| [1] |
MALIPATI AEKJ, KAIDIRIYA KEB, XU L, et al. Research advances in the pathogenesis, phenotype-genotype relationship, and pharmacotherapy of hepatolenticular degeneration[J]. J Clin Hepatol, 2023, 39( 6): 1497- 1504. DOI: 10.3969/j.issn.1001-5256.2023.06.037. |
| [2] |
FERENCI P, STREMMEL W, CZŁONKOWSKA A, et al. Age and sex but not ATP7B genotype effectively influence the clinical phenotype of Wilson disease[J]. Hepatology, 2019, 69( 4): 1464- 1476. DOI: 10.1002/hep.30280. |
| [3] |
CAI L, HUANG XT, YE Y, et al. Role of gender and age in features of Wilson’s disease[J]. Front Neurol, 2023, 14: 1176946. DOI: 10.3389/fneur.2023.1176946. |
| [4] |
ROBERTS EA, SCHILSKY ML. Current and emerging issues in Wilson’s disease[J]. N Engl J Med, 2023, 389( 10): 922- 938. DOI: 10.1056/NEJMra1903585. |
| [5] |
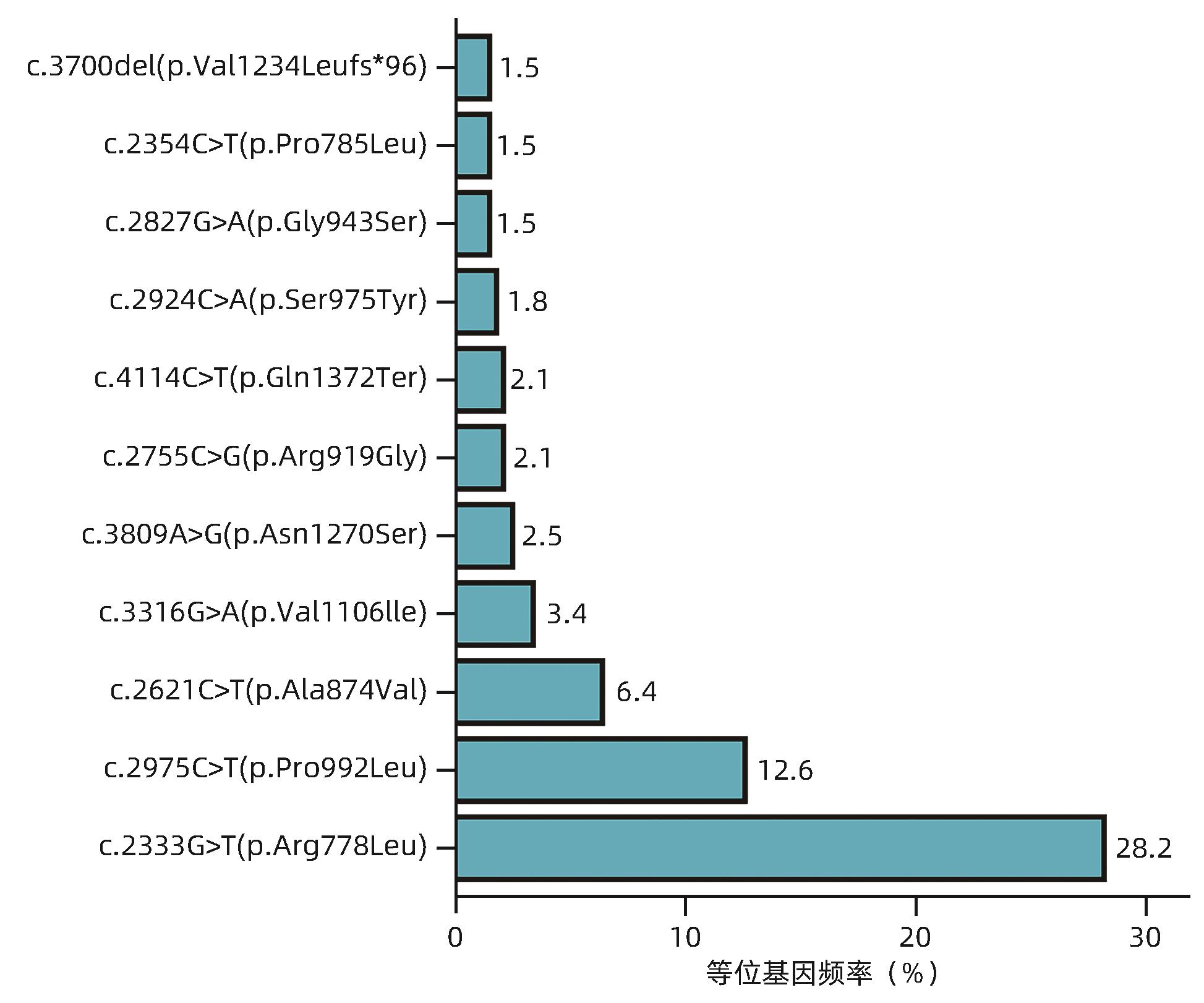
DONG Y, NI W, CHEN WJ, et al. Spectrum and classification of ATP7B variants in a large cohort of Chinese patients with Wilson’s disease guides genetic diagnosis[J]. Theranostics, 2016, 6( 5): 638- 649. DOI: 10.7150/thno.14596. |
| [6] |
DAS S, MOHAMMED A, MANDAL T, et al. Polarized trafficking and copper transport activity of ATP7B: A mutational approach to establish genotype-phenotype correlation in Wilson disease[J]. Hum Mutat, 2022, 43( 10): 1408- 1429. DOI: 10.1002/humu.24428. |
| [7] |
ZHANG TH, MAO ZQ. Clinical characteristics and gene analysis of hepatolenticular degeneration in children: A report of 70 cases[J]. Chin J Pract Pediatr, 2022, 37( 2): 135- 139. DOI: 10.19538/j.ek2022020614. |
| [8] |
XUE ZR, CHEN HY, YU L, et al. A systematic review and meta-analysis of the R778L mutation in ATP7B with Wilson disease in China[J]. Pediatr Neurol, 2023, 145: 135- 147. DOI: 10.1016/j.pediatrneurol.2023.04.026. |
| [9] |
ZHANG SJ, YANG WM, LI X, et al. Clinical and genetic characterization of a large cohort of patients with Wilson’s disease in China[J]. Transl Neurodegener, 2022, 11( 1): 13. DOI: 10.1186/s40035-022-00287-0. |
| [10] |
OKADA T, SHIONO Y, KANEKO Y, et al. High prevalence of fulminant hepatic failure among patients with mutant alleles for truncation of ATP7B in Wilson’s disease[J]. Scand J Gastroenterol, 2010, 45( 10): 1232- 1237. DOI: 10.3109/00365521.2010.492527. |
| [11] |
MERLE U, WEISS KH, EISENBACH C, et al. Truncating mutations in the Wilson disease gene ATP7B are associated with very low serum ceruloplasmin oxidase activity and an early onset of Wilson disease[J]. BMC Gastroenterol, 2010, 10: 8. DOI: 10.1186/1471-230X-10-8. |
| [12] |
FERENCI P, CACA K, LOUDIANOS G, et al. Diagnosis and phenotypic classification of Wilson disease[J]. Liver Int, 2003, 23( 3): 139- 142. DOI: 10.1034/j.1600-0676.2003.00824.x. |
| [13] |
ROZEN S, SKALETSKY H. Primer3 on the WWW for general users and for biologist programmers[J]. Methods Mol Biol, 2000, 132: 365- 386. DOI: 10.1385/1-59259-192-2: 365.
|
| [14] |
JI L, ZHANG Y, KONG L, et al. Clinical features of Wilson’s disease: An analysis of 83 cases[J]. J Clin Hepatol, 2022, 38( 8): 1843- 1846. DOI: 10.3969/j.issn.1001-5256.2022.08.023. |
| [15] |
European Association for study of Liver. EASL clinical practice guidelines: Wilson’s disease[J]. J Hepatol, 2012, 56( 3): 671- 685. DOI: 10.1016/j.jhep.2011.11.007. |
| [16] |
CHOE EJ, CHOI JW, KANG MJ, et al. A population-based epidemiology of Wilson’s disease in South Korea between 2010 and 2016[J]. Sci Rep, 2020, 10( 1): 14041. DOI: 10.1038/s41598-020-70976-1. |
| [17] |
OKADA T, SHIONO Y, HAYASHI H, et al. Mutational analysis of ATP7B and genotype-phenotype correlation in Japanese with Wilson’s disease[J]. Hum Mutat, 2000, 15( 5): 454- 462. DOI: 3.0.CO;2-J">10.1002/(SICI)1098-1004(200005)15: 5<454: AID-HUMU7>3.0.CO;2-J.
|
| [18] |
ESPINÓS C, FERENCI P. Are the new genetic tools for diagnosis of Wilson disease helpful in clinical practice?[J]. JHEP Rep, 2020, 2( 4): 100114. DOI: 10.1016/j.jhepr.2020.100114. |
| [19] |
LIU XQ, ZHANG YF, LIU TT, et al. Correlation of ATP7B genotype with phenotype in Chinese patients with Wilson disease[J]. World J Gastroenterol, 2004, 10( 4): 590- 593. DOI: 10.3748/wjg.v10.i4.590. |
| [20] |
LALIOTI V, SANDOVAL I, CASSIO D, et al. Molecular pathology of Wilson’s disease: A brief[J]. J Hepatol, 2010, 53( 6): 1151- 1153. DOI: 10.1016/j.jhep.2010.07.008. |
| [21] |
HUSTER D, HOPPERT M, LUTSENKO S, et al. Defective cellular localization of mutant ATP7B in Wilson’s disease patients and hepatoma cell lines[J]. Gastroenterology, 2003, 124( 2): 335- 345. DOI: 10.1053/gast.2003.50066. |
| [22] |
FANNI D, GEROSA C, NURCHI VM, et al. Copper-induced epigenetic changes shape the clinical phenotype in Wilson’s disease[J]. Curr Med Chem, 2021, 28( 14): 2707- 2716. DOI: 10.2174/0929867327666200730214757. |
| [23] |
KIEFFER DA, MEDICI V. Wilson disease: At the crossroads between genetics and epigenetics-a review of the evidence[J]. Liver Res, 2017, 1( 2): 121- 130. DOI: 10.1016/j.livres.2017.08.003. |
| [24] |
SCHIEFERMEIER M, KOLLEGGER H, MADL C, et al. The impact of apolipoprotein E genotypes on age at onset of symptoms and phenotypic expression in Wilson’s disease[J]. Brain, 2000, 123 Pt 3: 585- 590. DOI: 10.1093/brain/123.3.585. |
| [25] |
STUEHLER B, REICHERT J, STREMMEL W, et al. Analysis of the human homologue of the canine copper toxicosis gene MURR1 in Wilson disease patients[J]. J Mol Med(Berl), 2004, 82( 9): 629- 634. DOI: 10.1007/s00109-004-0557-9. |
| [26] |
|







 DownLoad:
DownLoad: