| [1] |
BRAY F, FERLAY J, SOERJOMATARAM I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2018, 68( 6): 394- 424. DOI: 10.3322/caac.21492. |
| [2] |
RUMGAY H, ARNOLD M, FERLAY J, et al. Global burden of primary liver cancer in 2020 and predictions to 2040[J]. J Hepatol, 2022, 77( 6): 1598- 1606. DOI: 10.1016/j.jhep.2022.08.021. |
| [3] |
SUN M, SHANG PY, BAI JT, et al. High-intensity focused ultrasound ablation combined with transcatheter arterial chemoembolization improves long-term efficacy and prognosis of primary liver cancer[J]. J Clin Lab Anal, 2021, 35( 2): e23633. DOI: 10.1002/jcla.23633. |
| [4] |
SUNG H, FERLAY J, SIEGEL RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71( 3): 209- 249. DOI: 10.3322/caac.21660. |
| [5] |
ZONG JJ, QING X, FAN Z, et al. Progress in the treatment of primary liver cancer[J]. J Southeast Univ(Med Sci Edi), 2021, 40( 4): 542- 547. DOI: 10.3969/j.issn.1671-6264.2021.04.021. |
| [6] |
GALLUZZI L, HUMEAU J, BUQUÉ A, et al. Immunostimulation with chemotherapy in the era of immune checkpoint inhibitors[J]. Nat Rev Clin Oncol, 2020, 17( 12): 725- 741. DOI: 10.1038/s41571-020-0413-z. |
| [7] |
WEI WQ, ZENG HM, ZHENG RS, et al. Cancer registration in China and its role in cancer prevention and control[J]. Lancet Oncol, 2020, 21( 7): e342- e349. DOI: 10.1016/S1470-2045(20)30073-5. |
| [8] |
LI J, LI R, ZHAO HY, et al. Organoid: A new model for antitumor drug research[J]. Pharmacol Clin Chin Mater Med, 2022, 38( 5): 200- 208. DOI: 10.13412/j.cnki.zyyl.20220926.001. |
| [9] |
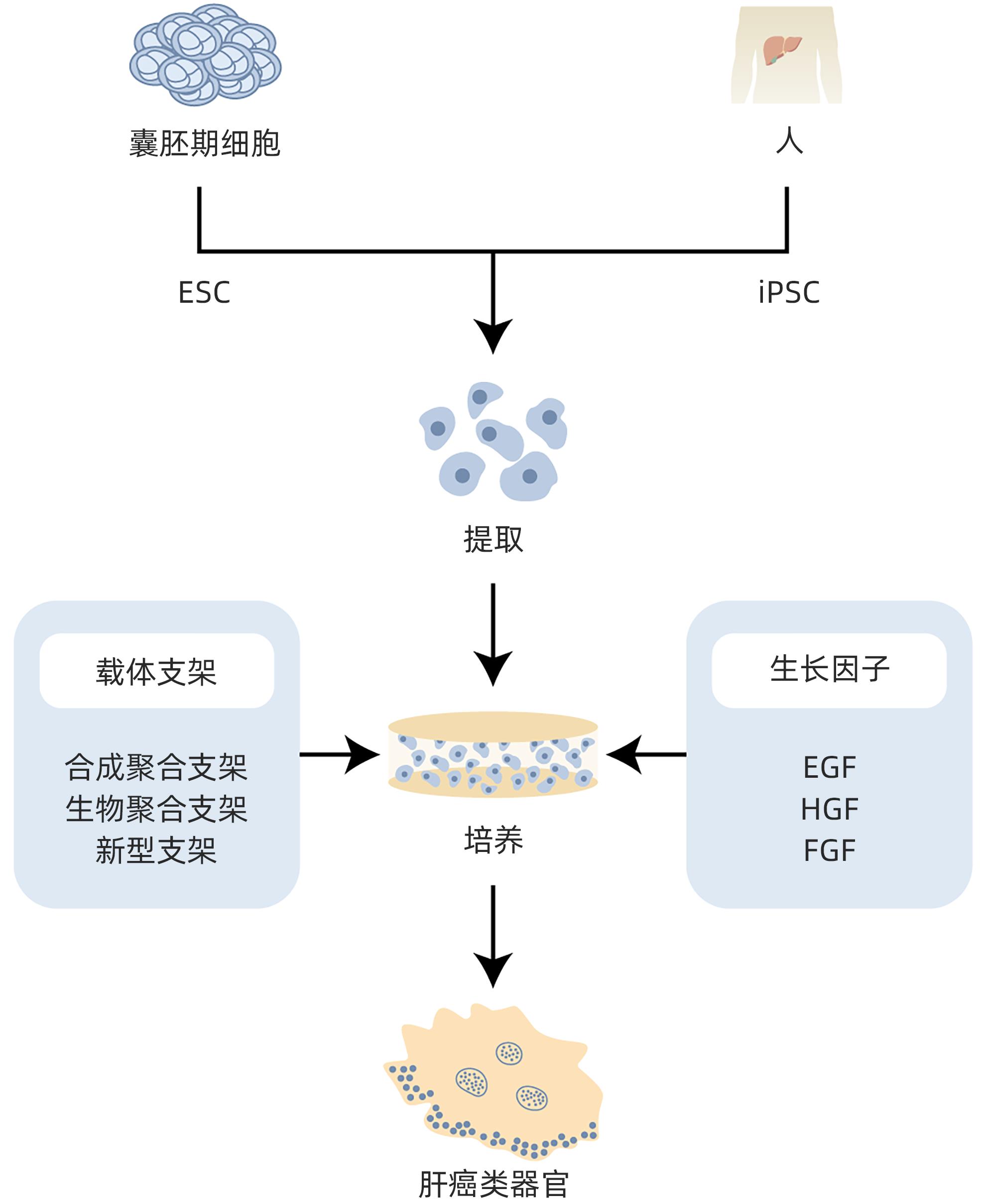
LIAO YL, LIU ZY, WANG H. Research progress on cultivation and application of liver cancer organoid[J]. J Med Postgrad, 2022, 35( 6): 664- 667. DOI: 10.16571/j.cnki.1008-8199.2022.06.018. |
| [10] |
MARQUARDT JU, ANDERSEN JB, THORGEIRSSON SS. Functional and genetic deconstruction of the cellular origin in liver cancer[J]. Nat Rev Cancer, 2015, 15( 11): 653- 667. DOI: 10.1038/nrc4017. |
| [11] |
SCHULZE K, NAULT JC, VILLANUEVA A. Genetic profiling of hepatocellular carcinoma using next-generation sequencing[J]. J Hepatol, 2016, 65( 5): 1031- 1042. DOI: 10.1016/j.jhep.2016.05.035. |
| [12] |
CAO XD, SUN MY, ZHANG HY, et al. Research progress on molecular pathogenesis of primary liver cancer[J]. J Hepatobiliary Surg, 2019, 27( 2): 153- 156. DOI: 10.3969/j.issn.1006-4761.2019.02.023. |
| [13] |
|
| [14] |
|
| [15] |
HUCH M, KOO BK. Modeling mouse and human development using organoid cultures[J]. Development, 2015, 142( 18): 3113- 3125. DOI: 10.1242/dev.118570. |
| [16] |
BI GY, ZHANG HY. Study on the formation mechanism and application of liver organoids[J]. Chin J Cell Biol, 2022, 44( 11): 2214- 2222. DOI: 10.11844/cjcb.2022.11.0018. |
| [17] |
MCCRACKEN KW, CATÁ EM, CRAWFORD CM, et al. Modelling human development and disease in pluripotent stem-cell-derived gastric organoids[J]. Nature, 2014, 516( 7531): 400- 404. DOI: 10.1038/nature13863. |
| [18] |
HATTORI N. Cerebral organoids model human brain development and microcephaly[J]. Mov Disord, 2014, 29( 2): 185. DOI: 10.1002/mds.25740. |
| [19] |
YAMADA M, UTOH R, OHASHI K, et al. Controlled formation of heterotypic hepatic micro-organoids in anisotropic hydrogel microfibers for long-term preservation of liver-specific functions[J]. Biomaterials, 2012, 33( 33): 8304- 8315. DOI: 10.1016/j.biomaterials.2012.07.068. |
| [20] |
WU FF, WU D, REN Y, et al. Generation of hepatobiliary organoids from human induced pluripotent stem cells[J]. J Hepatol, 2019, 70( 6): 1145- 1158. DOI: 10.1016/j.jhep.2018.12.028. |
| [21] |
BROUTIER L, MASTROGIOVANNI G, VERSTEGEN MM, et al. Human primary liver cancer-derived organoid cultures for disease modeling and drug screening[J]. Nat Med, 2017, 23( 12): 1424- 1435. DOI: 10.1038/nm.4438. |
| [22] |
|
| [23] |
MUN SJ, RYU JS, LEE MO, et al. Generation of expandable human pluripotent stem cell-derived hepatocyte-like liver organoids[J]. J Hepatol, 2019, 71( 5): 970- 985. DOI: 10.1016/j.jhep.2019.06.030. |
| [24] |
SUN GC, LI HY, CHEN J, et al. Research progress and application of organoids in biomedical field[J]. Clin J Med Offic, 2023, 51( 11): 1206- 1210. DOI: 10.16680/j.1671-3826.2023.11.28. |
| [25] |
BHATIA SN, UNDERHILL GH, ZARET KS, et al. Cell and tissue engineering for liver disease[J]. Sci Transl Med, 2014, 6( 245): 245sr2. DOI: 10.1126/scitranslmed.3005975. |
| [26] |
HOSSEINI V, MAROUFI NF, SAGHATI S, et al. Current progress in hepatic tissue regeneration by tissue engineering[J]. J Transl Med, 2019, 17( 1): 383. DOI: 10.1186/s12967-019-02137-6. |
| [27] |
ZHANG L, GUAN Z, YE JS, et al. Research progress in liver tissue engineering[J]. Biomed Mater Eng, 2017, 28( s1): S113- S119. DOI: 10.3233/BME-171632. |
| [28] |
TAKAHASHI K, YAMANAKA S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors[J]. Cell, 2006, 126( 4): 663- 676. DOI: 10.1016/j.cell.2006.07.024. |
| [29] |
PRIOR N, INACIO P, HUCH M. Liver organoids: From basic research to therapeutic applications[J]. Gut, 2019, 68( 12): 2228- 2237. DOI: 10.1136/gutjnl-2019-319256. |
| [30] |
NG SS, SAEB-PARSY K, BLACKFORD SJI, et al. Human iPS derived progenitors bioengineered into liver organoids using an inverted colloidal crystal poly(ethylene glycol) scaffold[J]. Biomaterials, 2018, 182: 299- 311. DOI: 10.1016/j.biomaterials.2018.07.043. |
| [31] |
TYSOE OC, JUSTIN AW, BREVINI T, et al. Isolation and propagation of primary human cholangiocyte organoids for the generation of bioengineered biliary tissue[J]. Nat Protoc, 2019, 14( 6): 1884- 1925. DOI: 10.1038/s41596-019-0168-0. |
| [32] |
VERSTEGEN MMA, WILLEMSE J, van den HOEK S, et al. Decellularization of whole human liver grafts using controlled perfusion for transplantable organ bioscaffolds[J]. Stem Cells Dev, 2017, 26( 18): 1304- 1315. DOI: 10.1089/scd.2017.0095. |
| [33] |
GEETHA BAI R, MUTHOOSAMY K, MANICKAM S, et al. Graphene-based 3D scaffolds in tissue engineering: Fabrication, applications, and future scope in liver tissue engineering[J]. Int J Nanomedicine, 2019, 14: 5753- 5783. DOI: 10.2147/IJN.S192779. |
| [34] |
WEI GF, WANG JW, LV Q, et al. Three-dimensional coculture of primary hepatocytes and stellate cells in silk scaffold improves hepatic morphology and functionality in vitro[J]. J Biomed Mater Res A, 2018, 106( 8): 2171- 2180. DOI: 10.1002/jbm.a.36421. |
| [35] |
WANG SY, WANG X, TAN ZL, et al. Human ESC-derived expandable hepatic organoids enable therapeutic liver repopulation and pathophysiological modeling of alcoholic liver injury[J]. Cell Res, 2019, 29( 12): 1009- 1026. DOI: 10.1038/s41422-019-0242-8. |
| [36] |
BROUTIER L, ANDERSSON-ROLF A, HINDLEY CJ, et al. Culture and establishment of self-renewing human and mouse adult liver and pancreas 3D organoids and their genetic manipulation[J]. Nat Protoc, 2016, 11( 9): 1724- 1743. DOI: 10.1038/nprot.2016.097. |
| [37] |
DRIEHUIS E, KRETZSCHMAR K, CLEVERS H. Establishment of patient-derived cancer organoids for drug-screening applications[J]. Nat Protoc, 2020, 15( 10): 3380- 3409. DOI: 10.1038/s41596-020-0379-4. |
| [38] |
ZHENG WJ, YAO DF, ZHANG J, et al. In-vitro construction method of liver cancer organ model: CN110004109B[P]. 2023-01-17.
郑文杰, 姚登福, 张捷, 等. 一种肝癌类器官模型的体外构建方法: CN110004109B[P]. 2023-01-17.
|
| [39] |
BROUTIER L, MASTROGIOVANNI G, VERSTEGEN MM, et al. Human primary liver cancer-derived organoid cultures for disease modeling and drug screening[J]. Nat Med, 2017, 23( 12): 1424- 1435. DOI: 10.1038/nm.4438. |
| [40] |
SHIOTA J, SAMUELSON LC, RAZUMILAVA N. Hepatobiliary organoids and their applications for studies of liver health and disease: Are we there yet?[J]. Hepatology, 2021, 74( 4): 2251- 2263. DOI: 10.1002/hep.31772. |
| [41] |
CAO WL, LIU JY, WANG L, et al. Modeling liver cancer and therapy responsiveness using organoids derived from primary mouse liver tumors[J]. Carcinogenesis, 2019, 40( 1): 145- 154. DOI: 10.1093/carcin/bgy129. |
| [42] |
FUJII M, CLEVERS H, SATO T. Modeling human digestive diseases with CRISPR-Cas9-modified organoids[J]. Gastroenterology, 2019, 156( 3): 562- 576. DOI: 10.1053/j.gastro.2018.11.048. |
| [43] |
WANG Y, TAKEISHI K, LI Z, et al. Microenvironment of a tumor-organoid system enhances hepatocellular carcinoma malignancy-related hallmarks[J]. Organogenesis, 2017, 13( 3): 83- 94. DOI: 10.1080/15476278.2017.1322243. |
| [44] |
WANG HC, CALVISI DF, CHEN X. Organoids for the study of liver cancer[J]. Semin Liver Dis, 2021, 41( 1): 19- 27. DOI: 10.1055/s-0040-1719176. |
| [45] |
WANG YX, ZHU YJ, WANG HY, et al. Advances and applications of liver organoids[J]. Chin J Cell Biol, 2021, 43( 6): 1132- 1141. DOI: 10.11844/cjcb.2021.06.0003. |
| [46] |
LI L, KNUTSDOTTIR H, HUI K, et al. Human primary liver cancer organoids reveal intratumor and interpatient drug response heterogeneity[J]. JCI Insight, 2019, 4( 2): e121490. DOI: 10.1172/jci.insight.121490. |
| [47] |
|
| [48] |
YU JH, MA S. Organoids as research models for hepatocellular carcinoma[J]. Exp Cell Res, 2022, 411( 1): 112987. DOI: 10.1016/j.yexcr.2021.112987. |
| [49] |
HU HL, GEHART H, ARTEGIANI B, et al. Long-term expansion of functional mouse and human hepatocytes as 3D organoids[J]. Cell, 2018, 175( 6): 1591- 1606. DOI: 10.1016/j.cell.2018.11.013. |
| [50] |
PENG WC, LOGAN CY, FISH M, et al. Inflammatory cytokine TNFα promotes the long-term expansion of primary hepatocytes in 3D culture[J]. Cell, 2018, 175( 6): 1607- 1619. DOI: 10.1016/j.cell.2018.11.012. |
| [51] |
SAMPAZIOTIS F, MURARO D, TYSOE OC, et al. Cholangiocyte organoids can repair bile ducts after transplantation in the human liver[J]. Science, 2021, 371( 6531): 839- 846. DOI: 10.1126/science.aaz6964. |
| [52] |
LI YQ, TANG PY, CAI SJ, et al. Organoid based personalized medicine: From bench to bedside[J]. Cell Regen, 2020, 9( 1): 21. DOI: 10.1186/s13619-020-00059-z. |
| [53] |
BROOKS A, LIANG X, ZHANG Y, et al. Liver organoid as a 3D in vitro model for drug validation and toxicity assessment[J]. Pharmacol Res, 2021, 169: 105608. DOI: 10.1016/j.phrs.2021.105608. |
| [54] |
GUAN Y, CHEN XY, WU MH, et al. The phosphatidylethanolamine biosynthesis pathway provides a new target for cancer chemotherapy[J]. J Hepatol, 2020, 72( 4): 746- 760. DOI: 10.1016/j.jhep.2019.11.007. |
| [55] |
LIN L, LEI M, LIN JM, et al. Advances and applications in liver organoid technology[J]. Sci Sin Vitae, 2023, 53( 2): 185- 195.
林丽, 雷妙, 林佳漫, 等. 肝脏类器官的研究进展及应用[J]. 中国科学: 生命科学, 2023, 53( 2): 185- 195.
|
| [56] |
LI LY, QIAN MX, CHEN IH, et al. Acquisition of cholangiocarcinoma traits during advanced hepatocellular carcinoma development in mice[J]. Am J Pathol, 2018, 188( 3): 656- 671. DOI: 10.1016/j.ajpath.2017.11.013. |
| [57] |
TIRIAC H, BELLEAU P, ENGLE DD, et al. Organoid profiling identifies common responders to chemotherapy in pancreatic cancer[J]. Cancer Discov, 2018, 8( 9): 1112- 1129. DOI: 10.1158/2159-8290.CD-18-0349. |
| [58] |
KONDO J, EKAWA T, ENDO H, et al. High-throughput screening in colorectal cancer tissue-originated spheroids[J]. Cancer Sci, 2019, 110( 1): 345- 355. DOI: 10.1111/cas.13843. |
| [59] |
NUCIFORO S, FOFANA I, MATTER MS, et al. Organoid models of human liver cancers derived from tumor needle biopsies[J]. Cell Rep, 2018, 24( 5): 1363- 1376. DOI: 10.1016/j.celrep.2018.07.001. |
| [60] |
XING JL, WANG YX, DU SD. Application and research progress of in vitro liver cancer cell culture models[J]. World Chin J Dig, 2021, 29( 11): 563- 570. DOI: 10.11569/wcjd.v29.i11.563. |
| [61] |
SAKABE K, TAKEBE T, ASAI A. Organoid medicine in hepatology[J]. Clin Liver Dis(Hoboken), 2020, 15( 1): 3- 8. DOI: 10.1002/cld.855. |
| [62] |
HUCH M, DORRELL C, BOJ SF, et al. In vitro expansion of single Lgr5 + liver stem cells induced by Wnt-driven regeneration[J]. Nature, 2013, 494( 7436): 247- 250. DOI: 10.1038/nature11826. |
| [63] |
JIN Y, KIM J, LEE JS, et al. Vascularized liver organoids generated using induced hepatic tissue and dynamic liver-specific microenvironment as a drug testing platform[J]. Adv Funct Mater, 2018, 28( 37): 1801954. DOI: 10.1002/adfm.201801954. |
| [64] |
HILMI M, VIENOT A, ROUSSEAU B, et al. Immune therapy for liver cancers[J]. Cancers(Basel), 2019, 12( 1): 77. DOI: 10.3390/cancers12010077. |
| [65] |
CAVALLONI G, PERALDO-NEIA C, VARAMO C, et al. Establishment and characterization of a human intrahepatic cholangiocarcinoma cell line derived from an Italian patient[J]. Tumour Biol, 2016, 37( 3): 4041- 4052. DOI: 10.1007/s13277-015-4215-3. |
| [66] |
GU QY, ZHANG B, SUN HY, et al. Genomic characterization of a large panel of patient-derived hepatocellular carcinoma xenograft tumor models for preclinical development[J]. Oncotarget, 2015, 6( 24): 20160- 20176. DOI: 10.18632/oncotarget.3969. |
| [67] |
HIDALGO M, AMANT F, BIANKIN AV, et al. Patient-derived xenograft models: An emerging platform for translational cancer research[J]. Cancer Discov, 2014, 4( 9): 998- 1013. DOI: 10.1158/2159-8290.CD-14-0001. |
| [68] |
HOU JJ, ZHANG HY, SUN BC, et al. The immunobiology of hepatocellular carcinoma in humans and mice: Basic concepts and therapeutic implications[J]. J Hepatol, 2020, 72( 1): 167- 182. DOI: 10.1016/j.jhep.2019.08.014. |
| [69] |
VOTANOPOULOS KI, FORSYTHE S, SIVAKUMAR H, et al. Model of patient-specific immune-enhanced organoids for immunotherapy screening: Feasibility study[J]. Ann Surg Oncol, 2020, 27( 6): 1956- 1967. DOI: 10.1245/s10434-019-08143-8. |
| [70] |
HAI J, ZHANG H, ZHOU J, et al. Generation of genetically engineered mouse lung organoid models for squamous cell lung cancers allows for the study of combinatorial immunotherapy[J]. Clin Cancer Res, 2020, 26( 13): 3431- 3442. DOI: 10.1158/1078-0432.CCR-19-1627. |







 DownLoad:
DownLoad: