Establishment and evaluation of a nomogram for predicting post-hepatectomy complications in two types of hepatic echinococcosis
-
摘要:
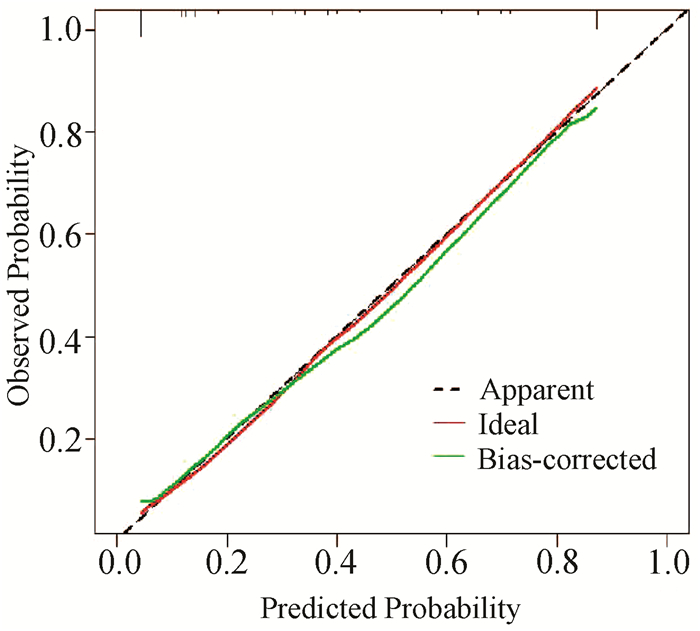
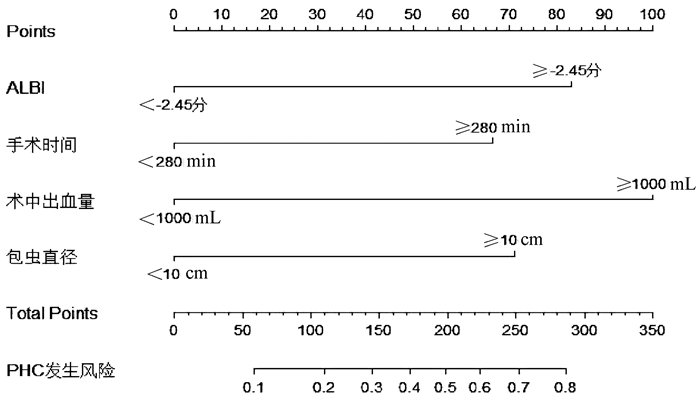
目的 通过分析两型肝包虫病肝切除术后并发症(PHC)的相关危险因素,建立预测肝包虫病PHC发生风险的列线图,并评价其临床使用价值。 方法 收集青海大学附属医院2015年1月—2020年8月收治的263例两型肝包虫病行肝切除手术患者的临床资料,并进行回顾性分析,263例患者中PHC组93例,对照组170例。非正态分布的计量资料2组间比较采用Mann-Whitney U秩和检验,正态性计量资料2组间比较采用独立样本t检验;计数资料2组间比较采用χ2检验和Fisher确切概率法。通过单因素和多因素logistic回归筛选出两型肝包虫病PHC的独立危险因素。根据独立危险因素所占权重,构建列线图预测风险模型。采用Bootstrap重采样法进行模型的内部验证、构建受试者工作特征曲线对模型的区分度进行评价、使用校准曲线和Hosmer-Lemeshow检验对模型的一致性进行评价、绘制临床决策曲线分析(DCA) 验证模型的临床有效性。 结果 ALBI评分(OR=3.694, 95%CI:1.860~7.336)、手术时间(OR=2.848,95%CI:1.384~5.859)、术中出血量(OR=4.832, 95%CI: 2.384~9.793)、包虫直径(OR=3.073,95%CI: 1.528~6.177)是两型肝包虫发生PHC的独立危险因素(P值均<0.05)。基于上述4个独立危险因素所占权重构建列线图风险预测模型,模型的受试者工作特征曲线下面积为0.877(95%CI:0.831~0.923);Bootstrap重采样法进行内部验证的一致性指数(C-index)为0.871,表明模型的区分度良好。校准曲线观测值和实际值贴合,Hosmer-Lemeshow检验(P=0.905)均显示列线图风险预测模型的预测值与实际观测值一致性良好。当阈概率为35.6%时,DCA显示的临床净获益为22%;在8%~89%阈概率区间内有较好的临床适用性。 结论 ALBI评分、手术时间、术中出血量、包虫直径是两型肝包虫病患者发生PHC的独立危险因素,以此为基础构建的列线图风险预测模型具有较好的准确度、一致性及临床实用性。 Abstract:Objective To establish a nomogram for predicting the risk of post-hepatectomy complications (PHC) in hepatic echinococcosis by analyzing the risk factors for PHC in two types of hepatic echinococcosis, and to investigate its value in clinical practice. Methods A retrospective analysis was performed for the clinical data of 263 patients with two types of hepatic echinococcosis who underwent hepatectomy in Qinghai University Affiliated Hospital from January 2015 to August 2020, and among these patients, 93 were enrolled as PHC group and 170 were enrolled as control group. The Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups, and the independent samples t-test was used for comparison of normally distributed continuous data between two groups; the chi-square test and the Fisher's exact test were used for comparison of categorical data between two groups. Univariate and multivariate logistic regression analyses were used to screen out independent risk factors for PHC, and a nomogram risk prediction model was established based on the weight of each independent risk factor. The Bootstrap resampling method was used for internal verification of the model; the receiver operating characteristic (ROC) curve was plotted to evaluate the discriminatory ability of the model; calibration curve and the Hosmer-Lemeshow test were used to evaluate the consistency of the model; decision curve analysis (DCA) was performed to verify the clinical effectiveness of the model. Results Albumin-bilirubin (ALBI) score (odds ratio [OR]=3.694, 95% confidence interval [CI]: 1.860-7.336, P < 0.05), time of operation (OR=2.848, 95%CI: 1.384-5.859, P < 0.05), intraoperative blood loss (OR=4.832, 95%CI: 2.384-9.793, P < 0.05), and hydatid diameter (OR=3.073, 95%CI: 1.528-6.177, P < 0.05) were independent risk factors for PHC in two types of hepatic echinococcosis. A nomogram risk prediction model was established based on the weight of the above four independent risk factors, and the model had an area under the ROC curve of 0.877 (95%CI: 0.831-0.923). The model had a consistency index of 0.871 after internal verification using the Bootstrap resampling method, suggesting that the model had good discriminatory ability. The fitting of the observed value and the actual value of the calibration curve and the Hosmer-Lemeshow test (P=0.905) showed that the predicted value of the nomogram risk prediction model had good consistency with the actual observed value. When the threshold probability was 35.6%, DCA showed a net clinical benefit of 22%, and the model had good clinical applicability within the threshold probability ranging from 8% to 89%. Conclusion ALBI score, time of operation, intraoperative blood loss, and hydatid diameter are independent risk factors for PHC in patients with two types of hepatic echinococcosis, and the nomogram risk prediction model established based on these factors has good accuracy, consistency, and clinical practicability. -
Key words:
- Echinococcosis, Hepatic /
- Hepatectomy /
- Postoperative Complications /
- Risk Factors /
- Nomograms
-
表 1 两型肝包虫病PHC组和对照组资料比较
指标 对照组(n=170) PHC组(n=93) 统计值 P值 年龄(岁) 37.04±13.11 38.73±12.98 t=-1.003 0.317 BMI(kg/m2) 21.61±4.31 21.39±3.36 t=0.427 0.670 APRI 0.23(0.19~0.38) 0.27(0.17~0.49) Z=-0.837 0.403 ALBI评分 -2.66(-2.91~-2.39) -2.31(-2.66~-1.87) Z=-5.333 <0.001 手术时间(min) 250(210~286) 330(287~402) Z=-8.120 <0.001 术中出血量(mL) 400(200~800) 1400(900~2100) Z=-9.310 <0.001 包虫直径(cm) 8.50(6.43~11.07) 11.98(10.02~14.24) Z=-7.227 <0.001 切除段数(例) χ2=38.941 <0.001 <3 79 8 ≥3 91 85 切除部位(例) 0.746 非肝中叶切除 164 89 肝中叶切除 6 4 胆道介入(例) χ2=39.866 <0.001 否 167 68 是 3 25 乙型肝炎(例) χ2=0.782 0.377 否 139 80 是 31 13 手术方式(例) 0.103 开腹肝切除 160 92 腹腔镜肝切除 10 1 阻断方式(例) χ2=0.637 0.425 Pringle阻断 79 48 区域阻断 91 45 表 2 两型肝包虫病PHC的单因素logistic回归分析结果
指标 β值 标准误 Wald值 OR值 95%CI P值 年龄 0.010 0.010 1.006 1.010 0.991~1.030 0.316 BMI -0.014 0.033 0.183 0.986 0.925~1.051 0.669 APRI 0.471 0.257 3.369 1.602 0.969~2.651 0.066 ALBI 2.093 0.292 51.210 8.108 4.571~14.383 <0.001 手术时间 2.087 0.302 47.786 8.058 6.898~23.144 <0.001 术中出血量 2.536 0.309 67.463 12.635 6.898~23.144 <0.001 包虫直径 2.076 0.297 48.839 7.969 4.453~14.264 <0.001 切除段数 2.222 0.401 30.773 9.224 4.207~20.222 <0.001 切除部位 0.206 0.659 0.098 1.228 0.338~4.468 0.755 胆道介入 3.019 0.628 23.127 20.466 5.980~70.039 <0.001 乙型肝炎 -0.317 0.359 0.778 0.729 0.361~1.473 0.378 手术方式 -1.749 1.057 2.739 0.174 0.022~1.380 0.098 阻断方式 -0.206 0.258 0.636 0.814 0.491~1.350 0.425 表 3 两型肝包虫病PHC的多因素logistic回归分析结果
指标 β值 标准误 Wald值 OR值 95%CI P值 ALBI 1.307 0.350 13.939 3.694 1.860~7.336 <0.001 手术时间 1.046 0.368 8.082 2.848 1.384~5.859 0.004 术中出血量 1.575 0.360 19.103 4.832 2.384~9.793 <0.001 包虫直径 1.123 0.356 9.928 3.073 1.528~6.177 0.002 常量 -3.122 0.367 72.444 0.044 <0.001 -
[1] MA L, CHEN DC, ZOU SY, et al. Epidemiological characteristics of hepatic echinococcosis, concurrent cerebral echinococcosis, and pulmonary echinococcosis in Ganzi County, Sichuan Province, China[J]. Medicine (Baltimore), 2020, 99(15): e19753. DOI: 10.1097/MD.0000000000019753. [2] MCMANUS DP, GRAY DJ, ZHANG W, et al. Diagnosis, treatment, and management of echinococcosis[J]. BMJ, 2012, 344: e3866. DOI: 10.1136/bmj.e3866. [3] CEHN L, LI Y. The risk factors and prediction systems for posthepatectomy complications[J]. J Clin Hepatol, 2019, 35(1): 217-221. DOI: 10.3969/j.issn.1001-5256.2019.01.048.陈龙, 李钺. 肝切除术后并发症的危险因素及预测评分系统[J]. 临床肝胆病杂志, 2019, 35(1): 217-221. DOI: 10.3969/j.issn.1001-5256.2019.01.048. [4] KOCH M, GARDEN OJ, PADBURY R, et al. Bile leakage after hepatobiliary and pancreatic surgery: A definition and grading of severity by the International Study Group of Liver Surgery[J]. Surgery, 2011, 149(5): 680-688. DOI: 10.1016/j.surg.2010.12.002. [5] RAHBARI NN, GARDEN OJ, PADBURY R, et al. Posthepatectomy liver failure: A definition and grading by the International Study Group of Liver Surgery (ISGLS)[J]. Surgery, 2011, 149(5): 713-724. DOI: 10.1016/j.surg.2010.10.001. [6] RAHBARI NN, GARDEN OJ, PADBURY R, et al. Post-hepatectomy haemorrhage: A definition and grading by the International Study Group of Liver Surgery (ISGLS)[J]. HPB (Oxford), 2011, 13(8): 528-535. DOI: 10.1111/j.1477-2574.2011.00319.x. [7] National Health commission of the People's Republic of China. Diagnostic criteria for nosocomial infections(proposed)[J]. Natl Med J China, 2001, 81(5): 314-320. DOI: 10.3760/j:issn:0376-2491.2001.05.027.中华人民共和国卫生部. 医院感染诊断标准(试行)[J]. 中华医学杂志, 2001, 81(5): 314-320. DOI: 10.3760/j:issn:0376-2491.2001.05.027. [8] BELLOMO R, RONCO C, KELLUM JA, et al. Acute renal failure-definition, outcome measures, animal models, fluid therapy and information technology needs: The Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group[J]. Crit Care, 2004, 8(4): R204-R212. DOI: 10.1186/cc2872. [9] Chinese Doctor Association, Chinese College of Surgeons (CCS), Chinese Committee for Hadytidology (CCH). Expert consensus on diagnosis and treatment of hepatic cystic and alveolar echinococcosis (2019 edition)[J]. Chin J Dig Surg, 2019, 18(8): 711-721. DOI: 10.3760/cma.j.issn.1673-9752.2019.08.002.中国医师协会外科医师分会包虫病外科专业委员会. 肝两型包虫病诊断与治疗专家共识(2019版)[J]. 中华消化外科杂志, 2019, 18(8): 711-721. DOI: 10.3760/cma.j.issn.1673-9752.2019.08.002. [10] YANG X, QIU Y, WANG W, et al. Risk factors and a simple model for predicting bile leakage after radical hepatectomy in patients with hepatic alveolar echinococcosis[J]. Medicine (Baltimore), 2017, 96(46): e8774. DOI: 10.1097/MD.0000000000008774. [11] NAKAGAWA K, TANAKA K, NOJIRI K, et al. Predictive factors for bile leakage after hepatectomy for hepatic tumors: A retrospective multicenter study with 631 cases at Yokohama Clinical Oncology Group (YCOG)[J]. J Hepatobiliary Pancreat Sci, 2017, 24(1): 33-41. DOI: 10.1002/jhbp.411. [12] SADAMORI H, YAGI T, MATSUDA H, et al. Intractable bile leakage after hepatectomy for hepatocellular carcinoma in 359 recent cases[J]. Dig Surg, 2012, 29(2): 149-156. DOI: 10.1159/000337313. [13] ISHII H, OCHIAI T, MURAYAMA Y, et al. Risk factors and management of postoperative bile leakage after hepatectomy without bilioenteric anastomosis[J]. Dig Surg, 2011, 28(3): 198-204. DOI: 10.1159/000324042. [14] YIN TS, YI YY, MAO XX et al. Meta-analysis of risk factors for posthepatectomy liver failure in patients with hepatocellular carcinoma[J]. J Clin Hepatol, 2014, 30(10): 1009-1014. DOI: 10.3969/j.issn.1001-5256.2014.10.009.尹天圣, 易亚阳, 毛熙贤, 等. 肝癌肝切除术后肝衰竭危险因素的Meta分析[J]. 临床肝胆病杂志, 2014, 30(10): 1009-1014. DOI: 10.3969/j.issn.1001-5256.2014.10.009. [15] CHANG L, YU MC, YUAN YF, et al. Safety and effectiveness of hemihepatic blood flow occlusion versus pringle's maneuver during hepatectomy: A Meta-analysis[J]. Chin J Evid-based Med, 2014, 14(6): 743-751. DOI: 10.7507/1672-2531.20140125.常磊, 喻满成, 袁玉峰, 等. 半肝血流阻断法与Pringle法在肝切除术应用中安全性与有效性比较的Meta分析[J]. 中国循证医学杂志, 2014, 14(6): 743-751. DOI: 10.7507/1672-2531.20140125. [16] ZENG YC, DING HD, ZOU RY, et al. Research progress on the risk factors, prevention and therapy in posthepatectomy liver failure[J]. Chin J Hepatobiliary Surg, 2019, 25(9): 711-715. DOI: 10.3760/cma.j.issn.1007-8118.2019.09.020.曾勇超, 丁宏达, 邹若媱, 等. 肝切除术后肝功能衰竭危险因素与防治的研究进展[J]. 中华肝胆外科杂志, 2019, 25(9): 711-715. DOI: 10.3760/cma.j.issn.1007-8118.2019.09.020. [17] XU Y, LI JB, HU XL, et al. Research status of risk predictors and corresponding strategies of posthepatectomy liver failure[J]. Chin J Dig Surg, 2020, 19 (2): 220-224. DOI: 10.3760/cma.j.issn.1673-9752.2020.02.016.徐岩, 李江斌, 胡小玲, 等. 肝切除术后肝衰竭风险预测指标及应对策略的研究现状[J]. 中华消化外科杂志, 2020, 19 (2): 220-224. DOI: 10.3760/cma.j.issn.1673-9752.2020.02.016. [18] CHENG WL, QI YQ, CHEN YJ, et al. A meta-analysis of risk factors of postoperative infectious complications after liver resection for hepatocellular carcinoma[J]. Chin J Hepatobiliary Surg, 2016, 22(1): 5-8. DOI: 10.3760/cma.j.issn.1007-8118.2016.01.002.承文龙, 齐永强, 陈勇军, 等. 肝癌肝切除术后感染并发症相关危险因素的Meta分析[J]. 中华肝胆外科杂志, 2016, 22(1): 5-8. DOI: 10.3760/cma.j.issn.1007-8118.2016.01.002. [19] CHEN L, WANG YB, ZHANG YH, et al. Effective prediction of postoperative complications for patients after open hepatectomy: A simplified scoring system based on perioperative parameters[J]. BMC Surg, 2019, 19(1): 128. DOI: 10.1186/s12893-019-0597-2. [20] ZOU H, WEN Y, YUAN K, et al. Combining albumin-bilirubin score with future liver remnant predicts post-hepatectomy liver failure in HBV-associated HCC patients[J]. Liver Int, 2018, 38(3): 494-502. DOI: 10.1111/liv.13514. [21] ANDREATOS N, AMINI N, GANI F, et al. Albumin-Bilirubin Score: Predicting short-term outcomes including bile leak and post-hepatectomy liver failure following hepatic resection[J]. J Gastrointest Surg, 2017, 21(2): 238-248. DOI: 10.1007/s11605-016-3246-4. [22] TIAN F, LIU Y, GAO J, et al. Study on the association between TGF-β1 and liver fibrosis in patients with hepatic cystic echinococcosis[J]. Exp Ther Med, 2020, 19(2): 1275-1280. DOI: 10.3892/etm.2019.8355. [23] ZHANG C, WANG L, ALI T, et al. Hydatid cyst fluid promotes peri-cystic fibrosis in cystic echinococcosis by suppressing miR-19 expression[J]. Parasit Vectors, 2016, 9(1): 278. DOI: 10.1186/s13071-016-1562-x. [24] WANG Y, LIU XM, WANG B, et al. Preoperative aspartate transaminase and platelet ratio index(APRI)as a predictor of postoperative complications after hepatic resection for primary hepatocellular carcinoma[J]. Chin J Hepatobiliary Surg, 2016, 22(5): 289-293. DOI: 10.3760/cma.j.issn.1007-8118.2016.05.001.王越, 刘学民, 王博, 等. 术前天冬氨酸转氨酶/血小板比值指数对肝细胞癌患者手术切除后并发症的预测价值[J]. 中华肝胆外科杂志, 2016, 22(5): 289-293. DOI: 10.3760/cma.j.issn.1007-8118.2016.05.001. -



 PDF下载 ( 2502 KB)
PDF下载 ( 2502 KB)

 下载:
下载: