| [1] |
|
| [2] |
EGUCHI A, IWASA M. The role of elevated liver-type fatty acid-binding proteins in liver diseases[J]. Pharm Res, 2021, 38( 1): 89- 95. DOI: 10.1007/s11095-021-02998-x. |
| [3] |
WANG NN, XU LZ, WANG YP. Progress in liver type fatty acid binding protein[J]. Chin Bull Life Sci, 2012, 24( 2): 139- 144. DOI: 10.13376/j.cbls/2012.02.002. |
| [4] |
WEN YM, PARIKH CR. Current concepts and advances in biomarkers of acute kidney injury[J]. Crit Rev Clin Lab Sci, 2021, 58( 5): 354- 368. DOI: 10.1080/10408363.2021.1879000. |
| [5] |
PRIYADARSHINI G, RAJAPPA M. Predictive markers in chronic kidney disease[J]. Clin Chim Acta, 2022, 535: 180- 186. DOI: 10.1016/j.cca.2022.08.018. |
| [6] |
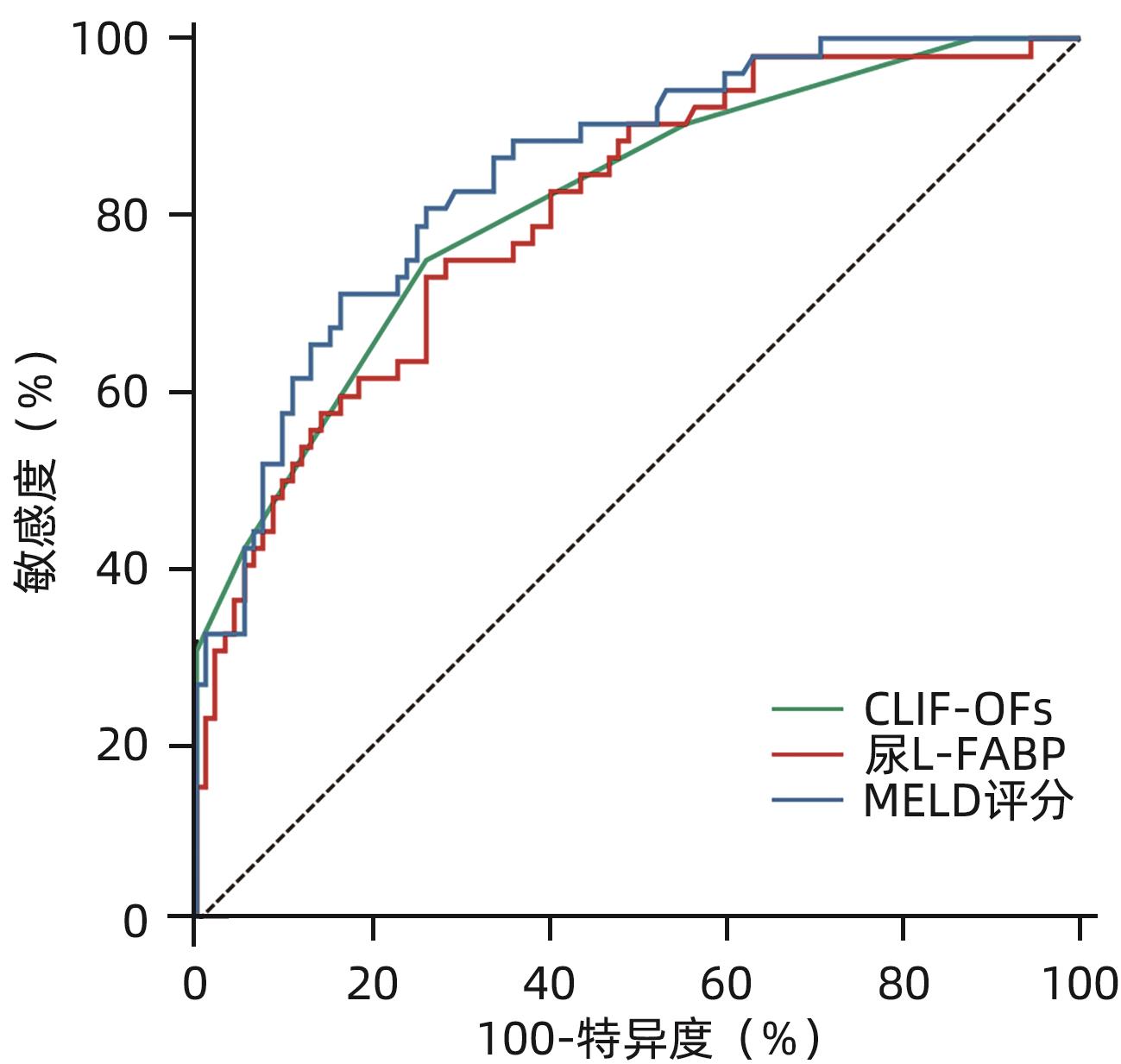
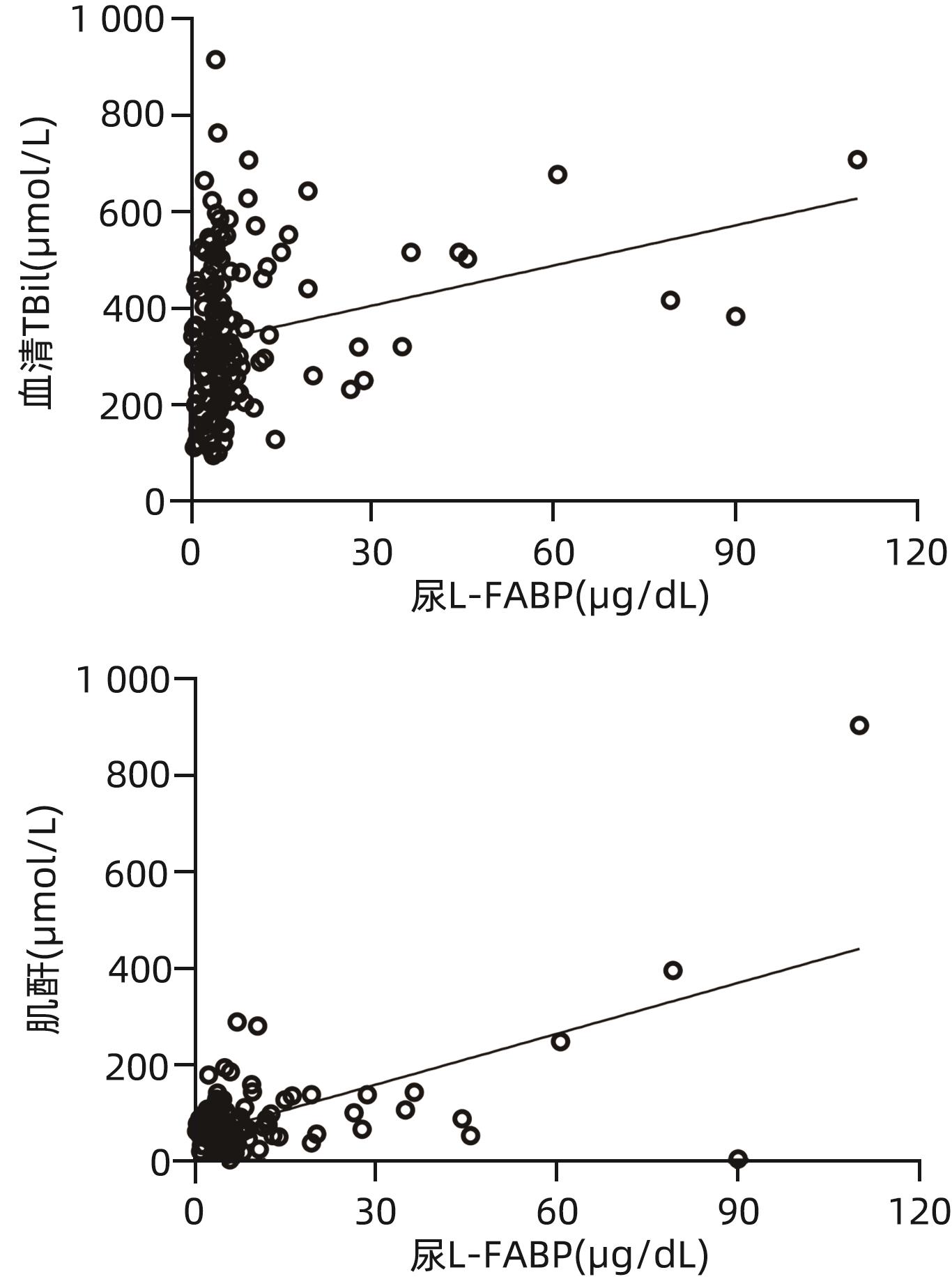
JUANOLA A, GRAUPERA I, ELIA C, et al. Urinary L-FABP is a promising prognostic biomarker of ACLF and mortality in patients with decompensated cirrhosis[J]. J Hepatol, 2022, 76( 1): 107- 114. DOI: 10.1016/j.jhep.2021.08.031. |
| [7] |
JIANG XH, CHAI SQ, HUANG Y, et al. Design for a multicentre prospective cohort for the assessment of platelet function in patients with hepatitis-B-virus-related acute-on-chronic liver failure[J]. Clin Epidemiol, 2022, 14: 997- 1011. DOI: 10.2147/CLEP.S376068. |
| [8] |
SARIN SK, CHOUDHURY A, SHARMA MK, et al. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific association for the study of the liver(APASL): An update[J]. Hepatol Int, 2019, 13( 4): 353- 390. DOI: 10.1007/s12072-019-09946-3. |
| [9] |
European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis[J]. J Hepatol, 2018, 69( 2): 406- 460. DOI: 10.1016/j.jhep.2018.03.024. |
| [10] |
ANGELI P, GINÈS P, WONG F, et al. Diagnosis and management of acute kidney injury in patients with cirrhosis: Revised consensus recommendations of the International Club of Ascites[J]. J Hepatol, 2015, 62( 4): 968- 974. DOI: 10.1016/j.jhep.2014.12.029. |
| [11] |
|
| [12] |
KULKARNI AV, SHARMA M, KUMAR P, et al. Adipocyte fatty acid-binding protein as a predictor of outcome in alcohol-induced acute-on-chronic liver failure[J]. J Clin Exp Hepatol, 2021, 11( 2): 201- 208. DOI: 10.1016/j.jceh.2020.07.010. |
| [13] |
CHEN AP, TANG YC, DAVIS V, et al. Liver fatty acid binding protein(L-Fabp) modulates murine stellate cell activation and diet-induced nonalcoholic fatty liver disease[J]. Hepatology, 2013, 57( 6): 2202- 2212. DOI: 10.1002/hep.26318. |
| [14] |
LIN JG, ZHENG SZ, ATTIE AD, et al. Perilipin 5 and liver fatty acid binding protein function to restore quiescence in mouse hepatic stellate cells[J]. J Lipid Res, 2018, 59( 3): 416- 428. DOI: 10.1194/jlr.M077487. |
| [15] |
PAWLAK M, LEFEBVRE P, STAELS B. Molecular mechanism of PPARα action and its impact on lipid metabolism, inflammation and fibrosis in non-alcoholic fatty liver disease[J]. J Hepatol, 2015, 62( 3): 720- 733. DOI: 10.1016/j.jhep.2014.10.039. |
| [16] |
LÓPEZ-VICARIO C, CHECA A, URDANGARIN A, et al. Targeted lipidomics reveals extensive changes in circulating lipid mediators in patients with acutely decompensated cirrhosis[J]. J Hepatol, 2020, 73( 4): 817- 828. DOI: 10.1016/j.jhep.2020.03.046. |
| [17] |
ZHANG Y, LIU KC, HASSAN HM, et al. Liver fatty acid binding protein deficiency provokes oxidative stress, inflammation, and apoptosis-mediated hepatotoxicity induced by pyrazinamide in zebrafish larvae[J]. Antimicrob Agents Chemother, 2016, 60( 12): 7347- 7356. DOI: 10.1128/AAC.01693-16. |
| [18] |
VOTH M, VERBOKET R, HENRICH D, et al. L-FABP and NGAL are novel biomarkers for detection of abdominal injury and hemorrhagic shock[J]. Injury, 2023, 54( 5): 1246- 1256. DOI: 10.1016/j.injury.2023.01.001. |
| [19] |
LI Q, WANG J, LU MJ, et al. Acute-on-chronic liver failure from chronic-hepatitis-B, who is the behind scenes[J]. Front Microbiol, 2020, 11: 583423. DOI: 10.3389/fmicb.2020.583423. |
| [20] |
EGUCHI A, HASEGAWA H, IWASA M, et al. Serum liver-type fatty acid-binding protein is a possible prognostic factor in human chronic liver diseases from chronic hepatitis to liver cirrhosis and hepatocellular carcinoma[J]. Hepatol Commun, 2019, 3( 6): 825- 837. DOI: 10.1002/hep4.1350. |
| [21] |
MCMAHON BA, MURRAY PT. Urinary liver fatty acid-binding protein: Another novel biomarker of acute kidney injury[J]. Kidney Int, 2010, 77( 8): 657- 659. DOI: 10.1038/ki.2010.5. |







 DownLoad:
DownLoad: