早期积极液体复苏与常规液体复苏治疗急性胰腺炎效果及安全性的Meta分析
DOI: 10.3969/j.issn.1001-5256.2023.09.019
Efficacy and safety of aggressive fluid resuscitation versus conventional fluid resuscitation in early treatment of acute pancreatitis: A Meta-analysis
-
摘要:
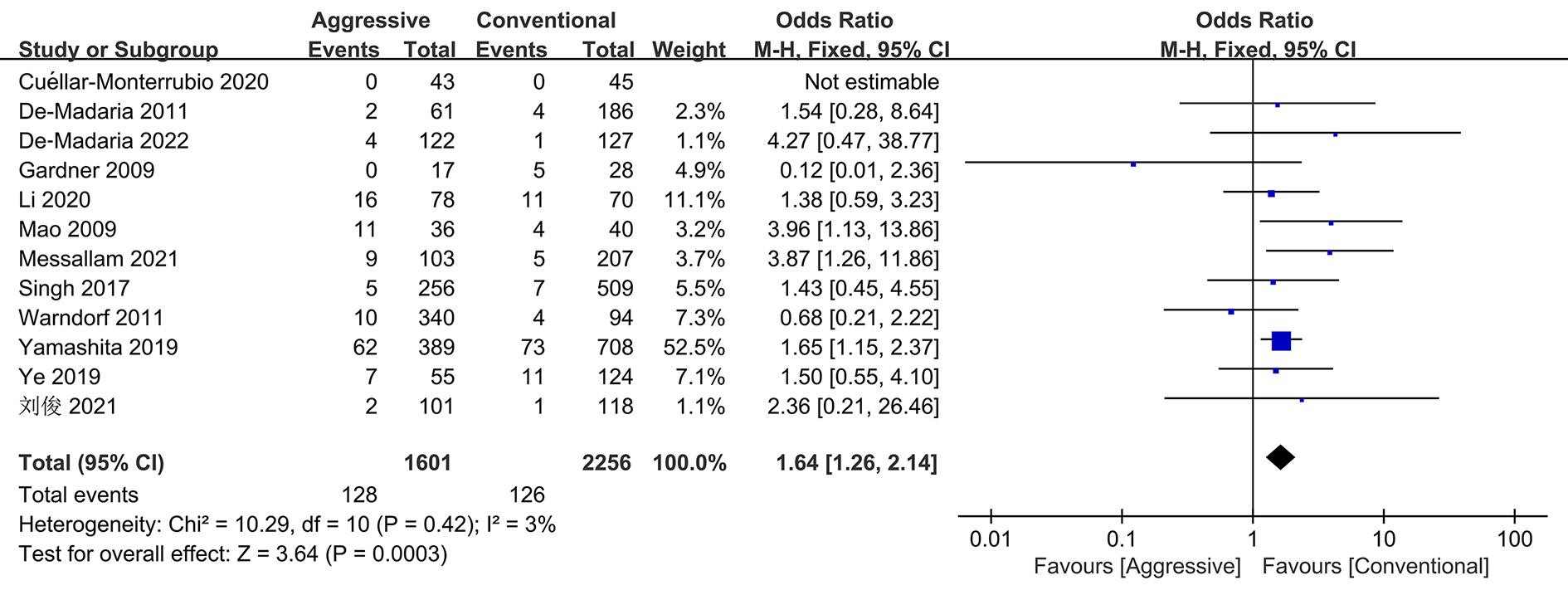
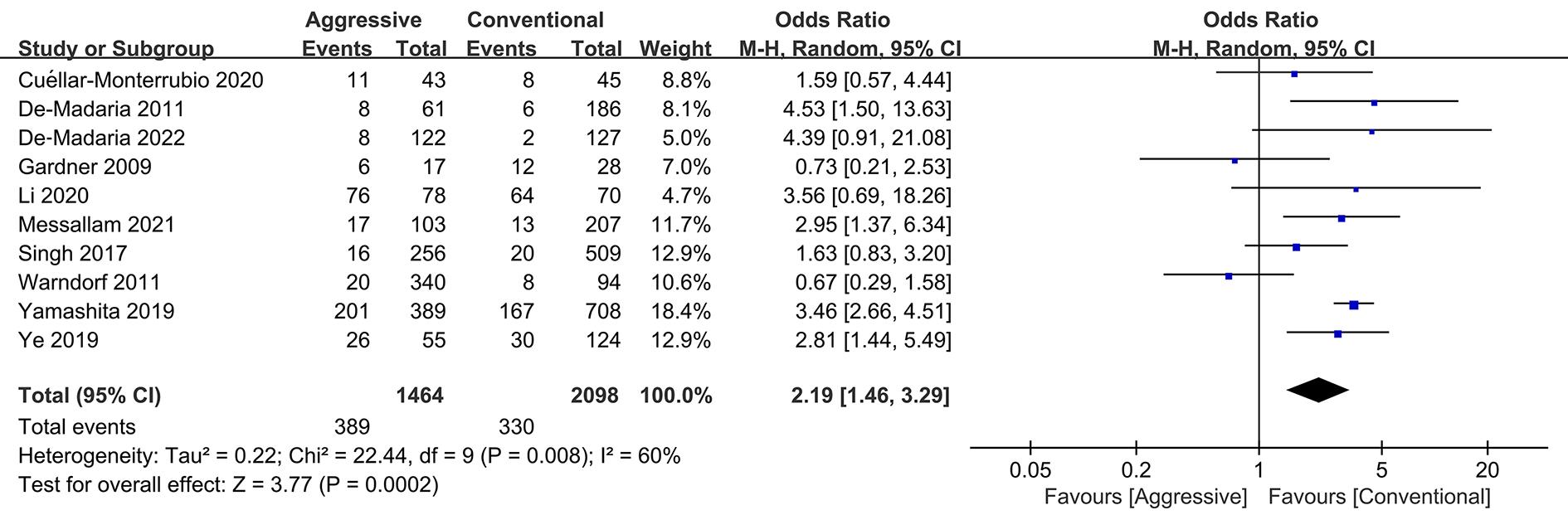
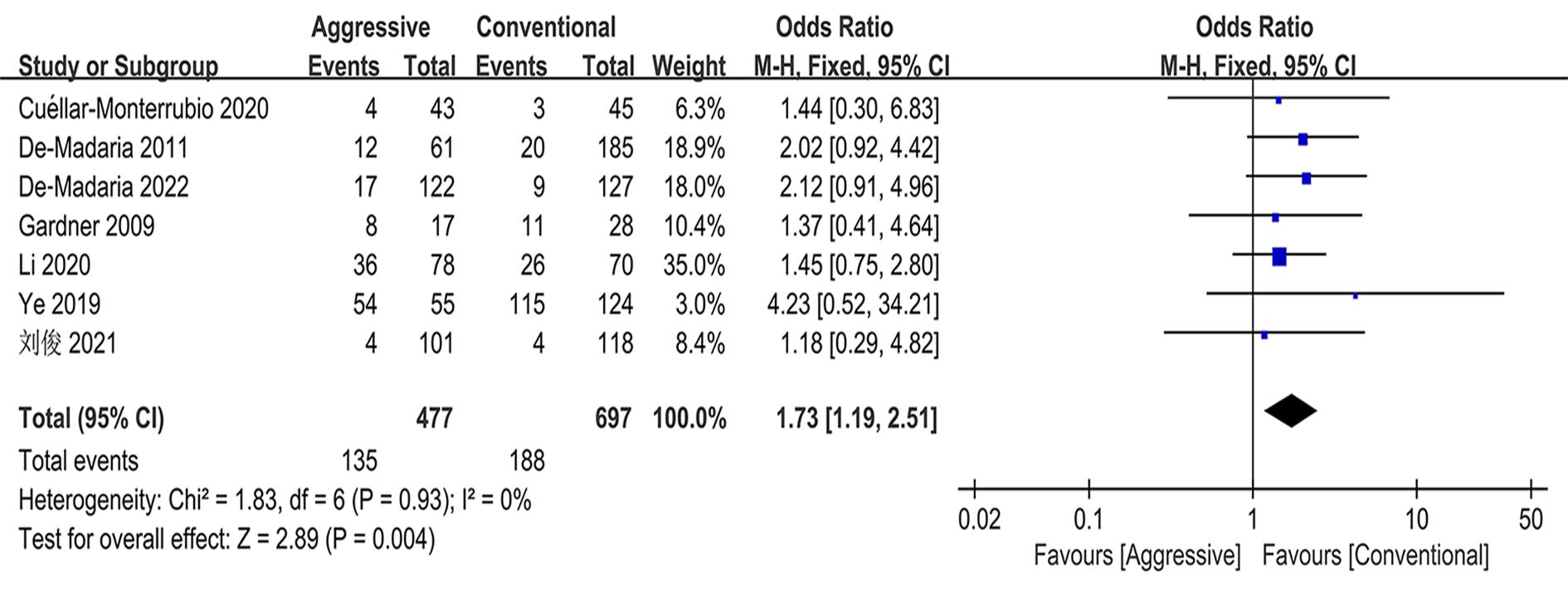
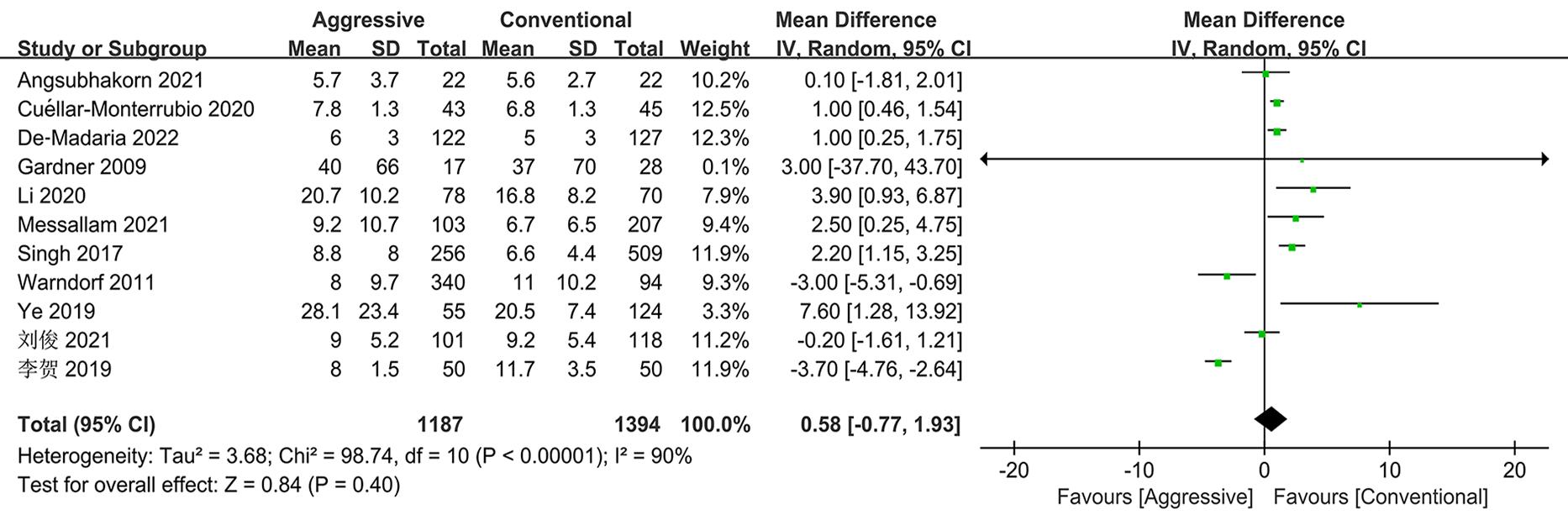
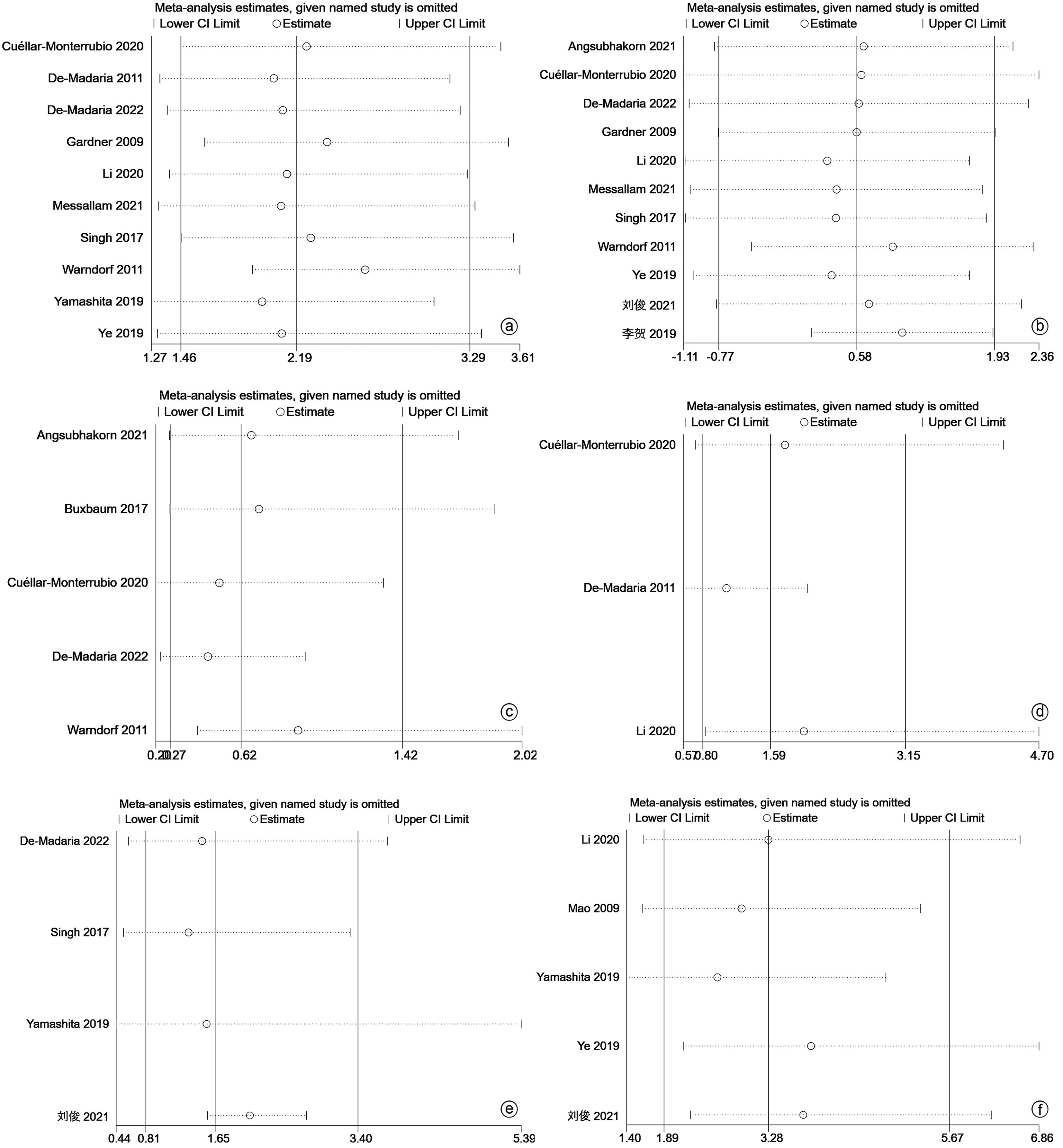
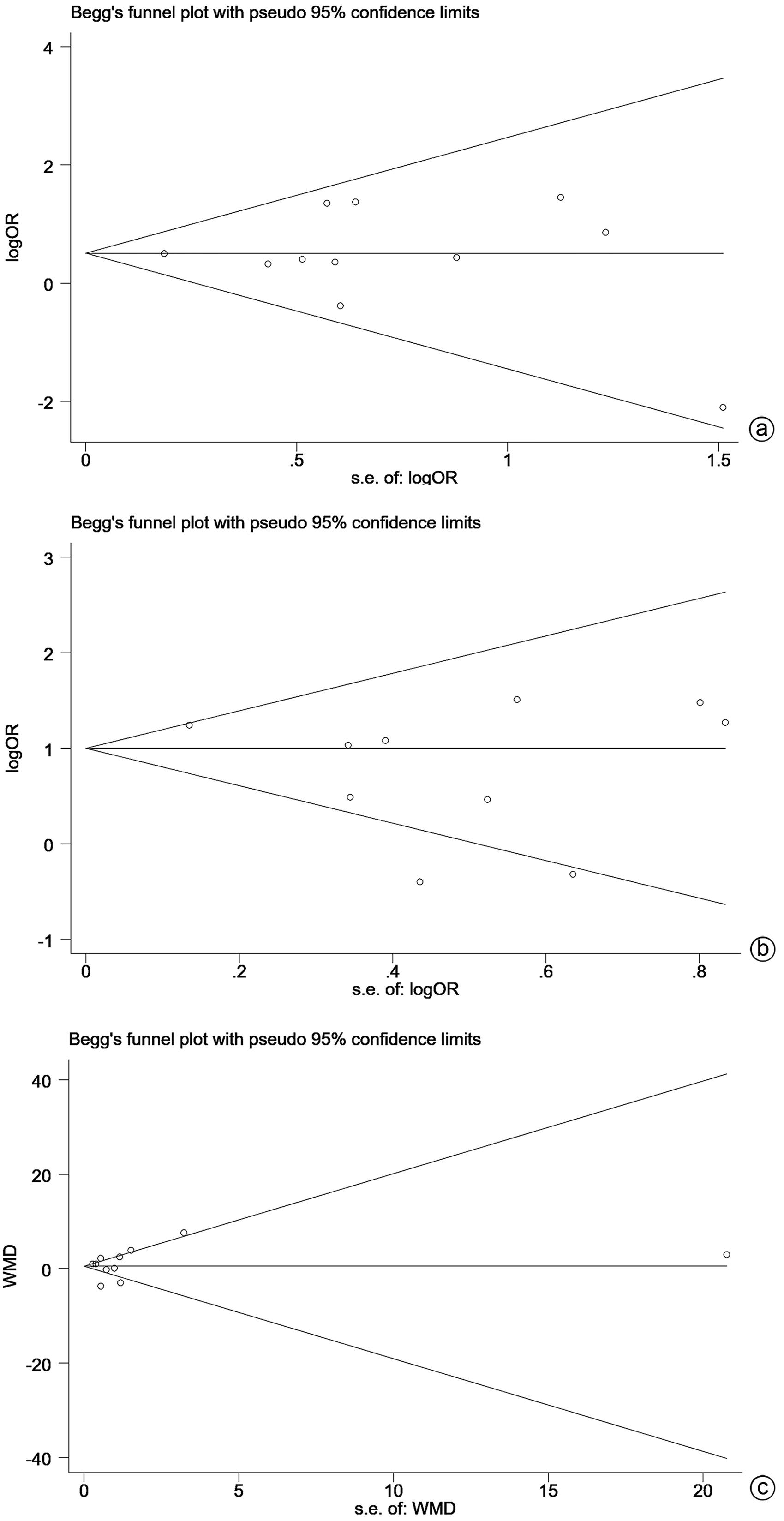
目的 本研究旨在系统评价积极液体复苏与常规液体复苏在急性胰腺炎(AP)早期治疗过程中的效果与安全性,为临床研究与实践提供参考。 方法 本研究根据 PRISMA 指南完成,PROSPERO注册号:CRD42023455046。计算机检索PubMed、Cochrane Library、Web of Science、中国知网、维普和万方数据库等中英文期刊服务平台,从建库至2022年11月30日发表的有关液体复苏治疗AP临床效果的随机对照试验与队列研究。采用RevMan 5.4软件和Stata 17.0软件进行Meta分析。 结果 最终纳入15项研究,共4 061例AP患者。Meta分析结果显示,与常规液体复苏组相比,积极液体复苏组的持续器官功能衰竭发生率(OR=2.19,95%CI:1.46~3.29,P<0.001)、胰腺坏死发生率(OR=1.73,95%CI:1.19~2.51,P=0.004)、死亡率(OR=1.64,95%CI:1.26~2.14,P<0.001)显著升高,同时还增加了感染性胰腺坏死(OR=1.82,95%CI:1.33~2.48,P<0.001)、循环功能衰竭(OR=6.31,95%CI:1.81~21.93,P=0.004)、呼吸功能衰竭(OR=3.81,95%CI=1.77~8.19,P<0.001)、肾功能衰竭(OR=1.88,95%CI:1.11~3.19,P=0.020)、腹腔间隔室综合征(OR=6.01,95%CI:2.45~14.71,P<0.001)、液体过负荷(OR=3.83,95%CI:1.65~8.88,P=0.002)的发生风险。 结论 积极液体复苏在AP早期治疗阶段表现出较差的效果及安全性,可能不利于患者预后。但受纳入研究数量和质量的限制,未来需要更多的多中心大样本随机对照试验来验证。 Abstract:Objective To systematically evaluate the efficacy and safety of aggressive fluid resuscitation versus conventional fluid resuscitation in the early treatment of acute pancreatitis (AP), and to provide a reference for clinical research and practice. Methods This study was conducted according to PRISMA guidelines, with a PROSPERO registration number of CRD42023455046. Chinese and English databases such as PubMed, the Cochrane Library, Web of Science, CNKI, VIP, and Wanfang Data were searched for randomized controlled trials and cohort studies on the clinical efficacy of aggressive fluid resuscitation versus conventional fluid resuscitation in the treatment of AP published up to November 30, 2022. RevMan 5.4 and Stata 17.0 were used to perform the meta-analysis. Results A total of 15 studies were included, with 4 061 patients in total. The meta-analysis showed that compared with the conventional fluid resuscitation group, the aggressive fluid resuscitation group had significantly higher incidence rate of persistent organ failure (odds ratio [OR]=2.19, 95% confidence interval [CI]: 1.46-3.29, P<0.001), incidence rate of pancreatic necrosis (OR=1.73, 95%CI: 1.19-2.51, P=0.004), and mortality rate (OR=1.64, 95%CI: 1.26-2.14, P<0.001), as well as significantly higher risks of infectious pancreatic necrosis (OR=1.82, 95%CI: 1.33-2.48, P<0.001), circulatory failure (OR=6.31, 95%CI: 1.81-21.93, P=0.004), respiratory failure (OR=3.81, 95%CI: 1.77-8.19, P<0.001), renal failure (OR=1.88, 95%CI: 1.11-3.19, P=0.02), abdominal compartment syndrome (OR=6.01, 95%CI: 2.45-14.71, P<0.001), and fluid overload (OR=3.83, 95%CI: 1.65-8.88, P=0.002). Conclusion Aggressive fluid resuscitation shows poor efficacy and safety in the early treatment of AP and may be unfavorable to the prognosis of patients. Due to the limited quantity and quality of studies included, more large multicenter randomized controlled trials are needed for verification in the future. -
Key words:
- Pancreatitis /
- Fluid Resuscitation /
- Treatment Outcome /
- Meta-Analysis
-
表 1 纳入研究的基本特征
Table 1. General characteristics of the included studies
第一作者 年份 国家 研究类型 积极组/常规组(例) 分组标准 (入院24 h内补液速率或总量) AP严重程度 年龄(积极组/常规组,岁) 结局指标 积极液体复苏 常规液体复苏 De-Madaria[10] 2022 印度、意大利、墨西哥、西班牙 RCT 122/127 20 mL/kg+ 3 mL·kg-1·h-1 1.5 mL·kg-1·h-1 MAP 56±18/57±17 a、b、c、d、e、g、h、i、k、n、o Messallam[18] 2021 美国 队列研究 103/207 ≥4.475 L <4.475 L MAP 43.7±13.6/48.2±14.0 a、b、d 刘俊[19] 2021 中国 队列研究 101/118 ≥3.2 L <3.2 L MAP 46.3±14.2/46.9±13.4 a、c、d、h、j Angsubhakorn[20] 2021 泰国 RCT 22/22 20 mL/kg+ 3 mL·kg-1·h-1 10 mL/kg+ 1.5 mL·kg-1·h-1 MAP 46.4±15.0/45.0±15.0 d、e Cuéllar-Monterrubio[21] 2020 墨西哥 RCT 43/45 20 mL/kg+ 3 mL·kg-1·h-1 1.5 mL·kg-1·h-1 MAP 36.7±16.0/38.6±15.1 a、b、c、d、e、f Li[22] 2020 中国 队列研究 78/70 ≥3 mL·kg-1·h-1 <3 mL·kg-1·h-1 SAP 45.0±10.2/47.3±9.2 a、b、c、d、f、i、j、k、o 李贺[23] 2019 中国 RCT 50/50 20 mL/kg+ 3 mL·kg-1·h-1 10 mL/kg+ 1.5 mL·kg-1·h-1 MAP 44.3±10.3/46.2±12.5 d Ye[13] 2019 中国 队列研究 55/124 ≥4 L <4 L SAP 44.6±11.4/47.0±12.5 a、b、c、d、g、j、k、l、m Yamashita[24] 2019 日本 队列研究 389/708 ≥6 L <6 L SAP 55.5±16.5/60.4±17.8 a、b、g、h、j、l Buxbaum[25] 2017 美国 RCT 27/33 20 mL/kg+ 3 mL·kg-1·h-1 10 mL/kg+1.5 mL·kg-1·h-1 MAP 44.4±13.7/45.3±12.3 e Singh[6] 2017 美国、西班牙 队列研究 256/509 ≥4.3 L <4.3 L MAP 49.5±17.3/54.7±19.7 a、b、d、h De-Madaria[9] 2011 西班牙 队列研究 61/186 ≥4.1 L <4.1 L MAP 56.0±20.0/64.6±19.8 a、b、c、f、i、k Warndorf[26] 2011 美国 队列研究 340/94 ≥入院72 h补液总量的1/3 <入院72 h补液总量的1/3 MAP 54±20/49±22 a、b、d、e Mao[11] 2009 中国 RCT 36/40 10~15 mL·kg-1·h-1 5~10 mL·kg-1·h-1 SAP 51.3±14.3/50.2±12.0 a、j、m Gardner[27] 2009 美国 队列研究 17/28 ≥入院72 h补液总量的1/3 <入院72 h补液总量的1/3 SAP 53±13/57±17 a、b、c、d 注:a,死亡率;b,POF;c,胰腺坏死;d,住院时间;e,持续性SIRS;f,急性胰周液体积聚;g,感染性胰腺坏死;h,侵入性治疗;i,呼吸功能衰竭;j,机械通气;k,肾功能衰竭;l,持续性肾脏替代治疗;m,ACS;n,液体过负荷;o,循环功能衰竭。 表 2 纳入队列研究的质量评估
Table 2. Quality evaluation of the included cohorts
第一作者 对象的选择 可比性 结局评估 NOS评分 暴露组代表性 非暴露组代表性 暴露因素确定方法 确定结局指标 基于设计所得队列的可比性 评价是否充分 随访是否充分 随访完整性 Messallam[18] 1 1 1 1 1 1 1 0 7 刘俊[19] 1 1 1 1 2 1 1 0 8 Li[22] 1 1 1 1 2 1 1 0 8 Ye[13] 1 1 1 1 2 1 1 0 8 Yamashita[24] 1 1 1 1 0 1 1 1 7 Singh[6] 1 1 1 1 2 1 1 1 9 De-Madaria[9] 1 1 1 1 1 1 1 1 8 Warndorf[26] 1 1 1 1 1 1 1 0 7 Gardner[27] 1 1 1 1 1 1 1 0 7 表 3 纳入RCT的质量评估
Table 3. Quality evaluation of the included RCTs
表 4 液体复苏方式与其他结局指标关系的Meta分析
Table 4. Meta-analysis of relationship between resuscitation and other outcomes
结局指标 纳入研究数量 积极组/常规组(例) 异质性检验 效应模型 OR(95%CI) P值 I2值 P值 持续性SIRS 5 528/298 62% 0.03 随机 0.62(0.27~1.42) 0.260 急性胰周液体积聚 3 182/301 54% 0.11 随机 1.59(0.80~3.15) 0.190 感染性胰腺坏死 3 566/959 0% 0.82 固定 1.82(1.33~2.48) <0.001 循环功能衰竭 2 200/197 0% 0.86 固定 6.31(1.81~21.93) 0.004 呼吸功能衰竭 3 261/383 0% 0.93 固定 3.81(1.77~8.19) <0.001 肾功能衰竭 4 316/507 0% 0.51 固定 1.88(1.11~3.19) 0.020 侵入性治疗 4 868/1 462 73% 0.01 随机 1.65(0.81~3.40) 0.170 机械通气 5 659/1 060 56% 0.06 随机 3.28(1.89~5.67) <0.001 持续性肾脏替代治疗 2 444/832 0% 0.63 固定 2.34(1.73~3.16) <0.001 ACS 2 91/164 0% 0.64 固定 6.01(2.45~14.71) <0.001 液体过负荷 1 122/127 固定 3.83(1.65~8.88) 0.002 表 5 亚组分析
Table 5. Subgroup analysis
亚组 纳入研究数量 异质性检验 效应模型 OR(95%CI) P值 I2值 P值 POF 研究类型 RCT 2 12% 0.290 随机 2.21(0.87~5.62) 0.100 队列研究 8 67% 0.004 随机 2.16(1.36~3.42) 0.001 病情严重程度 MAP 6 53% 0.060 随机 1.97(1.12~3.45) 0.020 SAP 4 50% 0.110 随机 2.63(1.54~4.50) <0.001 年龄 年老组(>50岁) 6 76% <0.001 随机 1.93(0.99~3.78) 0.053 年轻组(≤50岁) 4 0% 0.760 随机 2.62(1.69~4.05) <0.001 住院时间 研究类型 RCT 4 95% <0.001 随机 -0.39(-2.46~1.69) 0.710 队列研究 7 79% <0.001 随机 1.47(-0.50~3.44) 0.140 病情严重程度 MAP 8 92% <0.001 随机 0.02(-1.38~1.41) 0.980 SAP 3 0% 0.58 随机 4.56(1.88~7.24) <0.001 年龄 年老组(>50岁) 4 82% <0.001 随机 0.42(-1.50~2.33) 0.670 年轻组(≤50岁) 7 92% <0.001 随机 0.89(-1.13~2.91) 0.390 -
[1] BOXHOORN L, VOERMANS RP, BOUWENSE SA, et al. Acute pancreatitis[J]. Lancet, 2020, 396( 10252): 726- 734. DOI: 10.1016/S0140-6736(20)31310-6. [2] Chinese Society for Emergency Medicine; Beijing-Tianjin-Hebei Alliance of Emergency Treatment and First Aid; Emergency Medicine Branch, Beijing Medical Association, et al. Expert consensus on emergency diagnosis and treatment of acute pancreatitis[J]. J Clin Hepatol, 2021, 37( 5): 1034- 1041. DOI: 10.3969/j.issn.1001-5256.2021.05.012.中华医学会急诊分会, 京津冀急诊急救联盟, 北京医学会急诊分会, 等. 急性胰腺炎急诊诊断及治疗专家共识[J]. 临床肝胆病杂志, 2021, 37( 5): 1034- 1041. DOI: 10.3969/j.issn.1001-5256.2021.05.012. [3] MEDEROS MA, REBER HA, GIRGIS MD. Acute pancreatitis: A review[J]. JAMA, 2021, 325( 4): 382- 390. DOI: 10.1001/jama.2020.20317. [4] SZATMARY P, GRAMMATIKOPOULOS T, CAI W, et al. Acute pancreatitis: Diagnosis and treatment[J]. Drugs, 2022, 82( 12): 1251- 1276. DOI: 10.1007/s40265-022-01766-4. [5] SARR MG. Early fluid“resuscitation/therapy” in acute pancreatitis: which fluid? What rate? What parameters to gauge effectiveness?[J]. Ann Surg, 2013, 257( 2): 189- 190. DOI: 10.1097/SLA.0b013e318280e19e. [6] SINGH VK, GARDNER TB, PAPACHRISTOU GI, et al. An international multicenter study of early intravenous fluid administration and outcome in acute pancreatitis[J]. United European Gastroenterol J, 2017, 5( 4): 491- 498. DOI: 10.1177/2050640616671077. [7] GARDNER TB, VEGE SS, PEARSON RK, et al. Fluid resuscitation in acute pancreatitis[J]. Clin Gastroenterol Hepatol, 2008, 6( 10): 1070- 1076. DOI: 10.1016/j.cgh.2008.05.005. [8] WEITZ G, WOITALLA J, WELLHÖNER P, et al. Detrimental effect of high volume fluid administration in acute pancreatitis-a retrospective analysis of 391 patients[J]. Pancreatology, 2014, 14( 6): 478- 483. DOI: 10.1016/j.pan.2014.07.016. [9] DE-MADARIA E, SOLER-SALA G, SÁNCHEZ-PAYÁ J, et al. Influence of fluid therapy on the prognosis of acute pancreatitis: a prospective cohort study[J]. Am J Gastroenterol, 2011, 106( 10): 1843- 1850. DOI: 10.1038/ajg.2011.236. [10] DE-MADARIA E, BUXBAUM JL, MAISONNEUVE P, et al. Aggressive or moderate fluid resuscitation in acute pancreatitis[J]. N Engl J Med, 2022, 387( 11): 989- 1000. DOI: 10.1056/NEJMoa2202884. [11] MAO EQ, TANG YQ, FEI J, et al. Fluid therapy for severe acute pancreatitis in acute response stage[J]. Chin Med J(Engl), 2009, 122( 2): 169- 173. [12] BANKS PA, BOLLEN TL, DERVENIS C, et al. Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus[J]. Gut, 2013, 62( 1): 102- 111. DOI: 10.1136/gutjnl-2012-302779. [13] YE B, MAO W, CHEN Y, et al. Aggressive resuscitation is associated with the development of acute kidney injury in acute pancreatitis[J]. Dig Dis Sci, 2019, 64( 2): 544- 552. DOI: 10.1007/s10620-018-5328-5. [14] STANG A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses[J]. Eur J Epidemiol, 2010, 25( 9): 603- 605. DOI: 10.1007/s10654-010-9491-z. [15] JADAD AR, MOORE RA, CARROLL D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary?[J]. Control Clin Trials, 1996, 17( 1): 1- 12. DOI: 10.1016/0197-2456(95)00134-4. [16] MCGRATH S, ZHAO X, STEELE R, et al. Estimating the sample mean and standard deviation from commonly reported quantiles in meta-analysis[J]. Stat Methods Med Res, 2020, 29( 9): 2520- 2537. DOI: 10.1177/0962280219889080. [17] BARILI F, PAROLARI A, KAPPETEIN PA, et al. Statistical Primer: heterogeneity, random- or fixed-effects model analyses?[J]. Interact Cardiovasc Thorac Surg, 2018, 27( 3): 317- 321. DOI: 10.1093/icvts/ivy163. [18] MESSALLAM AA, BODY CB, BERGER S, et al. Impact of early aggressive fluid resuscitation in acute pancreatitis[J]. Pancreatology, 2021, 21( 1): 69- 73. DOI: 10.1016/j.pan.2020.11.006. [19] LIU J, WU PY, LIU L, et al. Impact of early active fluid resuscitation on patients initially assessed as non-severe acute pancreatitis[J]. Chin Gen Pract, 2021, 24( 27): 3457- 3463. DOI: 10.12114/j.issn.1007-9572.2021.00.454.刘俊, 武鹏宇, 刘莉, 等. 早期积极液体复苏对初始评估未达到重型标准的急性胰腺炎患者的影响研究[J]. 中国全科医学, 2021, 24( 27): 3457- 3463. DOI: 10.12114/j.issn.1007-9572.2021.00.454. [20] ANGSUBHAKORN A, TIPCHAICHATTA K, CHIRAPONGSATHORN S. Comparison of aggressive versus standard intravenous hydration for clinical improvement among patients with mild acute pancreatitis: A randomized controlled trial[J]. Pancreatology, 2021, 21( 7): 1224- 1230. DOI: 10.1016/j.pan.2021.06.004. [21] CUÉLLAR-MONTERRUBIO JE, MONREAL-ROBLES R, GONZÁLEZ-MORENO EI, et al. Nonaggressive versus aggressive intravenous fluid therapy in acute pancreatitis with more than 24 hours from disease onset: A randomized controlled trial[J]. Pancreas, 2020, 49( 4): 579- 583. DOI: 10.1097/MPA.0000000000001528. [22] LI L, JIN T, WEN S, et al. Early rapid fluid therapy is associated with increased rate of noninvasive positive-pressure ventilation in hemoconcentrated patients with severe acute pancreatitis[J]. Dig Dis Sci, 2020, 65( 9): 2700- 2711. DOI: 10.1007/s10620-019-05985-w. [23] LI H, GAO M, GE WW, et al. Application value of early active fluid resuscitation in mild acute pancreatitis[J]. Chin J Emerg Med, 2019, 28( 6): 794- 797. DOI: 10.3760/cma.j.issn.1671-0282.2019.06.030.李贺, 高明, 葛魏巍, 等. 早期积极液体复苏在轻症急性胰腺炎中的应用价值[J]. 中华急诊医学杂志, 2019, 28( 6): 794- 797. DOI: 10.3760/cma.j.issn.1671-0282.2019.06.030. [24] YAMASHITA T, HORIBE M, SANUI M, et al. Large volume fluid resuscitation for severe acute pancreatitis is associated with reduced mortality: A multicenter retrospective study[J]. J Clin Gastroenterol, 2019, 53( 5): 385- 391. DOI: 10.1097/MCG.0000000000001046. [25] BUXBAUM JL, QUEZADA M, DA B, et al. Early aggressive hydration hastens clinical improvement in mild acute pancreatitis[J]. Am J Gastroenterol, 2017, 112( 5): 797- 803. DOI: 10.1038/ajg.2017.40. [26] WARNDORF MG, KURTZMAN JT, BARTEL MJ, et al. Early fluid resuscitation reduces morbidity among patients with acute pancreatitis[J]. Clin Gastroenterol Hepatol, 2011, 9( 8): 705- 709. DOI: 10.1016/j.cgh.2011.03.032. [27] GARDNER TB, VEGE SS, CHARI ST, et al. Faster rate of initial fluid resuscitation in severe acute pancreatitis diminishes in-hospital mortality[J]. Pancreatology, 2009, 9( 6): 770- 776. DOI: 10.1159/000210022. [28] DERVENIS C, JOHNSON CD, BASSI C, et al. Diagnosis, objective assessment of severity, and management of acute pancreatitis. Santorini consensus conference[J]. Int J Pancreatol, 1999, 25( 3): 195- 210. DOI: 10.1007/BF02925968. [29] BANKS PA, FREEMAN ML, Practice Parameters Committee of the American College of Gastroenterology. Practice guidelines in acute pancreatitis[J]. Am J Gastroenterol, 2006, 101( 10): 2379- 2400. DOI: 10.1111/j.1572-0241.2006.00856.x. [30] WHITCOMB DC. Clinical practice. Acute pancreatitis[J]. N Engl J Med, 2006, 354( 20): 2142- 2150. DOI: 10.1056/NEJMcp054958. [31] PANDOL SJ, SALUJA AK, IMRIE CW, et al. Acute pancreatitis: bench to the bedside[J]. Gastroenterology, 2007, 132( 3): 1127- 1151. DOI: 10.1053/j.gastro.2007.01.055. [32] TENNER S, BAILLIE J, DEWITT J, et al. American College of Gastroenterology guideline: management of acute pancreatitis[J]. Am J Gastroenterol, 2013, 108( 9): 1400- 1415. DOI: 10.1038/ajg.2013.218. [33] KETWAROO G, SEALOCK RJ, FREEDMAN S, et al. Quality of care indicators in patients with acute pancreatitis[J]. Dig Dis Sci, 2019, 64( 9): 2514- 2526. DOI: 10.1007/s10620-019-05674-8. [34] MAO EQ, LI MJ. Early fluid resuscitation and protection of organ function in severe acute pancreatitis[J]. Chin J Dig, 2020, 40( 7): 441- 443. DOI: 10.3760/cma.j.cn311367-20200415-00231.毛恩强, 李梦娇. 重症急性胰腺炎早期液体复苏与器官功能维护[J]. 中华消化杂志, 2020, 40( 7): 441- 443. DOI: 10.3760/cma.j.cn311367-20200415-00231. [35] WU J, LU YC, HUANG Z, et al. Effect of abdominal paracentesis drainage on pancreatic pyroptosis of rats with severe acute pancreatitis and its significance[J]. Med J Chin PLA, 2022, 47( 9): 863- 870. DOI: 10.11855/j.issn.0577-7402.2022.09.0863.吴俊, 卢一琛, 黄竹, 等. 腹腔穿刺引流对重症急性胰腺炎大鼠胰腺细胞焦亡的影响及其意义[J]. 解放军医学杂志, 2022, 47( 9): 863- 870. DOI: 10.11855/j.issn.0577-7402.2022.09.0863. [36] HANSEN B. Fluid overload[J]. Front Vet Sci, 2021, 8: 668688. DOI: 10.3389/fvets.2021.668688. [37] FORGÁCS B, EIBL G, FAULHABER J, et al. Effect of fluid resuscitation with and without endothelin A receptor blockade on hemoconcentration and organ function in experimental pancreatitis[J]. Eur Surg Res, 2000, 32( 3): 162- 168. DOI: 10.1159/000008758. [38] DALFINO L, TULLO L, DONADIO I, et al. Intra-abdominal hypertension and acute renal failure in critically ill patients[J]. Intensive Care Med, 2008, 34( 4): 707- 713. DOI: 10.1007/s00134-007-0969-4. [39] O'CONNOR ME, PROWLE JR. Fluid overload[J]. Crit Care Clin, 2015, 31( 4): 803- 821. DOI: 10.1016/j.ccc.2015.06.013. [40] SUN J, SUN H, SUN Z, et al. Intra-abdominal hypertension and increased acute kidney injury risk: a systematic review and meta-analysis[J]. J Int Med Res, 2021, 49( 5): 3000605211016627. DOI: 10.1177/03000605211016627. [41] WANG T, LIU LY, LUO H, et al. Intra-abdominal pressure reduction after percutaneous catheter drainage is a protective factor for severe pancreatitis patients with sterile fluid collections[J]. Pancreas, 2016, 45( 1): 127- 133. DOI: 10.1097/MPA.0000000000000420. [42] GAD MM, SIMONS-LINARES CR. Is aggressive intravenous fluid resuscitation beneficial in acute pancreatitis? A meta-analysis of randomized control trials and cohort studies[J]. World J Gastroenterol, 2020, 26( 10): 1098- 1106. DOI: 10.3748/wjg.v26.i10.1098. [43] MAO EQ, FEI J, PENG YB, et al. Rapid hemodilution is associated with increased sepsis and mortality among patients with severe acute pancreatitis[J]. Chin Med J(Engl), 2010, 123( 13): 1639- 1644. [44] WU BU, HWANG JQ, GARDNER TH, et al. Lactated Ringer’s solution reduces systemic inflammation compared with saline in patients with acute pancreatitis[J]. Clin Gastroenterol Hepatol, 2011, 9( 8): 710- 717. DOI: 10.1016/j.cgh.2011.04.026. -



 PDF下载 ( 1574 KB)
PDF下载 ( 1574 KB)


 下载:
下载: