C反应蛋白与白蛋白比值对酒精性肝硬化合并自发性细菌性腹膜炎的诊断价值
DOI: 10.3969/j.issn.1001-5256.2023.08.017
Clinical value of C-reactive protein/albumin ratio in the diagnosis of alcoholic cirrhosis with spontaneous bacterial peritonitis
-
摘要:
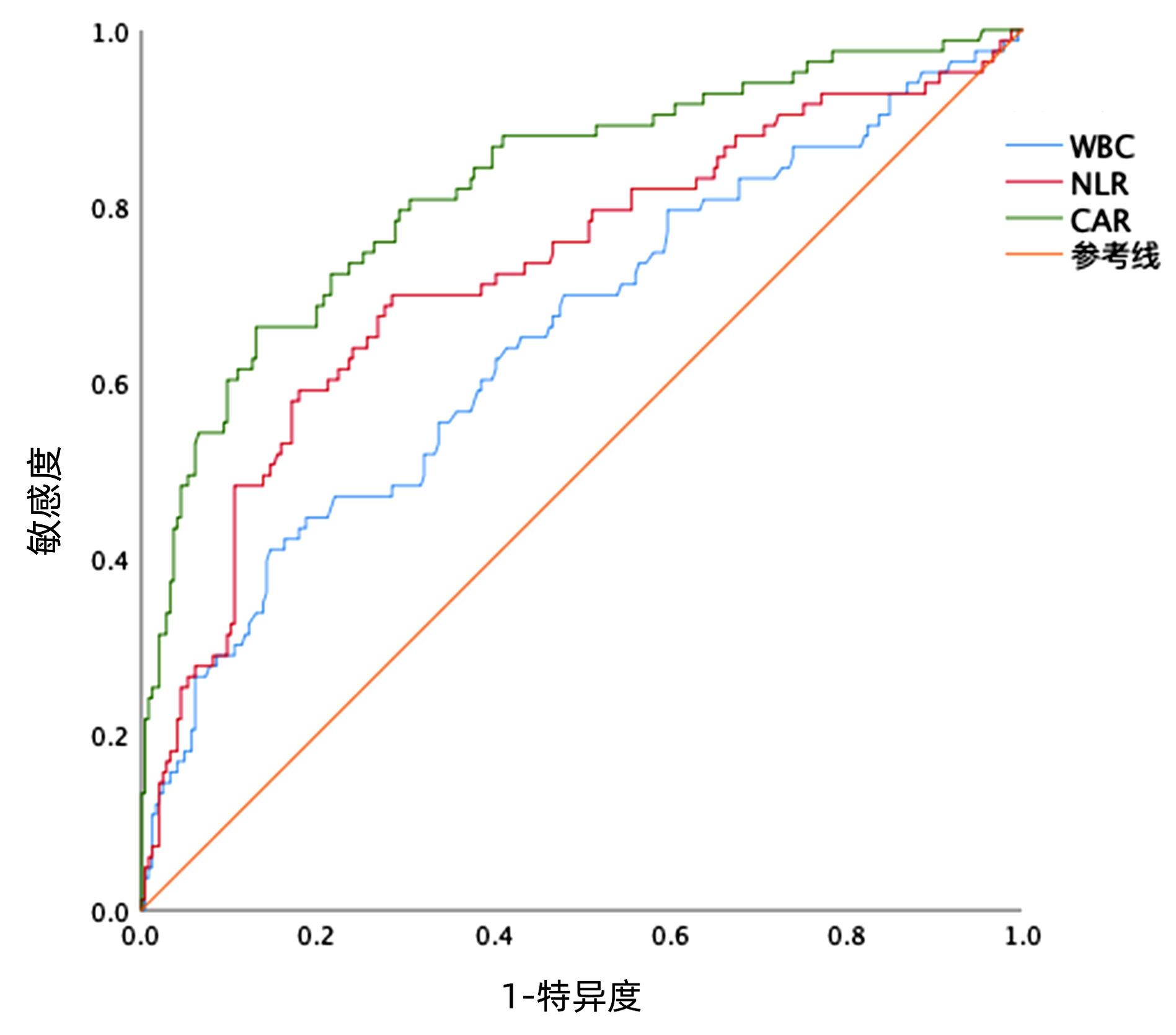
目的 分析C反应蛋白/白蛋白比值(CAR)判断酒精性肝硬化(ALC)患者是否合并自发性细菌性腹膜炎(SBP)的临床价值。 方法 回顾性选取2020年8月—2022年2月首都医科大学附属北京地坛医院住院的ALC患者329例,根据入院时是否合并SBP分为ALC未合并SBP组(n=246)和ALC合并SBP组(n=83),比较两组患者的性别、年龄、合并症、并发症、血常规、肝肾功能、血脂和凝血指标。符合正态分布的计量资料两组间比较采用成组t检验;不符合正态分布的计量资料两组间比较采用Mann-Whitney U检验。计数资料两组间比较采用χ2检验。多因素二元Logistic回归分析判断发生SBP的危险因素,绘制CAR的受试者工作特征曲线(ROC),计算曲线下面积(AUC)、最佳截断值和95%CI。 结果 合并SBP患者的WBC、中性粒细胞、中性粒细胞/淋巴细胞比值、单核细胞、C反应蛋白(CRP)、CAR等炎性指标水平均高于未合并SBP患者,前者的AST、TBil、INR、MELD评分高于后者,而Alb、HDL水平显著低于后者(P值均<0.05)。多因素Logistic回归分析发现CAR(OR=20.628,95%CI: 6.720~74.052,P<0.01)、RBC(OR=0.600,95%CI: 0.381~0.932,P=0.025)是判断ALC患者是否合并SBP的独立危险因素。与NLR(AUC=0.725)、WBC(AUC=0.651)相比,CAR的AUC(AUC=0.825)明显较高。CAR的最佳截断值为0.324,分组后显示高风险组合并SBP的比例是63.2%(55/87),显著高于低风险组的11.6%(28/242)(χ2=90.495,P<0.01)。 结论 CAR是判断ALC患者发生SBP的良好标志物。 -
关键词:
- C反应蛋白/白蛋白比值 /
- 肝硬化, 酒精性 /
- 自发性细菌性腹膜炎
Abstract:Objective To investigate the clinical value of C-reactive protein/albumin ratio (CAR) in determining spontaneous bacterial peritonitis (SBP) in patients with alcoholic cirrhosis (ALC). Methods A retrospective analysis was performed for 329 ALC patients with SBP who were hospitalized in Beijing Ditan Hospital, Capital Medical University, from August 2020 to February 2022, and according to the presence or absence of SBP on admission, they were divided into non-SBP group with 246 patients and SBP group with 83 patients. The two groups were compared in terms of sex, age, comorbidities, complications, blood routine, liver and renal function, blood lipids, and coagulation markers. The independent-samples t test was used for comparison of normally distributed quantitative data between two groups, and the Mann-Whitney U test was used for comparison of non-normally distributed quantitative data between two groups; the chi-square test was used for comparison of qualitative data between two groups. A multivariate binary logistic regression analysis was used to identify the risk factors for SBP. The receiver operating characteristic (ROC) curve was plotted for CAR to calculate the area under the ROC curve (AUC), the optimal cut-off value, and 95% confidence interval (CI). Results Compared with the non-SBP patients, the SBP patients had significantly higher inflammatory indicators (WBC, neutrophils, NLR, monocytes, C-reactive protein, and CAR), significantly higher aspartate aminotransferase, total bilirubin, international normalized ratio, and MELD score, and significantly lower levels of albumin and high-density lipoprotein (all P < 0.05). The multivariate logistic regression analysis showed that CAR (odds ratio [OR]=20.628, 95%CI: 6.720-74.052, P < 0.01) and red blood cell count (OR=0.600, 95%CI: 0.381-0.932, P=0.025) were independent risk factors for determining SBP in ALC patients. CAR had a significantly larger AUC than NLR and WBC (0.825 vs 0.725/0.651) and an optimal cut-off value of 0.324. The patients were divided into high-risk group and low-risk group, and the analysis showed that the high-risk group had a significantly higher proportion of patients with SBP than the low-risk group [63.2% (55/87) vs 11.6%(28/242), χ2=90.495, P < 0.01]. Conclusion CAR is a good marker for determining SBP in patients with ALC. -
表 1 两组患者一般资料的基线水平
Table 1. Baseline characters in two groups
项目 ALC未合并SBP组
(n=246)ALC合并SBP组
(n=83)统计值 P值 性别[例(%)] χ2=0.061 0.804 女 3(1.2) 2(2.4) 男 243(98.8) 81(97.6) 年龄(岁) 57.0(31.0~76.0) 55.0(24.0~78.0) Z=-0.505 0.614 吸烟史[例(%)] χ2=0.193 0.661 否 53(21.5) 16(19.3) 是 193(78.5) 67(80.7) 高血压[例(%)] χ2=0.232 0.630 否 174(70.7) 61(73.5) 是 72(29.3) 22(26.5) 糖尿病[例(%)] χ2=0.781 0.377 否 165(67.1) 60(72.3) 是 81(32.9) 23(27.7) 腹水[例(%)] χ2=20.561 <0.001 否 80(32.5) 6(7.2) 是 166(67.5) 77(92.8) 消化道出血[例(%)] χ2=6.415 0.011 否 199(80.9) 56(67.5) 是 47(19.1) 27(32.5) 肝性脑病[例(%)] χ2=1.677 0.195 否 218(88.6) 69(83.1) 是 28(11.4) 14(16.9) WBC(×109/L) 3.81(0.92~23.60) 4.81(1.12~17.70) Z=-4.104 <0.001 NE(×109/L) 2.31(0.45~17.50) 3.36(0.60~14.80) Z=-5.121 <0.001 LY(×109/L) 0.96(0.16~4.36) 0.85(0.20~3.47) Z=-0.929 0.353 NLR 2.50(0.47~23.10) 4.59(0.62~24.50) Z=-6.142 <0.001 MO(×109/L) 0.36(0.08~1.96) 0.46(0.11~1.63) Z=-2.414 0.016 LMR 2.41(0.67~8.43) 1.82(0.40~7.81) Z=-4.103 <0.001 RBC(×109/L) 3.41±0.87 2.78±0.84 t=5.689 <0.001 Hb(g/L) 103.0±29.5 89.0±27.3 t=3.888 <0.001 PLT(×109/L) 80.0(18.0~366.0) 79.0(33.0~501.0) Z=-0.612 0.541 K(mmol/L) 3.65(1.56~31.50) 3.71(2.54~5.98) Z=-1.196 0.232 Na(mmol/L) 141.3(139.4~142.9) 138.8(135.2~142.6) Z=-3.643 <0.001 Cr(μmol/L) 70.2(40.3~492.0) 77.7(24.3~554.0) Z=-0.815 0.416 ALT(U/L) 20.1(4.7~609.0) 21.6(1.9~496.0) Z=-0.197 0.844 AST(U/L) 30.2(10.8~425.0) 38.0(7.8~317.0) Z=-2.654 0.008 TBil(μmol/L) 25.3(2.4~255.0) 36.7(3.7~304.0) Z=-2.461 0.014 Alb(g/L) 32.80±5.72 28.30±4.62 t=6.504 <0.001 HDL(mmol/L) 0.91(0.08~1.99) 0.59(0.07~1.88) Z=-6.638 <0.001 LDL(mmol/L) 1.74(0.22~5.85) 1.58(0.42~5.13) Z=-1.274 0.203 CRP(mg/L) 2.6(0.0~36.7) 13.5(0.4~141.0) Z=-8.435 <0.001 CAR 0.08(0.00~1.51) 0.52(0.01~7.76) Z=-8.855 <0.001 PT(s) 14.5(9.7~30.8) 15.5(10.9~32.7) Z=-3.364 <0.001 INR 1.34(0.46~12.70) 1.47(1.01~3.03) Z=-3.201 0.001 MELD评分(分) 2.62(-9.35~27.20) 5.37(-4.03~24.40) Z=-3.204 0.001 注:LY,淋巴细胞。 表 2 多因素Logistic回归分析结果
Table 2. Multivariate Logistic regression results
指标 OR 95%CI P值 消化道出血(是= 1,否=0) 1.470 0.664~3.205 0.336 腹水(是=1,否=0) 2.681 1.014~8.316 0.062 WBC 0.987 0.872~1.109 0.831 NLR 1.065 0.945~1.195 0.286 RBC 0.600 0.381~0.932 0.025 Na 0.991 0.965~1.019 0.484 AST 1.002 0.993~1.010 0.629 TBil 0.997 0.989~1.005 0.465 CAR 20.628 6.720~74.052 <0.001 HDL 0.412 0.116~1.376 0.158 INR 1.083 0.382~1.704 0.965 -
[1] SHIZUMA T. Spontaneous bacterial and fungal peritonitis in patients with liver cirrhosis: A literature review[J]. World J Hepatol, 2018, 10(2): 254-266. DOI: 10.4254/wjh.v10.i2.254. [2] GAO XM, LENG XQ. Research advances of serological markers for spontaneous bacterial peritonitis[J]. Med Innov China, 2022, 19(28): 173-176. DOI: 10.3969/j.issn.1674-4985.2022.28.042.高小梅, 冷雪芹. 自发性细菌性腹膜炎的血清学标志物研究进展[J]. 中国医学创新, 2022, 19(28): 173-176. DOI: 10.3969/j.issn.1674-4985.2022.28.042. [3] METWALLY K, FOUAD T, ASSEM M, et al. Predictors of spontaneous bacterial peritonitis in patients with cirrhotic ascites[J]. J Clin Transl Hepatol, 2018, 6(4): 372-376. DOI: 10.14218/JCTH.2018.00001. [4] POPOIAG RE, SUCEVEANU AI, SUCEVEANU AP, et al. Predictors of spontaneous bacterial peritonitis in Romanian adults with liver cirrhosis: Focus on the neutrophil-to-lymphocyte ratio[J]. Exp Ther Med, 2021, 22(3): 983. DOI: 10.3892/etm.2021.10415. [5] HAN CJ, LI WH, WU ZX, et al. Role of NLR, LMR and PNI in anti-infective therapy of liver cirrhosis related spontaneous bacterial peritonitis[J]. Int J Lab Med, 2022, 43(24): 3012-3015, 3021. DOI: 10.3969/j.issn.1673-4130.2022.24.015.韩才均, 李文浩, 吴政燮, 等. NLR、LMR和PNI在肝硬化相关自发性细菌性腹膜炎抗感染治疗中的作用[J]. 国际检验医学杂志, 2022, 43(24): 3012-3015, 3021. DOI: 10.3969/j.issn.1673-4130.2022.24.015. [6] OETTL K, BIRNER-GRUENBERGER R, SPINDELBOECK W, et al. Oxidative albumin damage in chronic liver failure: Relation to albumin binding capacity, liver dysfunction and survival[J]. J Hepatol, 2013, 59(5): 978-983. DOI: 10.1016/j.jhep.2013.06.013. [7] OIKONOMOU T, GOULIS I, KIAPIDOU S, et al. The significance of C-reactive protein to albumin ratio in patients with decompensated cirrhosis[J]. Ann Gastroenterol, 2020, 33(6): 667-674. DOI: 10.20524/aog.2020.0534. [8] Fatty Liver Expert Committee, Chinese Medical Doctor Association, National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association. Guidelines of prevention and treatment for alcoholic liver disease: a 2018 update[J]. J Clin Hepatol, 2018, 34(5): 939-946. DOI: 10.3969/j.issn.1001-5256.2018.05.006.中国医师协会脂肪性肝病专家委员会, 中华医学会肝病学分会脂肪肝和酒精性肝病学组. 酒精性肝病防治指南(2018年更新版)[J]. 临床肝胆病杂志, 2018, 34(5): 939-946. DOI: 10.3969/j.issn.1001-5256.2018.05.006. [9] Chinese Society of Hepatology CMA, XU XY, DUAN ZP, et al. Chinese guidelines on the management of ascites and its related complications in cirrhosis[J]. Hepatol Int, 2019, 13(1): 1-21. DOI: 10.1007/s12072-018-09923-2. [10] BHANDARI R, KHALIQ K, RAVAT V, et al. Chronic alcoholic liver disease and mortality risk in spontaneous bacterial peritonitis: Analysis of 6, 530 hospitalizations[J]. Cureus, 2020, 12(5): e8189. DOI: 10.7759/cureus.8189. [11] BETRAPALLY NS, GILLEVET PM, BAJAJ JS. Gut microbiome and liver disease[J]. Transl Res, 2017, 179: 49-59. DOI: 10.1016/j.trsl.2016.07.005. [12] MARCIANO S, DÍAZ JM, DIRCHWOLF M, et al. Spontaneous bacterial peritonitis in patients with cirrhosis: Incidence, outcomes, and treatment strategies[J]. Hepat Med, 2019, 11: 13-22. DOI: 10.2147/HMER.S164250. [13] SORT P, NAVASA M, ARROYO V, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis[J]. N Engl J Med, 1999, 341(6): 403-409. DOI: 10.1056/NEJM199908053410603. [14] BIGGINS SW, ANGELI P, GARCIA-TSAO G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American association for the study of liver diseases[J]. Hepatology, 2021, 74(2): 1014-1048. DOI: 10.1002/hep.31884. [15] WEHMEYER MH, KROHM S, KASTEIN F, et al. Prediction of spontaneous bacterial peritonitis in cirrhotic ascites by a simple scoring system[J]. Scand J Gastroenterol, 2014, 49(5): 595-603. DOI: 10.3109/00365521.2013.848471. [16] ILIAZ R, OZPOLAT T, BARAN B, et al. Predicting mortality in patients with spontaneous bacterial peritonitis using routine inflammatory and biochemical markers[J]. Eur J Gastroenterol Hepatol, 2018, 30(7): 786-791. DOI: 10.1097/MEG.0000000000001111. [17] DONLON NE, MOHAN H, FREE R, et al. Predictive value of CRP/albumin ratio in major abdominal surgery[J]. Ir J Med Sci, 2020, 189(4): 1465-1470. DOI: 10.1007/s11845-020-02238-y. [18] KANO H, MIDORIKAWA Y, SONG PP, et al. High C-reactive protein/albumin ratio associated with reduced survival due to advanced stage of intrahepatic cholangiocarcinoma[J]. Biosci Trends, 2020, 14(4): 304-309. DOI: 10.5582/bst.2020.03167. [19] KINOSHITA A, ONODA H, IMAI N, et al. The C-reactive protein/albumin ratio, a novel inflammation-based prognostic score, predicts outcomes in patients with hepatocellular carcinoma[J]. Ann Surg Oncol, 2015, 22(3): 803-810. DOI: 10.1245/s10434-014-4048-0. [20] PIOTROWSKI D, SCZEWSKA-PIOTROWSKA A, JAROSZEWICZ J, et al. Lymphocyte-to-monocyte ratio as the best simple predictor of bacterial infection in patients with liver cirrhosis[J]. Int J Environ Res Public Health, 2020, 17(5): 1727. DOI: 10.3390/ijerph17051727. [21] HUANG SS, XIE DM, CAI YJ, et al. C-reactive protein-to-albumin ratio is a predictor of hepatitis B virus related decompensated cirrhosis: Time-dependent receiver operating characteristics and decision curve analysis[J]. Eur J Gastroenterol Hepatol, 2017, 29(4): 472-480. DOI: 10.1097/MEG.0000000000000807. -



 PDF下载 ( 1848 KB)
PDF下载 ( 1848 KB)

 下载:
下载:


