| [1] |
LESMANA CRA, RAHARJO M, GANI RA. Managing liver cirrhotic complications: Overview of esophageal and gastric varices[J]. Clin Mol Hepatol, 2020, 26( 4): 444- 460. DOI: 10.3350/cmh.2020.0022. |
| [2] |
LYU Y, FAN DM, HAN GH. Application status and future prospect of transjugular intrahepatic portosystemic shunt in gastroesophageal variceal bleeding in liver cirrhosis[J]. J Clin Hepatol, 2022, 38( 6): 1229- 1233. DOI: 10.3969/j.issn.1001-5256.2022.06.004. |
| [3] |
ZHANG K, LIU JL, LIU YL, et al. The 3D model was constructed by computer based on CT thin-slice scanning data to guide the clinical observation of the clinical effect of intrahepatic portal shunt through jugular vein in the treatment of portal hypertension complicated with gastrointestinal bleeding in cirrhosis[J]. Clin J Med Offic, 2023, 51( 6): 655- 656, 660. DOI: 10.16680/j.1671-3826.2023.06.28. |
| [4] |
STEPANOVA M, MISHRA A, VENKATESAN C, et al. In-hospital mortality and economic burden associated with hepatic encephalopathy in the United States from 2005 to 2009[J]. Clin Gastroenterol Hepatol, 2012, 10( 9): 1034- 1041. DOI: 10.1016/j.cgh.2012.05.016. |
| [5] |
TONG H, GAN C, WEI B, et al. Risk factors for overt hepatic encephalopathy after transjugular intrahepatic portosystemic shunt creation in patients with liver cirrhosis[J]. J Dig Dis, 2021, 22( 1): 31- 40. DOI: 10.1111/1751-2980.12957. |
| [6] |
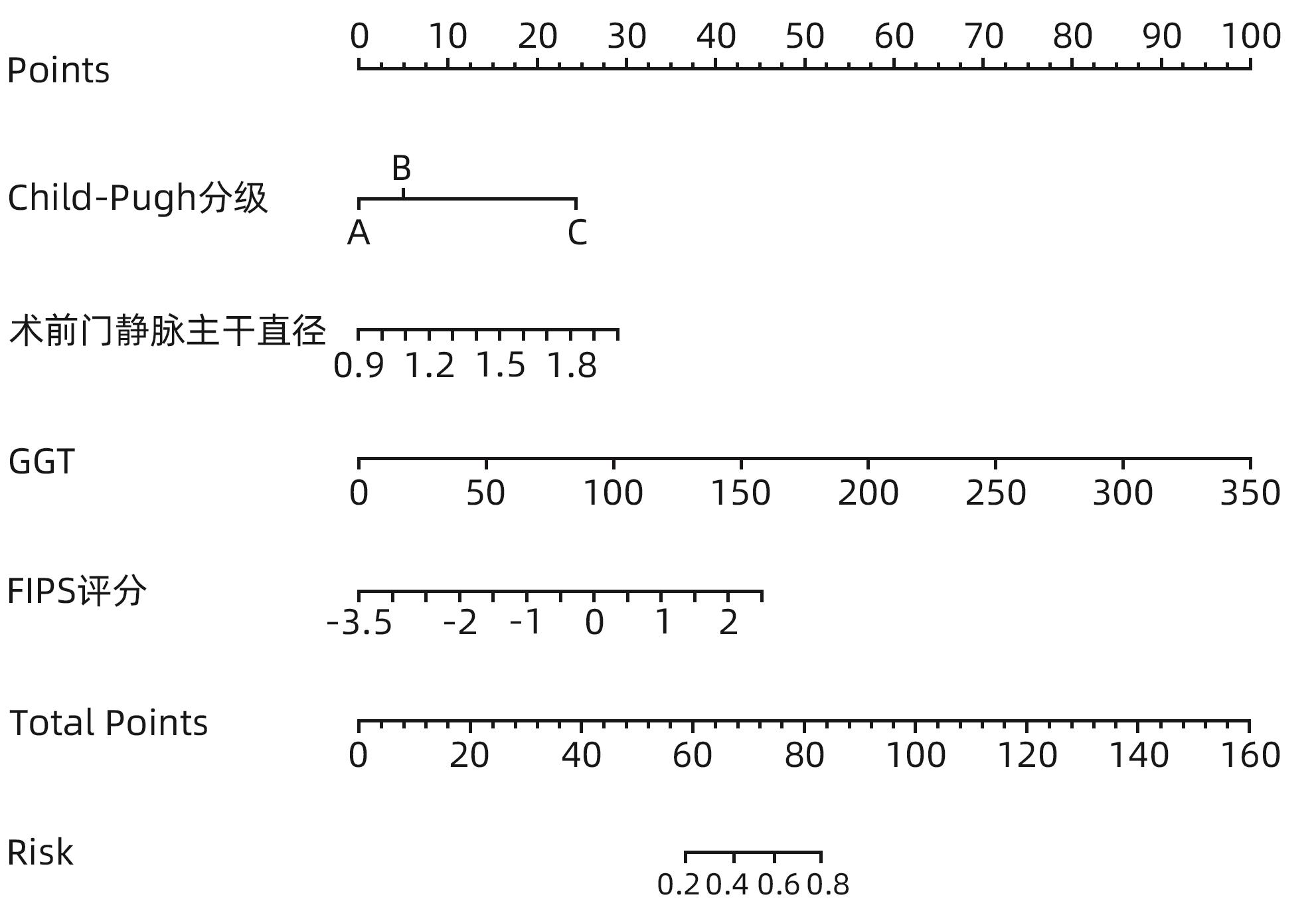
BETTINGER D, STURM L, PFAFF L, et al. Refining prediction of survival after TIPS with the novel Freiburg index of post-TIPS survival[J]. J Hepatol, 2021, 74( 6): 1362- 1372. DOI: 10.1016/j.jhep.2021.01.023. |
| [7] |
CAI WM, ZHENG BS, LIN XR, et al. Prediction of patient hepatic encephalopathy risk with Freiburg index of post-TIPS survival score following transjugular intrahepatic portosystemic shunts: A retrospective study[J]. Int J Gen Med, 2022, 15: 4007- 4016. DOI: 10.2147/IJGM.S359918. |
| [8] |
Chinese Society of Hepatology, Chinese Medical Association. Guidelines on the management of hepatic encephalopathy in cirrhosis[J]. J Clin Hepatol, 2018, 34( 10): 2076- 2089. DOI: 10.3969/j.issn.1001-5256.2018.10.007. |
| [9] |
BAJAJ JS, CORDOBA J, MULLEN KD, et al. Review article: The design of clinical trials in hepatic encephalopathy: An International Society for Hepatic Encephalopathy and Nitrogen Metabolism(ISHEN) consensus statement[J]. Aliment Pharmacol Ther, 2011, 33( 7): 739- 747. DOI: 10.1111/j.1365-2036.2011.04590.x. |
| [10] |
MA JL, CHEN X, HE LL, et al. Value of Child-Pugh score, Model for End-Stage Liver Disease score, MELD combined with serum sodium concentration, APASAL score, and R-score in predicting rebleeding and death in cirrhotic patients with esophagogastric variceal bleeding[J]. J Clin Hepatol, 2020, 36( 6): 1278- 1283. DOI: 10.3969/j.issn.1001-5256.2020.06.018. |
| [11] |
Chinese Society of Hepatology, Chinese Society of Gastroenterology, Chinese Society of Digestive Endoscopology of Chinese Medical Association. Guidelines on the management of esophagogastric variceal bleeding in cirrhotic portal hypertension[J]. J Clin Hepatol, 2023, 39( 3): 527- 538. DOI: 10.3760/cmaj.cn501113-20220824-00436. |
| [12] |
The Chinese College of Interventionalists. CCI clinical practice guidelines: Management of TIPS for portal hypertension(2019 edition)[J]. J Clin Hepatol, 2019, 35( 12): 2694- 2699. DOI: 10.3969/j.issn.1001-5256.2019.12.010. |
| [13] |
GAO Y. Predictive value of Freiburg survival index(FIPS) for survival of patients with cirrhosis and portal hypertension treated by transjugular intrahepatic portosystemic shunt[D]. Changchun: Jilin University, 2022.
高扬. 弗莱堡术后生存指数(FIPS)对经颈静脉肝内门体分流术治疗的肝硬化门脉高压患者生存期的预测价值[D]. 长春: 吉林大学, 2022.
|
| [14] |
LIU Y, ZHOU ZZ, LIU G, et al. The characteristics and risk factors of hepatic encephalopathy after emergent TIPS operation in patients with bleeding from esophageal and gastric varices[J]. Chin Hepatol, 2022, 27( 6): 658- 661. DOI: 10.3969/j.issn.1008-1704.2022.06.014. |
| [15] |
ICHAI P, SAMUEL D. Etiology and prognosis of fulminant hepatitis in adults[J]. Liver Transpl, 2008, 14( Suppl 2): S67- S79. DOI: 10.1002/lt.21612. |
| [16] |
KRISHNARAO A, GORDON FD. Prognosis of hepatic encephalopathy[J]. Clin Liver Dis, 2020, 24( 2): 219- 229. DOI: 10.1016/j.cld.2020.01.004. |
| [17] |
FONIO P, DISCALZI A, CALANDRI M, et al. Incidence of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt(TIPS) according to its severity and temporal grading classification[J]. Radiol Med, 2017, 122( 9): 713- 721. DOI: 10.1007/s11547-017-0770-6. |
| [18] |
YIN XC, ZHANG F, GUO HW, et al. A nomogram to predict the risk of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt in cirrhotic patients[J]. Sci Rep, 2020, 10( 1): 9381. DOI: 10.1038/s41598-020-65227-2. |
| [19] |
LIU J, ZHOU C, WANG Y, et al. The combination of Child-Pugh score and quantitative CT-based spleen volume could predict the risk of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt creation[J]. Abdom Radiol(NY), 2021, 46( 7): 3464- 3470. DOI: 10.1007/s00261-021-02972-6. |
| [20] |
WEISS N, BARBIER SAINT HILAIRE P, COLSCH B, et al. Cerebrospinal fluid metabolomics highlights dysregulation of energy metabolism in overt hepatic encephalopathy[J]. J Hepatol, 2016, 65( 6): 1120- 1130. DOI: 10.1016/j.jhep.2016.07.046. |
| [21] |
MCMILLIN M, FRAMPTON G, QUINN M, et al. Bile acid signaling is involved in the neurological decline in a murine model of acute liver failure[J]. Am J Pathol, 2016, 186( 2): 312- 323. DOI: 10.1016/j.ajpath.2015.10.005. |
| [22] |
AMPUERO J, RANCHAL I, DEL MAR DÍAZ-HERRERO M, et al. Role of diabetes mellitus on hepatic encephalopathy[J]. Metab Brain Dis, 2013, 28( 2): 277- 279. DOI: 10.1007/s11011-012-9354-2. |
| [23] |
YIN XC, ZHANG F, XIAO JQ, et al. Diabetes mellitus increases the risk of hepatic encephalopathy after a transjugular intrahepatic portosystemic shunt in cirrhotic patients[J]. Eur J Gastroenterol Hepatol, 2019, 31( 10): 1264- 1269. DOI: 10.1097/MEG.0000000000001452. |







 DownLoad:
DownLoad: