A serum metabolomics study on the intervention of nonalcoholic fatty liver disease by equicaloric low-carbohydrate high-protein diet combined with aerobic exercise
-
摘要:
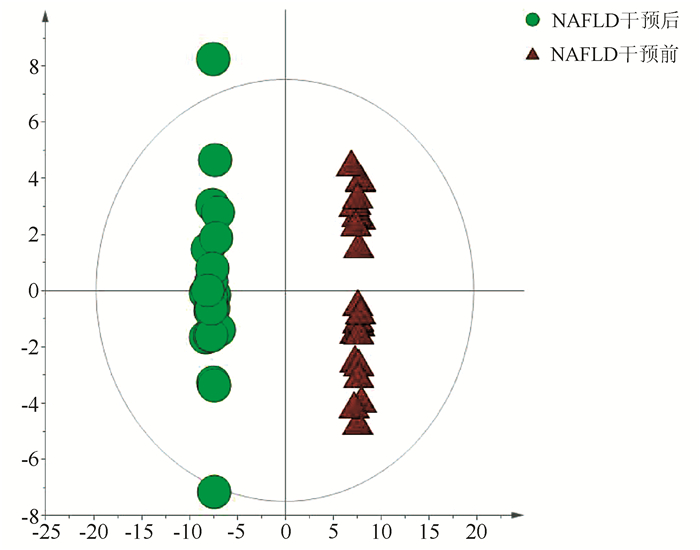
目的 收集非酒精性脂肪性肝病(NAFLD)患者的血清并对生活方式干预前后的血清代谢生物标志物变化情况进行分析。 方法 收集2019年1月—2020年1月于上海市普陀区中心医院消化科及住院部诊断为NAFLD的患者23例,患者采取有氧运动及等热量低碳水化合物高蛋白饮食进行干预,从体检中心选择13例健康志愿者作为对照组。NAFLD患者于干预前后进行常规的基本信息采集,并分别采血2次检测肝功能、血糖、血脂等指标,另分装部分血清用于血清代谢组学分析。将血清样本通过处理后使用超高效液相色谱串联高分辨质谱(UPLC-Q-Orbitrap/MS)进行分析。采集的数据经Compound Discover处理后运用主成分分析(PCA) 和正交偏最小二乘判别法分析构建患者与正常健康人的差异血清代谢物谱,并对差异代谢通路进行富集分析。正态分布的计量资料两组比较采用独立样本t检验;非分正态分布的计量资料两组比较采用Wilcoxon非参数检验。 结果 经生活方式干预后,患者的BMI及体质量均明显降低(P值均<0.01);血清生化指标ALP、Alb、GGT、ALT表达水平均降低(P值均<0.05),总蛋白(TP)显著降低(P<0.01),胆碱酯酶(ChE)、AST、血糖(GLU)改善不明显;血脂四项中TG的水平显著减低(P<0.01),HDL-C、LDL-C、TC改善不显著。代谢组学研究发现NAFLD患者生活方式干预前后,血清中的代谢产物有33种代谢物发生了明显改变。此外,PCA结果显示NAFLD患者经干预后,体内的代谢产物水平趋于健康人。通过信号通路分析,发现运动饮食主要影响了胆汁酸、不饱和脂肪酸合成及苯丙氨酸代谢等通路。 结论 生活方式干预可不同程度的减轻NAFLD患者的体质量,改善血清生化指标,改善NAFLD患者的异常代谢途径,这对指导临床医生为NAFLD患者制订合理的饮食及运动策略,预防NAFLD进展具有一定的临床价值和意义。 Abstract:Objective To collect the serum samples of patients with nonalcoholic fatty liver disease (NAFLD), and to investigate the changes in serum metabolic biomarkers before and after lifestyle intervention. Methods A total of 23 patients who were diagnosed with NAFLD in Department of Gastroenterology and Inpatient Department, Putuo District Central Hospital of Shanghai, from January 2019 to January 2020 were enrolled, and all patients received the intervention with aerobic exercise and equicaloric low-carbohydrate high-protein diet. A total of 13 healthy volunteers who underwent physical examination in Physical Examination Center were enrolled as control group. For the patients with NAFLD, basic information was collected before and after intervention, blood samples were collected twice to measure liver function, blood glucose, and blood lipids, and part of serum was used for serum metabolomics analysis. The serum samples were analyzed by ultra-performance liquid chromatography/tandem high-resolution mass spectrometry. The data collected were processed in Compound Discover, and then principal component analysis (PCA) and orthogonal partial least squares discriminant analysis were used to establish the profile of differentially expressed blood metabolites between patients and healthy people and perform the enrichment analysis of differentially expressed metabolic pathways. The independent samples t-test was used for comparison of normally distributed continuous data between two groups, and the Wilcoxon non-parametric test was used for comparison of non-normally distributed continuous data between two groups. Results After lifestyle intervention, the patients had significant reductions in body mass index (P < 0.01), body weight (P < 0.01), and serum biochemical parameters alkaline phosphatase, albumin, gamma-glutamyl transpeptidase, and alanine aminotransferase (all P < 0.05), as well as a significant reduction in total protein (P < 0.01), while there were no significant improvements in cholinesterase, aspartate aminotransferase, and glucose. As for the four items for blood lipids, there was a significant reduction in triglyceride (P < 0.01), while there were no significant improvements in high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and total cholesterol. The metabolomics analysis showed that 33 serum metabolites changed significantly after lifestyle intervention. In addition, PCA results showed that after intervention, the level of metabolites in patients tended to be normal. The signaling pathway analysis showed that exercise and diet mainly affected the pathways of bile acid, unsaturated fatty acid synthesis, and phenylalanine metabolism. Conclusion Lifestyle intervention can achieve varying degrees of reduction in the body weight of patients with NAFLD, improve serum biochemical parameters, and regulate the abnormal metabolic pathway in patients with NAFLD, which has important clinical value and significance for guiding clinicians to formulate reasonable diet and exercise strategies for patients with NAFLD and prevent the progression of NAFLD. -
表 1 梯度洗脱程序
时间(min) 流速(mL/min) A(%) B(%) 0 0.3 95 5 2 0.3 95 5 12 0.3 5 95 15 0.3 5 95 17 0.3 95 5 表 2 2组基线资料及血清生化参数比较
参数 健康对照组(n=13) NAFLD组(n=23) 统计值 P值 年龄(岁) 42±14 48±14 t=1.208 0.235 体质量(kg) 82.00(74.00~90.00) 71.00(68.00~77.85) Z=2.408 0.015 BMI(kg/m2) 27.08(25.86~27.85) 24.98(24.22~26.61) Z=-2.289 0.022 腰围(cm) 102.38±10.02 94.50±14.17 t=1.721 0.094 TBil(μmol/L) 11.00(10.00~14.00) 13.00(10.00~14.20) Z=-0.564 0.580 DBil(μmol/L) 2.21±0.75 2.38±0.75 t=-0.625 0.536 ALP(U/L) 70.00(61.00~87.00) 86.00(69.00~100.50) Z=-1.648 0.100 TP(g/L) 72.00(67.00~75.00) 76.00(72.50~79.15) Z=-1.404 0.169 Alb(μmol/L) 30.00(27.00~31.00) 39.00(30.00~45.50) Z=-1.584 0.015 GGT(U/L) 30.00(25.00~46.00) 55.00(32.50~75.00) Z=-2.208 0.026 ChE(U/L) 9732.85±1244.79 10 047.35±1488.81 t=-0.627 0.535 ALT(U/L) 43.00(28.00~47.00) 61.00(28.50~102.50) Z=-1.763 0.031 AST(U/L) 26.00(25.00~35.00) 32.00(23.00~52.50) Z=-1.172 0.253 GLU(mmol/L) 4.80(4.50~5.10) 5.50(5.10~5.65) Z=-2.295 0.022 HDL-C(mmol/L) 1.26±0.33 1.15±0.25 t=1.168 0.410 LDL-C(mmol/L) 3.73±0.68 3.44±1.10 t=0.835 0.282 TC(mmol/L) 4.36±1.79 5.05±1.76 t=-1.093 0.018 TG(mmol/L) 1.72(1.43~2.89) 2.63(1.82~3.69) Z=-1.268 0.021 注:TP,总蛋白;ChE,胆碱酯酶;GLU,血糖。 表 3 NAFLD组干预前后临床资料及血清生化参数比较
参数 干预前 干预后 统计值 P值 体质量(kg) 71.00(68.00~77.85) 68.00(63.00~72.75) Z=-1.442 0.149 BMI(kg/m2) 24.98(24.22~26.61) 24.17(23.07~25.53) Z=-1.736 0.083 腰围(cm) 94.50±14.17 90.12±13.91 t=1.035 0.306 TBil(μmol/L) 13.00(10.00~14.20) 13.00(10.50~14.50) Z=-0.343 0.731 DBil(μmol/L) 2.38±0.75 2.28±0.74 t=0.434 0.666 ALP(U/L) 86.00(69.00~100.50) 85.00(68.00~99.50) Z=-0.066 0.947 TP(g/L) 76.00(72.50~79.15) 74.00(72.00~79.50) Z=-0.264 0.792 Alb(μmol/L) 39.00(30.00~45.50) 36.00(29.90~45.50) Z=-1.004 0.035 GGT(U/L) 55.00(32.50~75.00) 41.00(22.50~46.00) Z=-2.089 0.037 ChE(U/L) 10 047.35±1488.81 9575.26±1938.16 t=0.906 0.370 ALT(U/L) 61.00(28.50~102.50) 32.00(24.50~55.00) Z=-1.726 0.044 AST(U/L) 32.00(23.00~52.50) 34.00(21.00~45.00) Z=-1.431 0.152 GLU(mmol/L) 5.50(5.10~5.65) 5.30(4.45~5.50) Z=-1.389 0.165 HDL-C(mmol/L) 1.15±0.25 1.15±0.21 t=-0.111 0.765 LDL-C(mmol/L) 3.44±1.10 3.35±0.81 t=0.301 0.109 TC(mmol/L) 5.05±1.76 4.27±1.38 t=1.635 0.013 TG(mmol/L) 2.63(1.82~3.69) 1.59(1.22~2.30) Z=-2.702 0.007 -
[1] DIEHL AM, DAY C. Cause, Pathogenesis, and Treatment of Nonalcoholic Steatohepatitis[J]. N Engl J Med, 2017, 377(21): 2063-2072. DOI: 10.1056/NEJMra1503519. [2] GAO JJ, WANG T, JIANG YY, et al. Metabonomics and traditional Chinese medicine syndrome of nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2020, 36(8): 1880-1882. DOI: 10.3969/j.issn.1001-5256.2020.08.044.高静静, 汪涛, 蒋元烨, 等. 非酒精性脂肪性肝病代谢组学与中医证候[J]. 临床肝胆病杂志, 2020, 36(8): 1880-1882. DOI: 10.3969/j.issn.1001-5256.2020.08.044. [3] ANGELICO F, DEL BEN M, CONTI R, et al. Non-alcoholic fatty liver syndrome: A hepatic consequence of common metabolic diseases[J]. J Gastroenterol Hepatol, 2003, 18(5): 588-594. DOI: 10.1046/j.1440-1746.2003.02958.x. [4] YANG CQ, SHU L, WANG S, et al. Dietary patterns modulate the risk of non-alcoholic fatty liver disease in chinese adults[J]. Nutrients, 2015, 7(6): 4778-4791. DOI: 10.3390/nu7064778. [5] BARSHOP NJ, SIRLIN CB, SCHWIMMER JB, et al. Review article: Epidemiology, pathogenesis and potential treatments of paediatric non-alcoholic fatty liver disease[J]. Aliment Pharmacol Ther, 2008, 28(1): 13-24. DOI: 10.1111/j.1365-2036.2008.03703.x. [6] MARDINOGLU A, WU H, BJORNSON E, et al. An integrated understanding of the rapid metabolic benefits of a carbohydrate-restricted diet on hepatic steatosis in humans[J]. Cell Metab, 2018, 27(3): 559-571. e5. DOI: 10.1016/j.cmet.2018.01.005. [7] JIMBA S, NAKAGAMI T, TAKAHASHI M, et al. Prevalence of non-alcoholic fatty liver disease and its association with impaired glucose metabolism in Japanese adults[J]. Diabet Med, 2005, 22(9): 1141-1145. DOI: 10.1111/j.1464-5491.2005.01582.x. [8] FRIIS-LIBY I, ALDENBORG F, JERLSTAD P, et al. High prevalence of metabolic complications in patients with non-alcoholic fatty liver disease[J]. Scand J Gastroenterol, 2004, 39(9): 864-869. DOI: 10.1080/00365520410006431. [9] HUANG W, KONG D. The intestinal microbiota as a therapeutic target in the treatment of NAFLD and ALD[J]. Biomed Pharmacother, 2021, 135: 111235. DOI: 10.1016/j.biopha.2021.111235. [10] MA X, GU HT, ZHAO Y, et al. Serum metabolomics study on nonalcoholic fatty liver disease with liver damage of different syndromes[J]. China J Tradit Chin Med Pharma, 2017, 32(3): 1246-1250. https://www.cnki.com.cn/Article/CJFDTOTAL-BXYY201703103.htm马欣, 顾宏图, 赵瑜, 等. 不同证候的非酒精性脂肪肝合并肝损伤患者的血清代谢组学分析[J]. 中华中医药杂志, 2017, 32(3): 1246-1250. https://www.cnki.com.cn/Article/CJFDTOTAL-BXYY201703103.htm [11] LIN L, YAN H, CHEN J, et al. Application of metabolomics in viral pneumonia treatment with traditional Chinese medicine[J]. Chin Med, 2019, 14: 8. DOI: 10.1186/s13020-019-0229-x. [12] Group of Fatty Liver and Alcoholic Liver Diseases, Society of Hepatology, Chinese Medical Association. Guidelines for Management of non-alcoholic fatty liver disease[J]. J Clin Hepatol, 2010, 26(2): 120-124. http://lcgdbzz.org/cn/article/doi/1001-5256%20(2010)%2002-0120-05中华医学会肝脏病学分会脂肪肝和酒精性肝病学组. 非酒精性脂肪性肝病诊疗指南[J]. 临床肝胆病杂志, 2010, 26(2): 120-124. http://lcgdbzz.org/cn/article/doi/1001-5256%20(2010)%2002-0120-05 [13] NASCIMBENI F, PAIS R, BELLENTANI S, et al. From NAFLD in clinical practice to answers from guidelines[J]. J Hepatol, 2013, 59(4): 859-871. DOI: 10.1016/j.jhep.2013.05.044. [14] ZHANG HJ, HE J, PAN LL, et al. Effects of moderate and vigorous exercise on nonalcoholic fatty liver disease: A randomized clinical trial[J]. JAMA Intern Med, 2016, 176(8): 1074-1082. DOI: 10.1001/jamainternmed.2016.3202. [15] VUPPALANCHI R, CHALASANI N. Nonalcoholic fatty liver disease and nonalcoholic steatohepatitis: Selected practical issues in their evaluation and management[J]. Hepatology, 2009, 49(1): 306-317. DOI: 10.1002/hep.22603. [16] SUN GJ, JIANG AL, LI YB, et al. Progress in the research of metabonomics in disease diagnosis and Chinese medicine treatment [J]. Chin J Integr Trad West Med, 2021, 41(1): 122-125. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZXJ202101030.htm孙桂江, 姜埃利, 李遇伯, 等. 代谢组学在疾病诊断及中药治疗的研究进展[J]. 中国中西医结合杂志, 2021, 41(1): 122-125. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZXJ202101030.htm [17] TIAN G, LI C, ZHAI YY, et al. Effect of Pudilan Xiaoyan Oral Liquid on energy metabolism in mice with acute pneumonia induced by LPS based on serum tar-geted metabolomics[J]. J Nangjing Univ Tradit Chin Med, 2021, 37(1): 120-125. DOI: 10.14148/j.issn.1672-0482.2021.0120.田刚, 李超, 翟园园, 等. 基于血清靶向代谢组学研究蒲地蓝消炎口服液对脂多糖诱导的急性肺炎小鼠能量代谢的影响[J]. 南京中医药大学学报, 2021, 37(1): 120-125. DOI: 10.14148/j.issn.1672-0482.2021.0120. [18] MA R, XIE Q, WANG J, et al. Metabolomics study on effects of compatibility of alcohol extracts of Magnolia officinalis and Polygala tenuifolia on urine metabolites in rats[J]. Chin Pharmacol Bull, 2019, 35(6): 870-877. DOI: 10.3969/j.issn.1001-1978.2019.06.026.马荣, 谢倩, 王建, 等. 基于代谢组学研究厚朴远志配伍醇提物对尿液代谢物的影响[J]. 中国药理学通报, 2019, 35(6): 870-877. DOI: 10.3969/j.issn.1001-1978.2019.06.026. [19] WANG X, WANG X, XIE G, et al. Urinary metabolite variation is associated with pathological progression of the post-hepatitis B cirrhosis patients[J]. J Proteome Res, 2012, 11(7): 3838-3847. DOI: 10.1021/pr300337s. [20] YU Y. The toxic effect of high dose phenylalanine on mice liver[D]. Changchun: Jilin University, 2018.于杨. 高苯丙氨酸对小鼠肝脏的毒性作用[D]. 长春: 吉林大学, 2018. [21] SUN YX. Explore the protective mechanism of metformin on bisphenol A-induced liver injury in rats based on metabolomics[D]. Zhengzhou: Zhengzhou University, 2020.孙亚新. 基于代谢组学技术的二甲双脈对双酚A诱导大鼠肝损伤的保护作用机制研究[D]. 郑州: 郑州大学, 2020. [22] WANG W, YANG J, QI W, et al. Lipidomic profiling of high-fat diet-induced obesity in mice: Importance of cytochrome P450-derived fatty acid epoxides[J]. Obesity (Silver Spring), 2017, 25(1): 132-140. DOI: 10.1002/oby.21692. [23] WATERS PJ, PARNIAK M, AKERMAN BR, et al. Characterization of phenylketonuria missense substitutions, distant from the phenylalanine hydroxylase active site, illustrates a paradigm for mechanism and potential modulation of phenotype[J]. Mol Genet Metab, 2000, 69(2): 101-110. DOI: 10.1006/mgme.2000.2965. -



 PDF下载 ( 4093 KB)
PDF下载 ( 4093 KB)


 下载:
下载: