间充质干细胞及其外泌体在药物性肝损伤治疗中的作用
DOI: 10.12449/JCH240333
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:邢国静负责课题设计,撰写论文;王丽菲、罗龙龙、王顺娜、郑晓凤参与修改论文;卢利霞、张久聪负责拟定写作思路,指导撰写文章并最后定稿。
Role of mesenchymal stem cells and their exosomes in the treatment of drug-induced liver injury
-
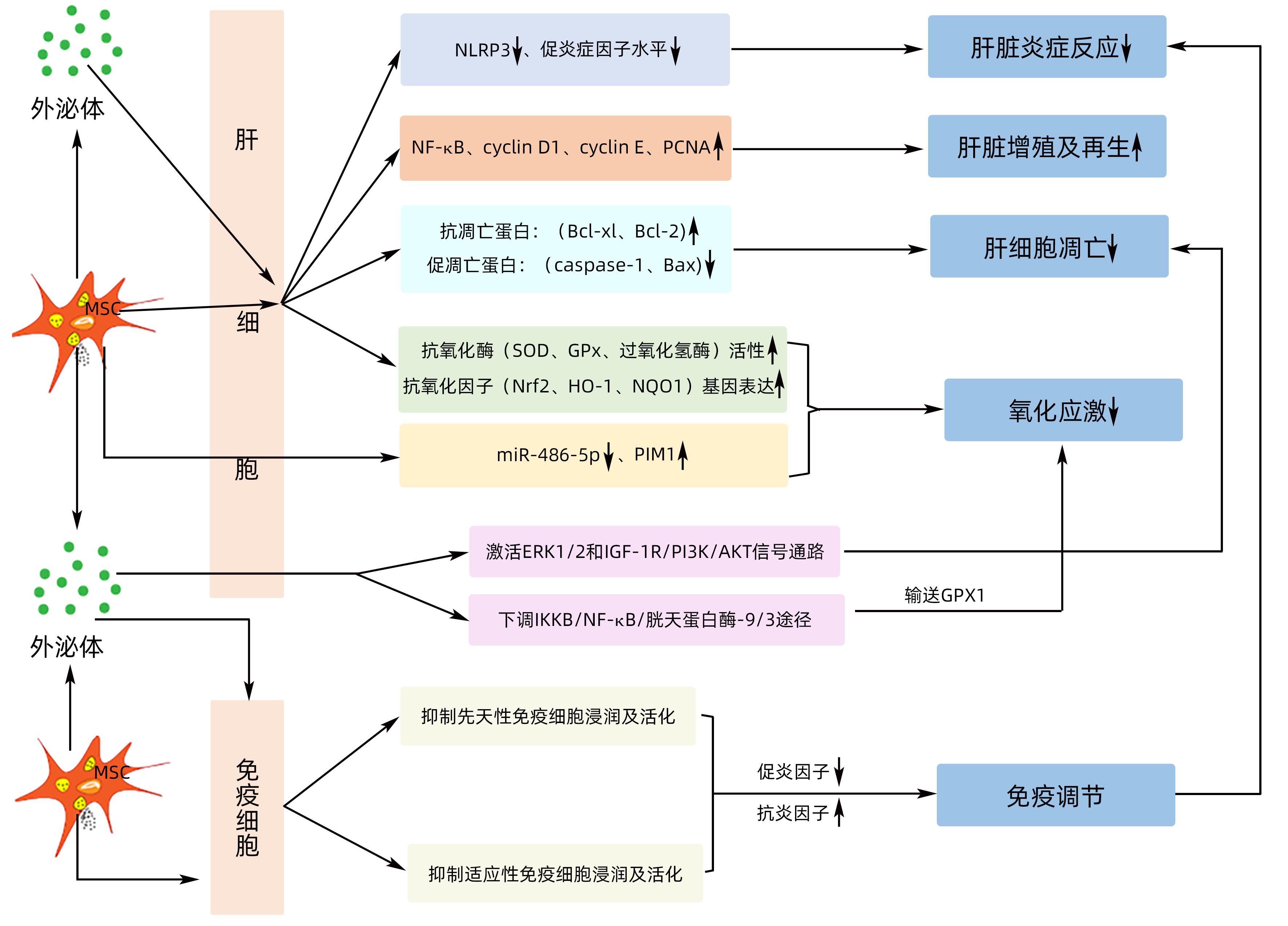
摘要: 药物性肝损伤(DILI)的发生率呈逐年上升趋势且损伤机制并不明确,针对DILI的治疗药物、肝脏支持系统及肝移植均有一定的局限性。因此,寻找更安全有效的治疗方法已成为当下研究的热点。间充质干细胞及其外泌体可通过减轻肝脏炎症反应,促进肝细胞增殖及再生、抗肝细胞凋亡,改善氧化应激和免疫调节等机制减轻肝损伤。本文就间充质干细胞及其外泌体在药物性肝损伤治疗中的作用进行简要综述,以期为进一步研究提供参考。Abstract: The incidence rate of drug-induced liver injury (DILI) is increasing year by year with unknown mechanisms, and the treatment methods for DILI mainly include drugs, liver support systems, and liver transplantation, all of which have certain limitations. Therefore, the search for safer and more effective treatment methods has become a research hotspot at present. Studies have shown that mesenchymal stem cells and their exosomes can alleviate liver injury by reducing liver inflammation, promoting hepatocyte proliferation and regeneration, inhibiting the apoptosis of hepatocytes, improving oxidative stress, and regulating immunity. This article briefly reviews the role of mesenchymal stem cells and their exosomes in the treatment of DILI, so as to provide a reference for further research.
-
Key words:
- Mesenchymal Stem Cells /
- Exosomes /
- Drug Induced Liver Injury
-
[1] Professional Committee of Prevention and Treatment of Pharmaceutical Liver Injury of China Medical Biotechnology Association, Pharmaceutical Hepatology Group of Liver Disease Branch of Chinese Medical Association. Chinese guideline for diagnosis and management of drug-induced liver injury(2023 version)[J]. Chin J Gastroenterol, 2022, 27( 6): 341- 375. DOI: 10.3760/cma.j.cn501113-20230419-00176.中国医药生物技术协会药物性肝损伤防治技术专业委员会, 中华医学会肝病学分会药物性肝病学组. 中国药物性肝损伤诊治指南(2023年版)[J]. 胃肠病学, 2022, 27( 6): 341- 375. DOI: 10.3760/cma.j.cn501113-20230419-00176. [2] LI X, TANG J, MAO Y. Incidence and risk factors of drug-induced liver injury[J]. Liver Int, 2022, 42( 9): 1999- 2014. DOI: 10.1111/liv.15262. [3] HU C, ZHAO L, WU Z, et al. Transplantation of mesenchymal stem cells and their derivatives effectively promotes liver regeneration to attenuate acetaminophen-induced liver injury[J]. Stem Cell Res Ther, 2020, 11( 1): 88. DOI: 10.1186/s13287-020-01596-9. [4] HU PF, XIE WF. Corticosteroid therapy in drug-induced liver injury: Pros and cons[J]. J Dig Dis, 2019, 20( 3): 122- 126. DOI: 10.1111/1751-2980.12697. [5] CHALASANI NP, MADDUR H, RUSSO MW, et al. ACG clinical guideline: diagnosis and management of idiosyncratic drug-induced liver injury[J]. Am J Gastroenterol, 2021, 116( 5): 878- 898. DOI: 10.14309/ajg.0000000000001259. [6] ZHANG J, CHAN HF, WANG H, et al. Stem cell therapy and tissue engineering strategies using cell aggregates and decellularized scaffolds for the rescue of liver failure[J]. J Tissue Eng, 2021, 12: 2041731420986711. DOI: 10.1177/2041731420986711. [7] HADE MD, SUIRE CN, SUO Z. Mesenchymal stem cell-derived exosomes: applications in regenerative medicine[J]. Cells, 2021, 10( 8): 1959. DOI: 10.3390/cells10081959. [8] SALEHINEJAD P, MOSHREFI M, ESLAMINEJAD T. An overview on mesenchymal stem cells derived from extraembryonic tissues: supplement sources and isolation methods[J]. Stem Cells Cloning, 2020, 13: 57- 65. DOI: 10.2147/SCCAA.S248519. [9] ABDAL DAYEM A, LEE SB, KIM K, et al. Production of mesenchymal stem cells through stem cell reprogramming[J]. Int J Mol Sci, 2019, 20( 8): 1922. DOI: 10.3390/ijms20081922. [10] MARINESCU CI, PREDA MB, BURLACU A. A procedure for in vitro evaluation of the immunosuppressive effect of mouse mesenchymal stem cells on activated T cell proliferation[J]. Stem Cell Res Ther, 2021, 12( 1): 319. DOI: 10.1186/s13287-021-02344-3. [11] MALEKPOUR K, HAZRATI A, ZAHAR M, et al. The potential use of mesenchymal stem cells and their derived exosomes for orthopedic diseases treatment[J]. Stem Cell Rev Rep, 2022, 18( 3): 933- 951. DOI: 10.1007/s12015-021-10185-z. [12] ARAVINDHAN S, EJAM SS, LAFTA MH, et al. Mesenchymal stem cells and cancer therapy: insights into targeting the tumour vasculature[J]. Cancer Cell Int, 2021, 21( 1): 158. DOI: 10.1186/s12935-021-01836-9. [13] HAN Y, LI X, ZHANG Y, et al. Mesenchymal stem cells for regenerative medicine[J]. Cells, 2019, 8( 8): 886. DOI: 10.3390/cells8080886. [14] DWIVEDI M, GHOSH D, SAHA A, et al. Biochemistry of exosomes and their theranostic potential in human diseases[J]. Life Sci, 2023, 315: 121369. DOI: 10.1016/j.lfs.2023.121369. [15] KALLURI R, LEBLEU VS. The biology, function, and biomedical applications of exosomes[J]. Science, 2020, 367( 6478): eaau6977. DOI: 10.1126/science.aau6977. [16] GURUNATHAN S, KANG MH, JEYARAJ M, et al. Review of the isolation, characterization, biological function, and multifarious therapeutic approaches of exosomes[J]. Cells, 2019, 8( 4): 307. DOI: 10.3390/cells8040307. [17] YIN K, WANG S, ZHAO RC. Exosomes from mesenchymal stem/stromal cells: a new therapeutic paradigm[J]. Biomark Res, 2019, 7: 8. DOI: 10.1186/s40364-019-0159-x. [18] HA DH, KIM HK, LEE J, et al. Mesenchymal stem/stromal cell-derived exosomes for immunomodulatory therapeutics and skin regeneration[J]. Cells, 2020, 9( 5): 1157. DOI: 10.3390/cells9051157. [19] SQUILLARO T, PELUSO G, GALDERISI U. Clinical trials with mesenchymal stem cells: an update[J]. Cell Transplant, 2016, 25( 5): 829- 848. DOI: 10.3727/096368915X689622. [20] SALOMONE F, BARBAGALLO I, PUZZO L, et al. Efficacy of adipose tissue-mesenchymal stem cell transplantation in rats with acetaminophen liver injury[J]. Stem Cell Res, 2013, 11( 3): 1037- 1044. DOI: 10.1016/j.scr.2013.07.003. [21] YU M, ZHOU M, LI J, et al. Notch-activated mesenchymal stromal/stem cells enhance the protective effect against acetaminophen-induced acute liver injury by activating AMPK/SIRT1 pathway[J]. Stem Cell Res Ther, 2022, 13( 1): 318. DOI: 10.1186/s13287-022-02999-6. [22] LIU Y, LOU G, LI A, et al. AMSC-derived exosomes alleviate lipopolysaccharide/d-galactosamine-induced acute liver failure by miR-17-mediated reduction of TXNIP/NLRP3 inflammasome activation in macrophages[J]. EBioMedicine, 2018, 36: 140- 150. DOI: 10.1016/j.ebiom.2018.08.054. [23] ZHANG S, JIANG L, HU H, et al. Pretreatment of exosomes derived from hUCMSCs with TNF-α ameliorates acute liver failure by inhibiting the activation of NLRP3 in macrophage[J]. Life Sci, 2020, 246: 117401. DOI: 10.1016/j.lfs.2020.117401. [24] MEIRELLES LDA S, FONTES AM, COVAS DT, et al. Mechanisms involved in the therapeutic properties of mesenchymal stem cells[J]. Cytokine Growth Factor Rev, 2009, 20( 5-6): 419- 427. DOI: 10.1016/j.cytogfr.2009.10.002. [25] HUANG YL, de GREGORIO C, SILVA V, et al. Administration of secretome derived from human mesenchymal stem cells induces hepatoprotective effects in models of idiosyncratic drug-induced liver injury caused by amiodarone or tamoxifen[J]. Cells, 2023, 12( 4): 636. DOI: 10.3390/cells12040636. [26] TAN CY, LAI RC, WONG W, et al. Mesenchymal stem cell-derived exosomes promote hepatic regeneration in drug-induced liver injury models[J]. Stem Cell Res Ther, 2014, 5( 3): 76. DOI: 10.1186/scrt465. [27] LIU M, HE J, ZHENG S, et al. Human umbilical cord mesenchymal stem cells ameliorate acute liver failure by inhibiting apoptosis, inflammation and pyroptosis[J]. Ann Transl Med, 2021, 9( 21): 1615. DOI: 10.21037/atm-21-2885. [28] ZHAO S, LIU Y, PU Z. Bone marrow mesenchymal stem cell-derived exosomes attenuate D-GaIN/LPS-induced hepatocyte apoptosis by activating autophagy in vitro[J]. Drug Des Devel Ther, 2019, 13: 2887- 2897. DOI: 10.2147/DDDT.S220190. [29] ZHANG XC. The effect and mechanisms of human umbilical cord mesenchymal sfem cells derived exosomes in reparation of acute liver failure[D]. Nanchang: Nanchang University, 2022.张乡城. 人脐带间充质干细胞外泌体(hUCMSC-Exo)治疗小鼠急性肝衰竭的潜能及机制研究[D]. 南昌: 南昌大学, 2022. [30] HUANG YJ, CHEN P, LEE CY, et al. Protection against acetaminophen-induced acute liver failure by omentum adipose tissue derived stem cells through the mediation of Nrf2 and cytochrome P450 expression[J]. J Biomed Sci, 2016, 23: 5. DOI: 10.1186/s12929-016-0231-x. [31] MA N, LI S, LIN C, et al. Mesenchymal stem cell conditioned medium attenuates oxidative stress injury in hepatocytes partly by regulating the miR-486-5p/PIM1 axis and the TGF-β/Smad pathway[J]. Bioengineered, 2021, 12( 1): 6434- 6447. DOI: 10.1080/21655979.2021.1972196. [32] JIANG W, TAN Y, CAI M, et al. Human umbilical cord MSC-derived exosomes suppress the development of CCl4-induced liver injury through antioxidant effect[J]. Stem Cells Int, 2018, 2018: 6079642. DOI: 10.1155/2018/6079642. [33] YAN Y, JIANG W, TAN Y, et al. hucMSC exosome-derived GPX1 is required for the recovery of hepatic oxidant injury[J]. Mol Ther, 2017, 25( 2): 465- 479. DOI: 10.1016/j.ymthe.2016.11.019. [34] RYU KH, KIM SY, KIM YR, et al. Tonsil-derived mesenchymal stem cells alleviate concanavalin A-induced acute liver injury[J]. Exp Cell Res, 2014, 326( 1): 143- 154. DOI: 10.1016/j.yexcr.2014.06.007. [35] WANG J, LIU Y, DING H, et al. Mesenchymal stem cell-secreted prostaglandin E2 ameliorates acute liver failure via attenuation of cell death and regulation of macrophage polarization[J]. Stem Cell Res Ther, 2021, 12( 1): 15. DOI: 10.1186/s13287-020-02070-2. [36] MILOSAVLJEVIC N, GAZDIC M, SIMOVIC MARKOVIC B, et al. Mesenchymal stem cells attenuate acute liver injury by altering ratio between interleukin 17 producing and regulatory natural killer T cells[J]. Liver Transpl, 2017, 23( 8): 1040- 1050. DOI: 10.1002/lt.24784. [37] ZHAO X, SHI X, ZHANG Z, et al. Combined treatment with MSC transplantation and neutrophil depletion ameliorates D-GalN/LPS-induced acute liver failure in rats[J]. Clin Res Hepatol Gastroenterol, 2016, 40( 6): 730- 738. DOI: 10.1016/j.clinre.2016.04.003. [38] ZHOU JH, LU X, YAN CL, et al. Mesenchymal stromal cell-dependent immunoregulation in chemically-induced acute liver failure[J]. World J Stem Cells, 2021, 13( 3): 208- 220. DOI: 10.4252/wjsc.v13.i3.208. [39] SHAO M, XU Q, WU Z, et al. Exosomes derived from human umbilical cord mesenchymal stem cells ameliorate IL-6-induced acute liver injury through miR-455-3p[J]. Stem Cell Res Ther, 2020, 11( 1): 37. DOI: 10.1186/s13287-020-1550-0. [40] QIN YY, XU LF, WANG Q, et al. Effect of exosomes derived from bone marrow mesenchymal stem cells on the polarization of mouse liver Kupffer cells[J]. Acta Anatomica Sinica, 2022, 53( 4): 447- 452. DOI: 10.16098/j.issn.0529-1356.2022.04.007.秦阳阳, 许龙飞, 王琪, 等. 骨髓间充质干细胞来源的外泌体对小鼠肝库普弗细胞极化的影响[J]. 解剖学报, 2022, 53( 4): 447- 452. DOI: 10.16098/j.issn.0529-1356.2022.04.007. [41] TIAN S, ZHOU X, ZHANG M, et al. Mesenchymal stem cell-derived exosomes protect against liver fibrosis via delivering miR-148a to target KLF6/STAT3 pathway in macrophages[J]. Stem Cell Res Ther, 2022, 13( 1): 330. DOI: 10.1186/s13287-022-03010-y. [42] KANG Y, SONG Y, LUO Y, et al. Exosomes derived from human umbilical cord mesenchymal stem cells ameliorate experimental non-alcoholic steatohepatitis via Nrf2/NQO-1 pathway[J]. Free Radic Biol Med, 2022, 192: 25- 36. DOI: 10.1016/j.freeradbiomed.2022.08.037. [43] NONG K, WANG W, NIU X, et al. Hepatoprotective effect of exosomes from human-induced pluripotent stem cell-derived mesenchymal stromal cells against hepatic ischemia-reperfusion injury in rats[J]. Cytotherapy, 2016, 18( 12): 1548- 1559. DOI: 10.1016/j.jcyt.2016.08.002. [44] CUI SY, TANG S, DING XL, et al. Research progress of mesenchymal stem cells and their exosomes on tumors[J]. Chin J Lung Cancer, 2022, 25( 5): 351- 357. DOI: 10.3779/j.issn.1009-3419.2022.101.20.崔舒悦, 汤帅, 丁晓玲, 等. 间充质干细胞及其外泌体对肿瘤影响的研究进展[J]. 中国肺癌杂志, 2022, 25( 5): 351- 357. DOI: 10.3779/j.issn.1009-3419.2022.101.20. [45] BARKHOLT L, FLORY E, JEKERLE V, et al. Risk of tumorigenicity in mesenchymal stromal cell-based therapies--bridging scientific observations and regulatory viewpoints[J]. Cytotherapy, 2013, 15( 7): 753- 759. DOI: 10.1016/j.jcyt.2013.03.005. [46] EZQUER F, HUANG YL, EZQUER M. New perspectives to improve mesenchymal stem cell therapies for drug-induced liver injury[J]. Int J Mol Sci, 2022, 23( 5): 2669. DOI: 10.3390/ijms23052669. -



 PDF下载 ( 908 KB)
PDF下载 ( 908 KB)

 下载:
下载:


