乙型肝炎肝硬化患者发生慢性肾病的影响因素分析
DOI: 10.3969/j.issn.1001-5256.2021.08.015
Influencing factors for chronic kidney disease in patients with hepatitis B cirrhosis
-
摘要:
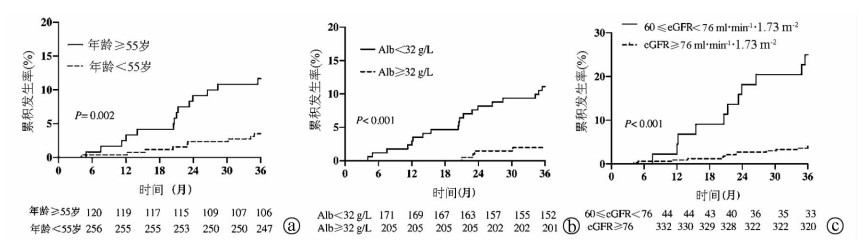
目的 探讨乙型肝炎肝硬化患者3年内发生慢性肾病(CKD)的影响因素。 方法 纳入2014年1月—2017年7月就诊于首都医科大学附属北京地坛医院的乙型肝炎肝硬化患者376例,随访3年,根据是否发生CKD分为CKD组(n=23)和非CKD组(n=353)。收集患者一般情况和实验室指标。计量资料两组间比较采用t检验或Mann-Whitney U检验。计数资料两组间比较采用χ2检验或Fisher精确概率法。采用多因素Cox逐步向前回归方法,分析乙型肝炎肝硬化患者3年内发生CKD的独立影响因素。采用受试者工作特征曲线下面积(AUC)评估影响因素对乙型肝炎肝硬化患者发生CKD的预测价值,Kalplan-Merier法进行生存分析,log-rank检验比较不同风险患者CKD累积发生率。 结果 Cox多因素分析显示,年龄(HR=1.078,95%CI:1.007~1.114,P=0.026)、Alb(HR=0.923,95%CI:0.860~0.989,P=0.024)、肾小球滤过率(eGFR)(HR=0.977,95%CI:0.955~0.999,P=0.037)是乙型肝炎肝硬化患者3年内发生CKD的独立影响因素。年龄、Alb、eGFR对CKD发生的预测价值较好(受试者工作特征曲线下面积分别为0.701、0.710、0.706)。Kalplan-Merier生存曲线显示,基线年龄≥55岁、Alb<32 g/L、60 ml·min-1·1.73m-2≤eGFR<76 ml·min-1·1.73m-2的患者发生CKD的风险高(χ2值分别为9.647、13.621、30.940,P值均<0.05)。 结论 高龄、低Alb水平及eGFR较低的患者建议密切监测肾功能。 Abstract:Objective To investigate the influencing factors for chronic kidney disease (CKD) in patients with hepatitis B cirrhosis within 3 years. Methods A total of 376 patients with hepatitis B cirrhosis who attended Beijing Ditan Hospital, Capital Medical University, from January 2014 to July 2017 were enrolled and followed up for 3 years, and according to the presence or absence of CKD, they were divided into CKD group with 23 patients and non-CKD group with 353 patients. Related general information and laboratory markers were collected. The t-test or the Mann-Whitney U test was used for comparison of continuous data between two groups, and the chi-square test or the Fisher's exact test was used for comparison of categorical data between two groups; a stepwise forward Cox regression analysis was used to screen out the independent influencing factors for CKD within 3 years in patients with hepatitis B cirrhosis. The area under the receiver operating characteristic curve (AUC) was used to investigate the value of the influencing factors in predicting CKD in patients with hepatitis B cirrhosis; the Kaplan-Meier method was used for survival analysis, and the log-rank test was used for comparison of the cumulative incidence rate of CKD between the patients with different risks. Results The multivariate Cox regression analysis showed that age (hazard ratio [HR]=1.078, 95% confidence interval [CI]: 1.007-1.114, P=0.026), albumin (Alb) (HR=0.923, 95% CI: 0.860-0.989, P=0.024), and estimated glomerular filtration rate (eGFR) (HR=0.977, 95% CI: 0.955-0.999, P=0.037) were independent influencing factors for CKD within 3 years in patients with hepatitis B cirrhosis. Age, Alb, and eGFR had a relatively good value in predicting CKD, with AUCs of 0.701, 0.710, and 0.706, respectively. The Kaplan-Meier survival curve showed that the patients with baseline age ≥55 years, Alb < 32 g/L, and eGFR ≥60 ml·min-1·1.73 m-2 and < 76 ml·min-1·1.73 m-2 had a higher risk of CKD (χ2=9.647, 13.621, and 30.940, all P < 0.05). Conclusion Renal function should be closely monitored for patients with old age and low Alb and eGFR levels. -
Key words:
- Liver Cirrhosis /
- Kidney Diseases /
- Root Cause Analysis
-
表 1 CKD组和非CKD组患者基线特征比较
指标 CKD组(n=23) 非CKD组(n=353) 统计值 P值 年龄(岁) 56.1±10.2 48.7±9.9 t=1.516 <0.001 男/女(例) 18/5 259/94 χ2=0.011 0.978 失代偿期肝硬化[例(%)] 19(82.6) 216(61.2) χ2=1.300 0.039 饮酒史[例(%)] 2(8.7) 54(15.3) χ2=0.647 0.389 吸烟史[例(%)] 4(17.4) 88(24.9) χ2=1.220 0.415 腹水[例(%)] 11(47.8) 108(30.6) χ2=3.522 0.152 上消化道出血[例(%)] 7(30.4) 63(17.8) χ2=0.066 0.181 肝性脑病[例(%)] 1(4.3) 11(3.1) χ2=0.175 0.077 ALT(U/L) 36.9(17.9~53.4) 37.0(22.8~75.5) Z=-0.752 0.209 AST(U/L) 43.8(31.9~71.7) 39.6(26.5~81.3) Z=-0.560 0.053 TBil(μmol/L) 22.2(15.3~30.5) 22.7(13.8~35.7) Z=5.136 0.521 Alb(g/L) 27.8(26.0~31.0) 33.2(28.3~38.3) Z=-0.794 0.004 ALP(U/L) 93.9(68.8~130.1) 79.3(59.7~106.4) Z=-0.199 0.088 GGT(U/L) 38.2(16.5~76.0) 37.4(19.4~84.5) Z=-0.564 0.336 TC(mmol/L) 2.7(2.4~3.6) 3.2(2.6~3.9) Z=-1.675 0.230 TG(mmol/L) 0.6(0.5~1.0) 0.7(0.5~1.0) Z=-0.681 0.104 HDL(mmol/L) 0.9(0.5~1.2) 0.8(0.5~1.1) Z=-0.802 0.986 LDL(mmol/L) 1.4(1.1~1.5) 1.6(1.3~2.1) Z=-2.310 0.114 WBC(×109/L) 4.2(2.8~5.4) 3.6(2.7~5.1) Z=1.180 0.521 PLT(×109/L) 79.5(44.0~98.4) 72.0(49.0~108.0) Z=0.127 0.583 BUN(mmol/L) 5.1(4.0~6.5) 5.4(4.2~6.5) Z=0.527 0.217 Cr(μmoI/L) 71.0(62.0~85.0) 66.0(56.0~75.0) Z=0.302 0.116 PT(s) 14.9(13.6~16.3) 14.3(12.9~16.0) Z=1.410 0.211 INR 1.3(1.2~1.4) 1.2(1.1~1.4) Z=0.923 0.523 HBeAg阳性[例(%)] 10(43.5) 175(49.6) χ2=0.065 0.799 HBV DNA(log10拷贝/ml) 4.3(2.7~5.7) 3.5(2.7~5.5) Z=-0.105 0.731 eGFR(ml·min-1·1.73 m-2) 75.9(67.7~106.5) 102.7(87.1~119.5) Z=-0.774 0.016 表 2 乙型肝炎肝硬化患者发生CKD的单因素分析
因素 HR(95%CI) P值 年龄(岁) 1.090(1.040~1.141) <0.001 男性 1.009(0.398~2.258) 0.986 失代偿期肝硬化 2.892(1.048~8.500) 0.045 吸烟史 0.650(0.221~1.909) 0.433 饮酒史 0.541(0.127~2.305) 0.406 腹水 1.421(0.096~1.969) 0.053 上消化道出血 1.852(0.762~4.502) 0.863 肝性脑病 0.852(0.215~3.377) 0.819 ALT(U/L) 0.996(0.991~1.003) 0.215 AST(U/L) 0.998(0.992~1.002) 0.412 TBil(μmol/L) 1.002(0.996~1.009) 0.499 Alb(g/L) 0.904(0.884~0.970) 0.005 ALP(U/L) 1.008(0.999~1.116) 0.076 GGT(U/L) 0.996(0.989~1.004) 0.331 WBC(×109/L) 1.071(0.868~1.321) 0.523 PLT(×109/L) 0.997(0.988~1.007) 0.583 BUN(mmol/L) 1.119(0.077~1.328) 0.126 Cr(μmoI/L) 1.033(0.997~1.062) 0.118 PT(s) 1.079(0.964~1.208) 0.186 INR 1.620(0.401~6.565) 0.498 TC(mmol/L) 0.759(0.482~1.194) 0.223 TG(mmol/L) 0.387(0.124~1.203) 0.101 HDL(mmol/L) 0.984(0.337~2.875) 0.997 LDL(mmol/L) 0.588(0.305~1.135) 0.113 HBeAg阳性 0.901(0.398~2.043) 0.809 HBV DNA(log10拷贝/ml) 1.043(0.838~1.299) 0.704 eGFR(ml·min-1·1.73 m-2) 0.968(0.950~0.984) 0.005 表 3 不同抗病毒药物对CKD发生影响
抗病毒药物 CKD组
(n=23)非CKD组
(n=353)P值 恩替卡韦(例) 14 194 0.221 替诺福韦(例) 5 42 0.449 拉米夫定(例) 0 8 替比夫定(例) 1 5 阿德福韦酯(例) 0 13 0.449 阿德福韦酯+拉米夫定(例) 1 11 0.942 阿德福韦酯+恩替卡韦(例) 1 19 0.667 阿德福韦酯→恩替卡韦(例) 0 10 阿德福韦酯→阿德福韦酯+恩替卡韦(例) 0 13 拉米夫定→恩替卡韦(例) 1 26 0.406 其他(例) 0 12 -
[1] FABRIZI F, CERUTTI R, RIDRUEJO E. Hepatitis B virus infection as a risk factor for chronic kidney disease[J]. Expert Rev Clin Pharmacol, 2019, 12(9): 867-874. DOI: 10.1080/17512433.2019.1657828. [2] HONG YS, RYU S, CHANG Y, et al. Hepatitis B virus infection and development of chronic kidney disease: A cohort study[J]. BMC Nephrol, 2018, 19(1): 353. DOI: 10.1186/s12882-018-1154-4. [3] CHACKO EC, SURRUN SK, MUBARACK SANI TP, et al. Chronic viral hepatitis and chronic kidney disease[J]. Postgrad Med J, 2010, 86(1018): 486-492. DOI: 10.1136/pgmj.2009.092775. [4] GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017[J]. Lancet, 2020, 395(10225): 709-733. DOI: 10.1016/S0140-6736(20)30045-3. [5] Chinese Society of Infectious Diseases, Chinese Medical Association, Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B (version 2019)[J]. J Clin Hepatol, 2019, 35(12): 2648-2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007.中华医学会感染病学分会, 中华医学会肝病学分会. 慢性乙型肝炎防治指南(2019年版)[J]. 临床肝胆病杂志, 2019, 35(12): 2648-2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007. [6] Chinese Society of Hepatology, Chinese Medical Association. Chinese guidelines on the management of liver cirrhosis[J]. J Clin Hepatol, 2019, 35(11): 2408-2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006.中华医学会肝病学分会. 肝硬化诊治指南[J]. 临床肝胆病杂志, 2019, 35(11): 2408-2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006. [7] STEVENS PE, LEVIN A, Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: Synopsis of the kidney disease: Improving global outcomes 2012 clinical practice guideline[J]. Ann Intern Med, 2013, 158(11): 825-830. DOI: 10.7326/0003-4819-158-11-201306040-00007. [8] LEVEY AS, BOSCH JP, LEWIS JB, et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group[J]. Ann Intern Med, 1999, 130(6): 461-470. DOI: 10.7326/0003-4819-130-6-199903160-00002. [9] CARNEY EF. Glomerular filtration rate: CKD risk factors are associated with increased single-nephron GFR[J]. Nat Rev Nephrol, 2017, 13(8): 443. DOI: 10.1038/nrneph.2017.95. [10] ISHANI A, XUE JL, HIMMELFARB J, et al. Acute kidney injury increases risk of ESRD among elderly[J]. J Am Soc Nephrol, 2009, 20(1): 223-228. DOI: 10.1681/ASN.2007080837. [11] LOW S, LIM SC, ZHANG X, et al. Development and validation of a predictive model for chronic kidney disease progression in type 2 diabetes mellitus based on a 13-year study in Singapore[J]. Diabetes Res Clin Pract, 2017, 123: 49-54. DOI: 10.1016/j.diabres.2016.11.008. [12] CHEN PM, WADA T, CHIANG CK. Prognostic value of proteinuria and glomerular filtration rate on Taiwanese patients with diabetes mellitus and advanced chronic kidney disease: A single center experience[J]. Clin Exp Nephrol, 2017, 21(2): 307-315. DOI: 10.1007/s10157-016-1290-8. [13] KEANE WF, ZHANG Z, LYLE PA, et al. Risk scores for predicting outcomes in patients with type 2 diabetes and nephropathy: The RENAAL study[J]. Clin J Am Soc Nephrol, 2006, 1(4): 761-767. DOI: 10.2215/CJN.01381005. [14] KIKUCHI H, KANDA E, MANDAI S, et al. Combination of low body mass index and serum albumin level is associated with chronic kidney disease progression: The chronic kidney disease-research of outcomes in treatment and epidemiology (CKD-ROUTE) study[J]. Clin Exp Nephrol, 2017, 21(1): 55-62. DOI: 10.1007/s10157-016-1251-2. [15] TRAWALÉ JM, PARADIS V, RAUTOU PE, et al. The spectrum of renal lesions in patients with cirrhosis: A clinicopathological study[J]. Liver Int, 2010, 30(5): 725-732. DOI: 10.1111/j.1478-3231.2009.02182.x. [16] MORINAGA J, KADOMATSU T, MIYATA K, et al. Angiopoietin-like protein 2 increases renal fibrosis by accelerating transforming growth factor-β signaling in chronic kidney disease[J]. Kidney Int, 2016, 89(2): 327-341. DOI: 10.1016/j.kint.2015.12.021. [17] SI J, YU C, GUO Y, et al. Chronic hepatitis B virus infection and total and cause-specific mortality: A prospective cohort study of 0.5 million people[J]. BMJ Open, 2019, 9(4): e027696. DOI: 10.1136/bmjopen-2018-027696. [18] SARAFIDIS PA, RUILOPE LM. Insulin resistance, hyperinsulinemia, and renal injury: Mechanisms and implications[J]. Am J Nephrol, 2006, 26(3): 232-244. DOI: 10.1159/000093632. [19] LAMPERTICO P, CHAN HL, JANSSEN HL, et al. Review article: Long-term safety of nucleoside and nucleotide analogues in HBV-monoinfected patients[J]. Aliment Pharmacol Ther, 2016, 44(1): 16-34. DOI: 10.1111/apt.13659. [20] HAGER MR, NARLA AD, TANNOCK LR. Dyslipidemia in patients with chronic kidney disease[J]. Rev Endocr Metab Disord, 2017, 18(1): 29-40. DOI: 10.1007/s11154-016-9402-z. -



 PDF下载 ( 2006 KB)
PDF下载 ( 2006 KB)


 下载:
下载: