| [1] |
IWAKIRI Y, TREBICKA J. Portal hypertension in cirrhosis: Pathophysiological mechanisms and therapy[J]. JHEP Rep, 2021, 3( 4): 100316. DOI: 10.1016/j.jhepr.2021.100316. |
| [2] |
LUNOVA M, FRANKOVA S, GOTTFRIEDOVA H, et al. Portal hypertension is the main driver of liver stiffness in advanced liver cirrhosis[J]. Physiol Res, 2021, 70( 4): 563- 577. DOI: 10.33549/physiolres.934626. |
| [3] |
KIM KR, JUN CH, CHO KM, et al. Can proton pump inhibitors reduce rebleeding following Histoacryl sclerotherapy for gastric variceal hemorrhage?[J]. Korean J Intern Med, 2015, 30( 5): 593- 601. DOI: 10.3904/kjim.2015.30.5.593. |
| [4] |
ZHAO Y. Application value of endoscopic ultrasonography in precise devascularization of esophageal and gastric varices caused by portal hypertension[D]. Kaifeng: Henan University, 2020.
赵一. 超声内镜在门脉高压所致食管胃静脉曲张精准断流术中的应用价值[D]. 开封: 河南大学, 2020.
|
| [5] |
MA L, TSENG Y, LUO T, et al. Risk stratification for secondary prophylaxis of gastric varices due to portal hypertension[J]. Dig Liver Dis, 2019, 51( 12): 1678- 1684. DOI: 10.1016/j.dld.2019.05.020. |
| [6] |
LIU LM, ZHANG CQ. Advances in high risk factors of rebleeding after endoscopic treatment of esophagogastric variceal bleeding[J/CD]. Chin J Dig Med Imageology Electron Ed, 2022, 12( 4): 236- 240. DOI: 10.3877/cma.j.issn.2095-2015.2022.04.010. |
| [7] |
GUO YL, XU BH, LIU X, et al. Risk factors analysis of early rebleeding after endoscopic treatment of esophageal varices[J]. Chin J Dig Endosc, 2018, 35( 2): 89- 93. DOI: 10.3760/cma.j.issn.1007-5232.2018.02.003. |
| [8] |
GIRI S, SUNDARAM S, JEARTH V, et al. Predictors of early bleeding after endoscopic variceal ligation for esophageal varices: A systematic review and meta-analysis[J]. Clin Exp Hepatol, 2022, 8( 4): 267- 277. DOI: 10.5114/ceh.2022.123096. |
| [9] |
ZHANG N, PENG CY, ZHANG F, et al. Clinical value of regular endoscopic treatment for esophageal and gastric variceal bleeding in patients with liver cirrhosis[J]. Chin J Dig Endosc, 2022, 39( 5): 384- 387. DOI: 10.3760/cma.j.cn321463-20210113-00760. |
| [10] |
Chinese Society of Hepatology, Chinese Society of Gastroenterology, Chinese Society of Digestive Endoscopology of Chinese Medical Association. Guidelines on the management of esophagogastric variceal bleeding in cirrhotic portal hypertension[J]. J Clin Hepatol, 2023, 39( 3): 527- 538.
中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会消化内镜学分会. 肝硬化门静脉高压食管胃静脉曲张出血的防治指南[J]. 临床肝胆病杂志, 2023, 39( 3): 527- 538.
|
| [11] |
Esophagageal and Gastric Varices Group of Digestive Endoscopy Branch of Chinese Medical Association. Tentative guidelines for endoscopic diagnosis and treatment of varicosity and variceal bleeding in digestive tract(2009)[J]. Chin J Dig Endosc, 2010, 27( 1): 1- 4. DOI: 10.3760/cma.j.issn.1007-5232.2010.01.001. |
| [12] |
MOSTAFA EF, MOHAMMAD AN. Incidence and predictors of rebleeding after band ligation of oesophageal varices[J]. Arab J Gastroenterol, 2014, 15( 3-4): 135- 141. DOI: 10.1016/j.ajg.2014.10.002. |
| [13] |
HUANG C, SU N, WU SL, et al. Risk factors of early rebleeding after endoscopic variceal ligation[J]. J Clin Intern Med, 2019, 36( 4): 264- 266. DOI: 10.3969/j.issn.1001-9057.2019.04.014. |
| [14] |
ZHANG Y. Meta-analysis of risk factors of early rebleeding after endoscopic variceal ligation[D]. Changchun: Jilin University, 2023.
张赟. 食管静脉曲张内镜下套扎术后早期再出血危险因素的Meta分析[D]. 长春: 吉林大学, 2023.
|
| [15] |
DROLZ A, SCHRAMM C, SEIZ O, et al. Risk factors associated with bleeding after prophylactic endoscopic variceal ligation in cirrhosis[J]. Endoscopy, 2021, 53( 3): 226- 234. DOI: 10.1055/a-1214-5355. |
| [16] |
JIMÉNEZ ROSALES R, MARTÍNEZ-CARA JG, VADILLO-CALLES F, et al. Analysis of rebleeding in cases of an upper gastrointestinal bleed in a single center series[J]. Rev Esp Enferm Dig, 2019, 111( 3): 189- 192. DOI: 10.17235/reed.2018.5702/2018. |
| [17] |
ZHONG BH, WANG JP, LIN JH, et al. Risk assessment and prevention of gastroesophageal varices and variceal hemorrhage in cirrhosis[J]. Chin J Pract Intern Med, 2013, 33( 9): 690- 693.
钟碧慧, 王锦萍, 林菁华, 等. 肝硬化食管胃底静脉曲张破裂出血风险评估及预防策略[J]. 中国实用内科杂志, 2013, 33( 9): 690- 693.
|
| [18] |
ZHAO MY, WU XR, LI HX, et al. Study on correlation between serum 25-hydroxyvitamin D3 level and esophageal variceal bleeding in cirrhotic patients[J]. Chin J Hepatol, 2019, 27( 5): 358- 362. DOI: 10.3760/cma.j.issn.1007-3418.2019.05.007. |
| [19] |
ZHANG Q, SHI K, WANG XB. Developing the prediction model of esophagogastric variceal rebleeding in patients with liver cirrhosis based on artificial neural network[J]. J Clin Hepatol, 2022, 38( 11): 2493- 2498. DOI: 10.3969/j.issn.1001-5256.2022.11.011. |
| [20] |
YUAN XY, HUANG YQ, JIANG M. Influence of hyponatremia on the condition and prognosis of patients with liver cirrhosis[J]. J China Med Univ, 2019, 48( 11): 1003- 1006. DOI: 10.12007/j.issn.0258-4646.2019.11.010. |
| [21] |
ZHANG XB, LI HP, LU CL, et al. Relationship between serum sodium level and liver function and complications in patients with decompensated cirrhosis[J]. Anhui Med J, 2019, 40( 6): 673- 676. DOI: 10.3969/j.issn.1000-0399.2019.06.022. |
| [22] |
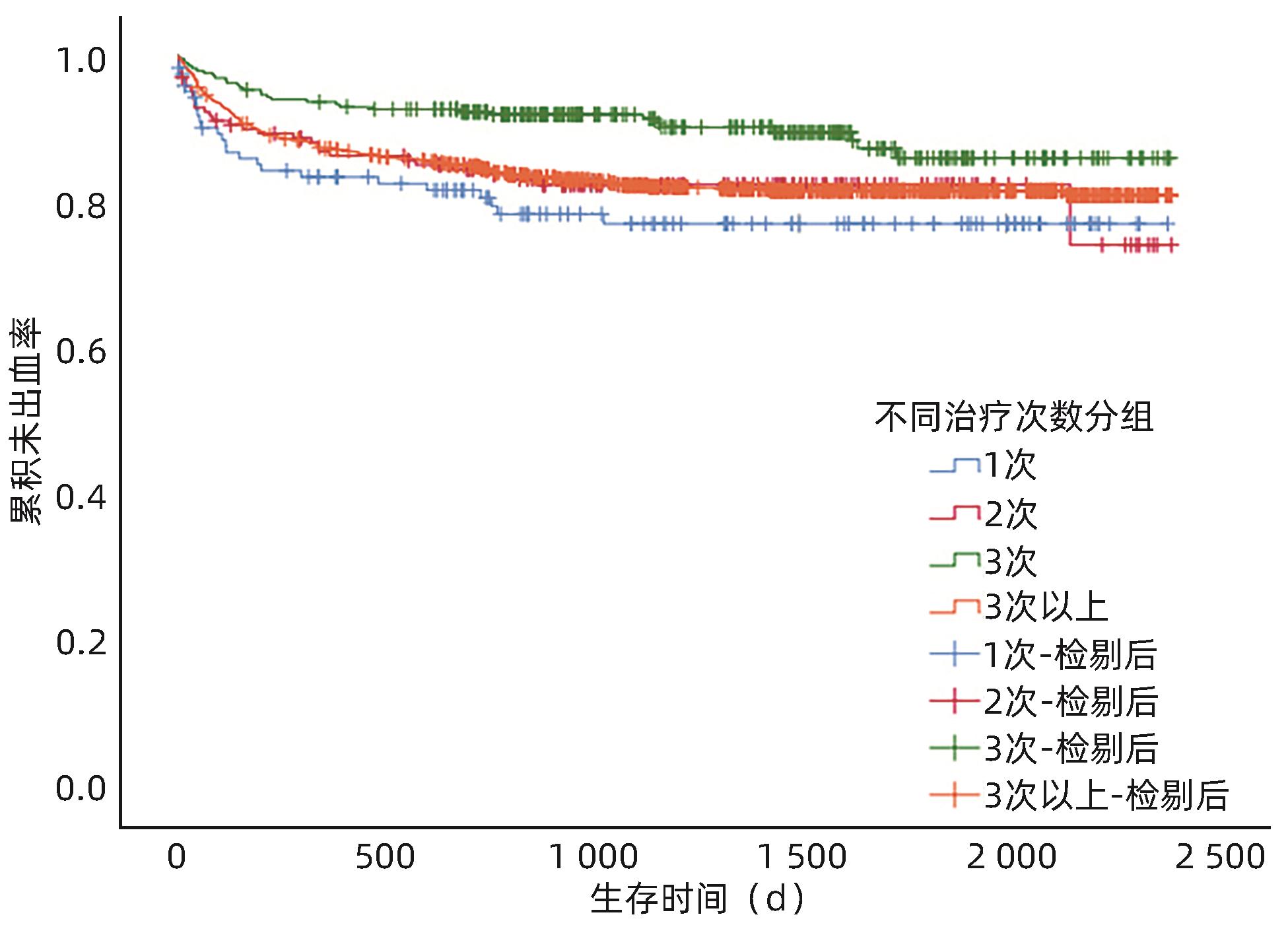
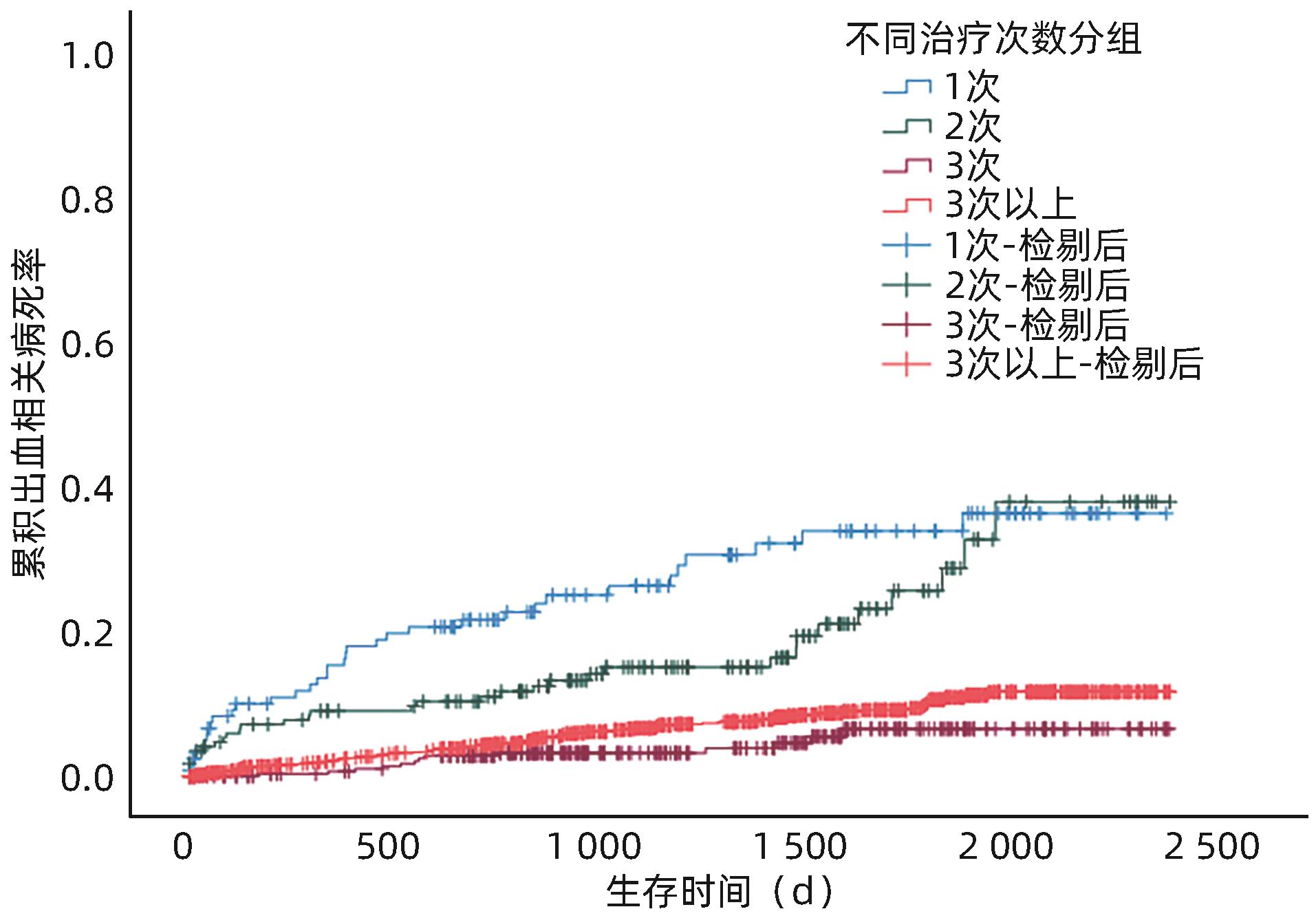
GUO H, ZHANG M, ZHANG N, et al. Number of endoscopic sessions to eradicate varices identifies high risk of rebleeding in cirrhotic patients[J]. BMC Gastroenterol, 2022, 22( 1): 213. DOI: 10.1186/s12876-022-02283-0. |
| [23] |
RÍOS E, SIERRALTA A, ABARZÚA M, et al. Comparison of band ligation with sclerotherapy for the treatment of bleeding esophageal varices[J]. Rev Med Chil, 2012, 140( 6): 713- 718. DOI: 10.4067/s0034-98872012000600003. |
| [24] |
YANG YJ. Comparative analysis of ligation, sclerosing agent and drug therapy in patients with esophageal varices bleeding[J]. Guide China Med, 2011, 9( 19): 288- 289.
杨悦军. 食管静脉曲张破裂出血患者套扎术、硬化剂、药物治疗方法比较分析[J]. 中国医药指南, 2011, 9( 19): 288- 289.
|
| [25] |
XIANG Y, WANG X, MEI XC, et al. Comparative analysis of endoscopic ligation and tissue adhesive injection for tortuous gastric varices[J]. Chin J Dig Endosc, 2021, 38( 11): 901- 906. DOI: 10.3760/cma.j.cn321463-20210223-00123. |
| [26] |
HUANG XQ, WU L, JIANG SY, et al. Clinical evaluation of different modalities in emergency endoscopic treatment of esophageal variceal bleeding[J]. J Chin Physician, 2022, 24( 5): 653- 657. DOI: 10.3760/cma.j.cn431274-20220419-00361. |
| [27] |
SONG ZM, CHEN YM, YANG M. Comparison of clinical evaluation of endoscopic therapy for esophageal variceal bleeding[J]. Chin J Curr Adv Gen Surg, 2010, 13( 3): 199- 201. DOI: 10.3969/j.issn.1009-9905.2010.03.009. |






 DownLoad:
DownLoad: