10.3969/j.issn.1007-5410.2019.01.002. |
| [17] |
Chinese Diabetes Society. Guidelines for the prevention and control of type 2 diabetes in China(2017 Edition)[J]. Chin J Pract Intern Med, 2018, 38( 4): 292- 344. DOI: 10.19538/j.nk2018040108. |
| [18] |
Pancreas Study Group, Chinese Society of Gastroenterology, Chinese Medical Association; Editorial Board of Chinese Journal of Pancreatology; Editorial Board of Chinese Journal of Digestion. Chinese guidelines for the management of acute pancreatitis(Shenyang, 2019)[J]. J Clin Hepatol, 2019, 35( 12): 2706- 2711. DOI: 10.3969/j.issn.1001-5256.2019.12.013. |
| [19] |
SU W, GUO F. Triglyceride-controlling during acute phase of hypertriglyceridemia induced pancreatitis[J]. Chin J Dig Surg, 2023, 22( 1): 89- 93. DOI: 10.3760/cma.j.cn115610-20221220-00755. |
| [20] |
WU YQ, ZHAO JC. Predictive value of Ranson score in the classification of moderate to severe hyperlipidemia acute pancreatitis[J]. J Clin Exp Med, 2022, 21( 2): 222- 225. DOI: 10.3969/j.issn.1671-4695.2022.02.029. |
| [21] |
Joint committee for guideline revision. 2016 Chinese guidelines for the management of dyslipidemia in adults[J]. J Geriatr Cardiol, 2018, 15( 1): 1- 29. DOI: 10.11909/j.issn.1671-5411.2018.01.011. |
| [22] |
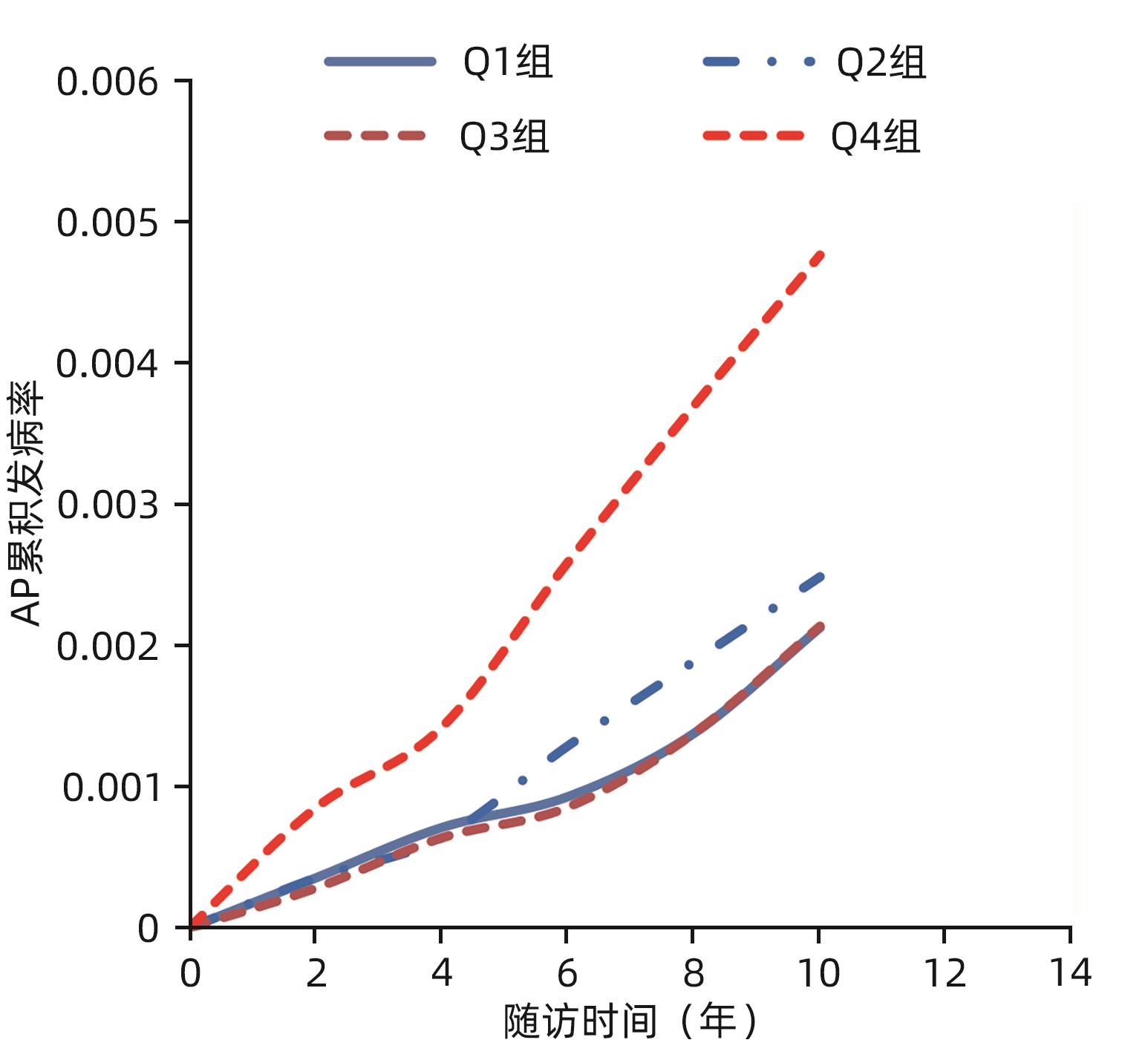
ZHU GL, ZHANG B, JI RG, et al. A prospective cohort study on triglycerides levels and risk of acute pancreatitis[J]. Chin J Dig, 2018, 38( 12): 829- 834. DOI: 10.3760/cma.j.issn.0254-1432.2018.12.008. |
| [23] |
LINDKVIST B, APPELROS S, REGNÉR S, et al. A prospective cohort study on risk of acute pancreatitis related to serum triglycerides, cholesterol and fasting glucose[J]. Pancreatology, 2012, 12( 4): 317- 324. DOI: 10.1016/j.pan.2012.05.002. |
| [24] |
PEDERSEN SB, LANGSTED A, NORDESTGAARD BG. Nonfasting mild-to-moderate hypertriglyceridemia and risk of acute pancreatitis[J]. JAMA Intern Med, 2016, 176( 12): 1834- 1842. DOI: 10.1001/jamainternmed.2016.6875. |
| [25] |
EWALD N, HARDT PD, KLOER HU. Severe hypertriglyceridemia and pancreatitis: Presentation and management[J]. Curr Opin Lipidol, 2009, 20( 6): 497- 504. DOI: 10.1097/MOL.0b013e3283319a1d. |
| [26] |
GERASIMENKO JV, GERASIMENKO OV, PETERSEN OH. The role of Ca 2+ in the pathophysiology of pancreatitis[J]. J Physiol, 2014, 592( 2): 269- 280. DOI: 10.1113/jphysiol.2013.261784. |
| [27] |
ZHANG XL, LI F, CUI YQ, et al. The role of oxide stress during the pathogenesis of chronic pancreatic injuries induced by chronic high-fat diets in rat[J]. Chin J Surg, 2012, 50( 7): 646- 649. DOI: 10.3760/cma.j.issn.0529-5815.2012.07.019. |
| [28] |
VALDIVIELSO P, RAMIREZ-BUENO A, EWALD N. Current knowledge of hypertriglyceridemic pancreatitis[J]. Eur J Intern Med, 2014, 25( 8): 689- 694. DOI: 10.1016/j.ejim.2014.08.008. |
| [29] |
RAWLA P, SUNKARA T, THANDRA KC, et al. Hypertriglyceridemia-induced pancreatitis: updated review of current treatment and preventive strategies[J]. Clin J Gastroenterol, 2018, 11( 6): 441- 448. DOI: 10.1007/s12328-018-0881-1. |
| [30] |
Joint Committee on the Chinese Guidelines for Lipid Management. Chinese guidelines for lipid management(2023)[J]. Chin J Cardiol, 2023, 51( 3): 221- 255. DOI: 10.3760/cma.j.cn112148-20230119-00038. |






 DownLoad:
DownLoad: