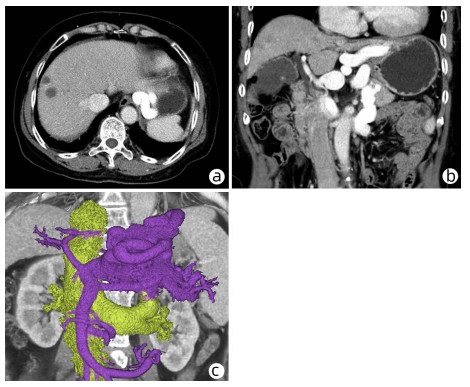
5例Abernethy畸形门静脉高压患者的临床特征分析
DOI: 10.3969/j.issn.1001-5256.2023.03.020
Clinical features of patients with portal hypertension due to Abernethy malformation: An analysis of 5 cases
-
-
关键词:
- Abernethy畸形 /
- 高血压, 门静脉 /
- 肝硬化
-
Key words:
- Abernethy Malformation /
- Hypertension, Portal /
- Liver Cirrhosis
-
表 1 5例Abernethy畸形患者的临床资料
Table 1. Clinical data of 5 patients with Abernethy malformation
编号 性别 年龄 入院主诉 既往史 查体 其他 1 女 67岁 腹胀2个月,呕血、黑便1个月 于外院诊断为“肝炎后肝硬化失代偿期、食管胃底静脉曲张破裂出血” - - 2 女 59岁 反复腹胀10余年 自诉幼年起左侧臀部静脉曲张,既往于外院诊断为“下肢静脉曲张”,行静脉曲张治疗(手术方式不详);10余年前于某医院诊断为“肝硬化” 双侧下肢静脉曲张,以左腿明显,下肢静脉增粗 家族中姐姐、妹妹均有下肢静脉曲张病史 3 男 48岁 确诊肝硬化8年,腹胀1个月,意识改变10 d 乙型肝炎20余年,8年前外院确诊为“乙型肝炎后肝硬化” 精神较差,意识清醒,皮肤巩膜黄染 - 4 男 16岁 呕血1 d 3年前发现先天性肝内胆管扩张,未治疗 - - 5 女 51岁 上腹痛10余年 - 上腹部轻压痛 - 注:-,无特殊既往疾病史或家族疾病史、查体无阳性体征。 表 2 5例Abernethy畸形患者实验室及内镜检查结果
Table 2. Laboratory and endoscopic examinations of 5 patients with Abernethy malformation
编号 血常规 肝功能 HBV血清学标志物 肿瘤标志物 其他 内镜检查 1 WBC 1.62×109/L,Hb 81 g/L,
PLT 55×109/LAlb 31.7 g/L,Glb 34.5 g/L,TBil 26.4 μmol/L,DBil 6.7 μmol/L,IBil 19.7 μmol/L,AST 35.2 U/L 阴性 CEA 6.43 ng/mL 血氨正常;自身抗体谱+肝抗原谱正常 胃镜:胃底静脉曲张 2 WBC 2.67×109/L,Hb 106 g/L,
PLT 109×109/LAlb 30.6 g/L,Glb 33.5 g/L,TBil 24.1 μmol/L,DBil 6.1 μmol/L,IBil 18.0 μmol/L,AST 30.2 U/L 阴性 正常 血氨93.26 μmol/L;自身抗体谱+肝抗原谱、铜蓝蛋白、血脂正常 胃镜:无食管胃静脉曲张;结肠镜:未见异常 3 WBC 3.61×109/L,Hb 99 g/L,
PLT 85×109/LAlb 22.7 g/L,Glb 37.2 g/L,TBil 101.2 μmol/L,DBil 35.5 μmol/L,IBil 66.1 μmol/L,AST 180 U/L 抗-
HBs
阳性AFP 15.2 ng/mL,
CEA 5.92 ng/mL,
CA19-9 29.9 ng/mL血氨正常;自身抗体谱+肝抗原谱正常 胃镜:食管胃底静脉曲张;胃底静脉瘤 4 WBC 2.31×109/L,Hb 77 g/L,
PLT 51×109/L;Alb 28.4 g/L,Glb 33.2 g/L,TBil 73.7 μmol/L,DBil 4.4 μmol/L,IBil 69.3 μmol/L,AST 220 U/L 阴性 正常 血氨90.60 μmol/L;自身抗体谱+肝抗原谱、铜蓝蛋白正常 胃镜: 食管胃静脉曲张重度,门静脉高压性胃病 5 WBC 1.64×109/L,Hb 87 g/L,
PLT 59×109/LAlb 35.7 g/L,Glb 37.3 g/L,TBil 28.6 μmol/L,DBil 4.5 μmol/L,IBil 24.1 μmol/L,AST 34.6 U/L 阴性 正常 血氨正常;自身抗体谱+肝抗原谱正常 胃镜:无食管胃静脉曲张 -
[1] ABERNETHY J. Account of two instances of uncommon formation in the viscera of the human body: from the philosophical transactions of the royal society of London[J]. Med Facts Obs, 1797, 7: 100-108. [2] PEČEK J, FISTER P, HOMAN M. Abernethy syndrome in Slovenian children: Five case reports and review of literature[J]. World J Gastroenterol, 2020, 26(37): 5731-5744. DOI: 10.3748/wjg.v26.i37.5731. [3] MORGAN G, SUPERINA R. Congenital absence of the portal vein: two cases and a proposed classification system for portasystemic vascular anomalies[J]. J Pediatr Surg, 1994, 29(9): 1239-1241. DOI: 10.1016/0022-3468(94)90812-5. [4] LAUTZ TB, TANTEMSAPYA N, ROWELL E, et al. Management and classification of type II congenital portosystemic shunts[J]. J Pediatr Surg, 2011, 46(2): 308-314. DOI: 10.1016/j.jpedsurg.2010.11.009. [5] PONZIANI FR, FACCIA M, ZOCCO MA, et al. Congenital extrahepatic portosystemic shunt: description of four cases and review of the literature[J]. J Ultrasound, 2019, 22(3): 349-358. DOI: 10.1007/s40477-018-0329-y. [6] UCHIDA H, SAKAMOTO S, KASAHARA M, et al. Longterm outcome of liver transplantation for congenital extrahepatic portosystemic shunt[J]. Liver Transpl, 2021, 27(2): 236-247. DOI: 10.1002/lt.25805. [7] WANG W, LI Q, WEN L. An unusual cause of left lower extremity varicose veins[J]. Gastroenterology, 2022, 162(4): e9-e11. DOI: 10.1053/j.gastro.2021.08.010. [8] ALONSO-GAMARRA E, PARRÓN M, PÉREZ A, et al. Clinical and radiologic manifestations of congenital extrahepatic portosystemic shunts: a comprehensive review[J]. Radiographics, 2011, 31(3): 707-722. DOI: 10.1148/rg.313105070. [9] ASH D, SUDHAHAR V, YOUN SW, et al. The P-type ATPase transporter ATP7A promotes angiogenesis by limiting autophagic degradation of VEGFR2[J]. Nat Commun, 2021, 12(1): 3091. DOI: 10.1038/s41467-021-23408-1. [10] TANAKA H, SAIJO Y, TOMONARI T, et al. An adult case of congenital extrahepatic portosystemic shunt successfully treated with balloon-occluded retrograde transvenous obliteration[J]. Intern Med, 2021, 60(12): 1839-1845. DOI: 10.2169/internalmedicine.5914-20. [11] ZHOU M, ZHANG J, LUO L, et al. Surgical ligation for the treatment of an unusual presentation of type II Abernethy malformation[J]. Ann Vasc Surg, 2020, 65: 285. e1-285. e5. DOI: 10.1016/j.avsg.2019.10.094. -



 PDF下载 ( 3579 KB)
PDF下载 ( 3579 KB)


 下载:
下载: