| [1] |
SUNG H, FERLAY J, SIEGEL RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71( 3): 209- 249. DOI: 10.3322/caac.21660. |
| [2] |
General Office of National Health Commission. Standard for diagnosis and treatment of primary liver cancer(2022 edition)[J]. J Clin Hepatol, 2022, 38( 2): 288- 303. DOI: 10.3969/j.issn.1001-5256.2022.02.009. |
| [3] |
NGUYEN QT, TSIEN RY. Fluorescence-guided surgery with live molecular navigation: A new cutting edge[J]. Nat Rev Cancer, 2013, 13( 9): 653- 662. DOI: 10.1038/nrc3566. |
| [4] |
POMPILI M, SAVIANO A, de MATTHAEIS N, et al. Long-term effectiveness of resection and radiofrequency ablation for single hepatocellular carcinoma ≤3 cm. Results of a multicenter Italian survey[J]. J Hepatol, 2013, 59( 1): 89- 97. DOI: 10.1016/j.jhep.2013.03.009. |
| [5] |
LIVRAGHI T. Single HCC smaller than 2 cm: surgery or ablation: Interventional oncologist’s perspective[J]. J Hepatobiliary Pancreat Sci, 2010, 17( 4): 425- 429. DOI: 10.1007/s00534-009-0244-x. |
| [6] |
FENG K, YAN J, LI XW, et al. A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma[J]. J Hepatol, 2012, 57( 4): 794- 802. DOI: 10.1016/j.jhep.2012.05.007. |
| [7] |
SOLBIATI L, IERACE T, TONOLINI M, et al. Guidance and monitoring of radiofrequency liver tumor ablation with contrast-enhanced ultrasound[J]. Eur J Radiol, 2004, 51 Suppl: S19- S23. DOI: 10.1016/j.ejrad.2004.03.035. |
| [8] |
Chinese Society of Digital Medicine, Chinese Medical Association; Chinese Society of Liver Cancer, Chinese Medical Doctor Association; Clinical Precision Medicine Committee of Chinese Medical Doctor Association, et al. Three-dimensional visualization and accurate diagnosis and treatment guidelines for complex liver tumors(2019 edition)[J]. Chin J Pract Surg, 2019, 39( 8): 766- 774. DOI: 10.19538/j.cjps.issn1005-2208.2019.08.02. |
| [9] |
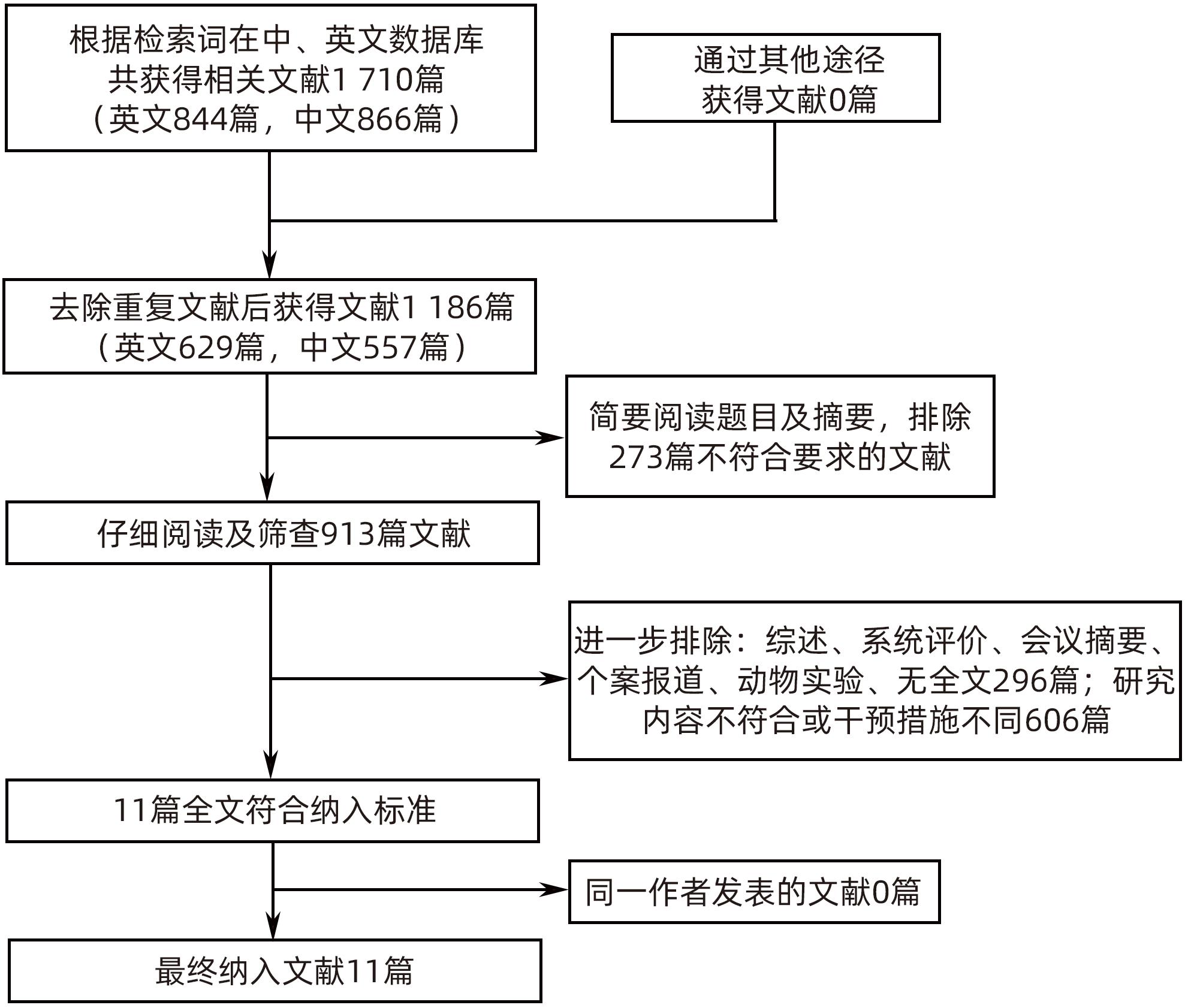
WANG C, HUANG Q, YANG J. Meta-analysis of application value of three-dimensional visualization technique in liver cancer surgery[J]. Chin J Gen Surg, 2020, 29( 1): 19- 26. DOI: 10.7659/j.issn.1005-6947.2020.01.003. |
| [10] |
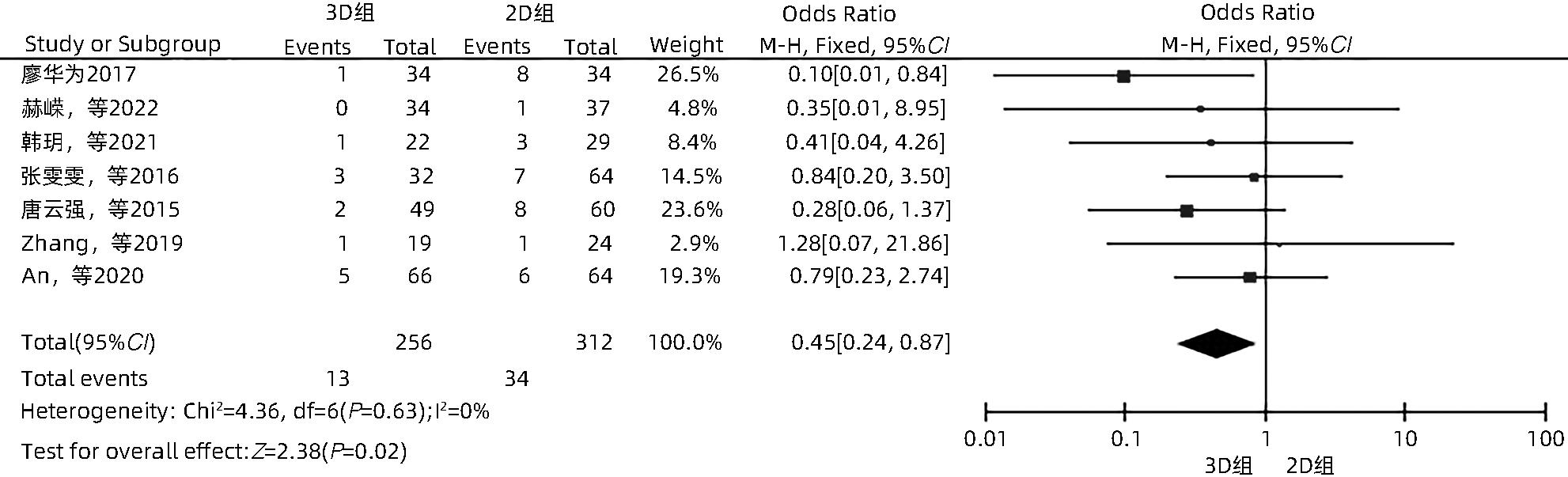
ZHANG DZ, LIANG WZ, ZHANG M, et al. Multiple antenna placement in microwave ablation assisted by a three-dimensional fusion image navigation system for hepatocellular carcinoma[J]. Int J Hyperthermia, 2019, 35( 1): 122- 132. DOI: 10.1080/02656736.2018.1484183. |
| [11] |
AHMED M, SOLBIATI L, BRACE CL, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria--a 10-year update[J]. Radiology, 2014, 273( 1): 241- 260. DOI: 10.1148/radiol.14132958. |
| [12] |
DINDO D, DEMARTINES N, CLAVIEN PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey[J]. Ann Surg, 2004, 240( 2): 205- 213. DOI: 10.1097/01.sla.0000133083.54934.ae. |
| [13] |
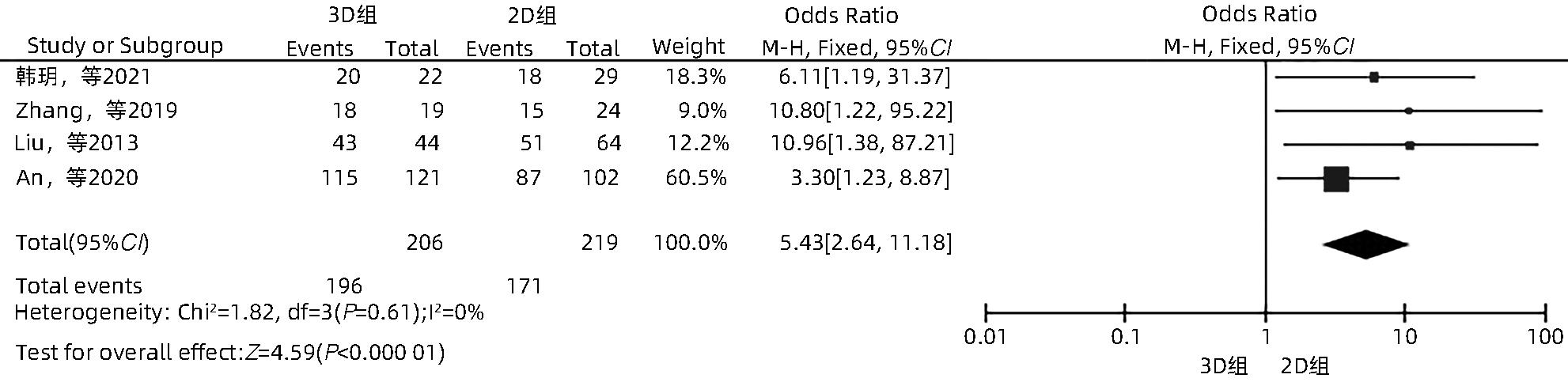
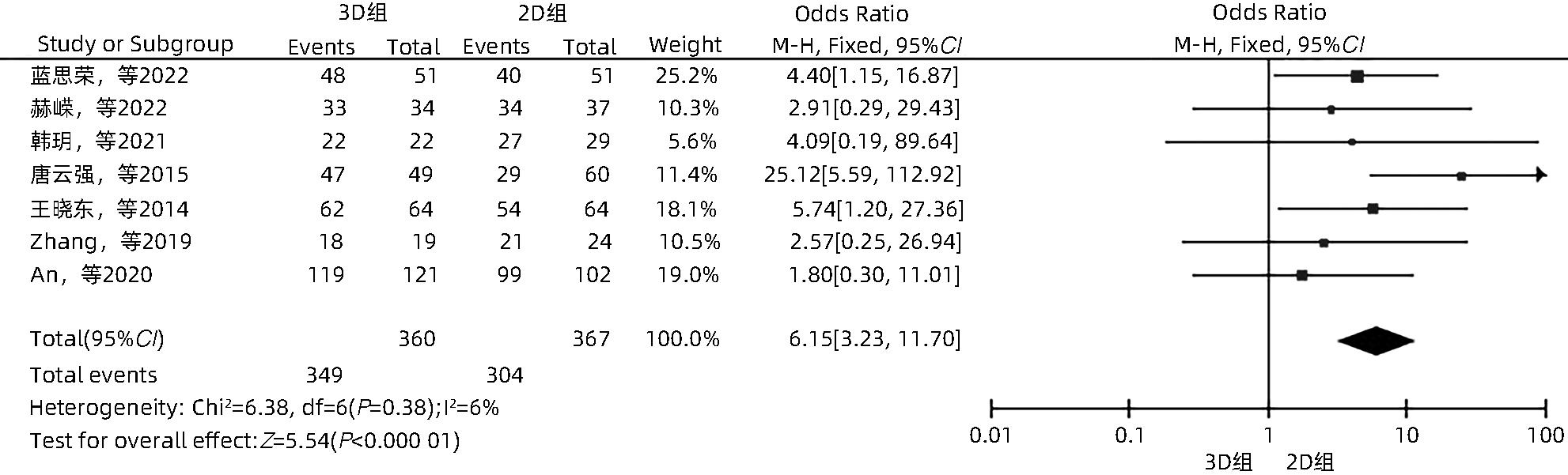
TANG YQ, JIANG P, SHI BY, et al. Three-dimensional reconstruction to improve the success rate in the first attempt of radiofrequency ablation for small hepatocellular carcinoma[J]. Chin J Hepatobiliary Surg, 2015, 21( 10): 664- 667. DOI: 10.3760/cma.j.issn.1007-8118.2015.10.005. |
| [14] |
JADAD AR, MOORE RA, CARROLL D, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary?[J]. Control Clin Trials, 1996, 17( 1): 1- 12. DOI: 10.1016/0197-2456(95)00134-4. |
| [15] |
LUCHINI C, STUBBS B, SOLMI M, et al. Assessing the quality of studies in meta-analyses: Advantages and limitations of the Newcastle Ottawa Scale[J]. World J Meta Anal, 2017, 5( 4): 80. DOI: 10.13105/wjma.v5.i4.80. |
| [16] |
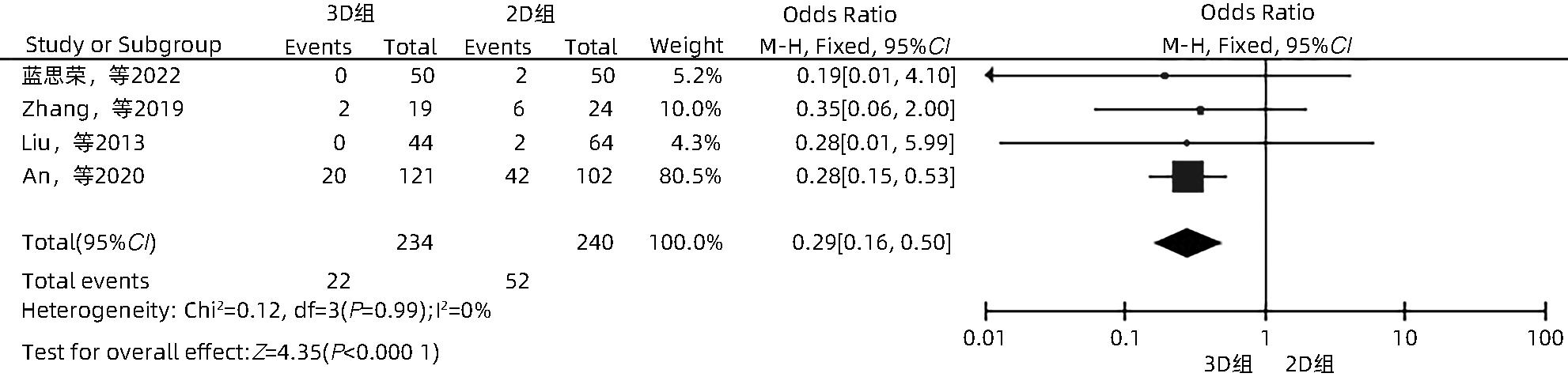
LAN SR, XU JW, ZHANG YM, et al. Guidance of real-time contrast-enhanced ultrasonography and 3D ultrasound fusion imaging for ablation area in patients with primary liver cancer during microwave ablation therapy[J]. J Pract Hepatol, 2022, 25( 6): 889- 892. DOI: 10.3969/j.issn.1672-5069.2022.06.033. |
| [17] |
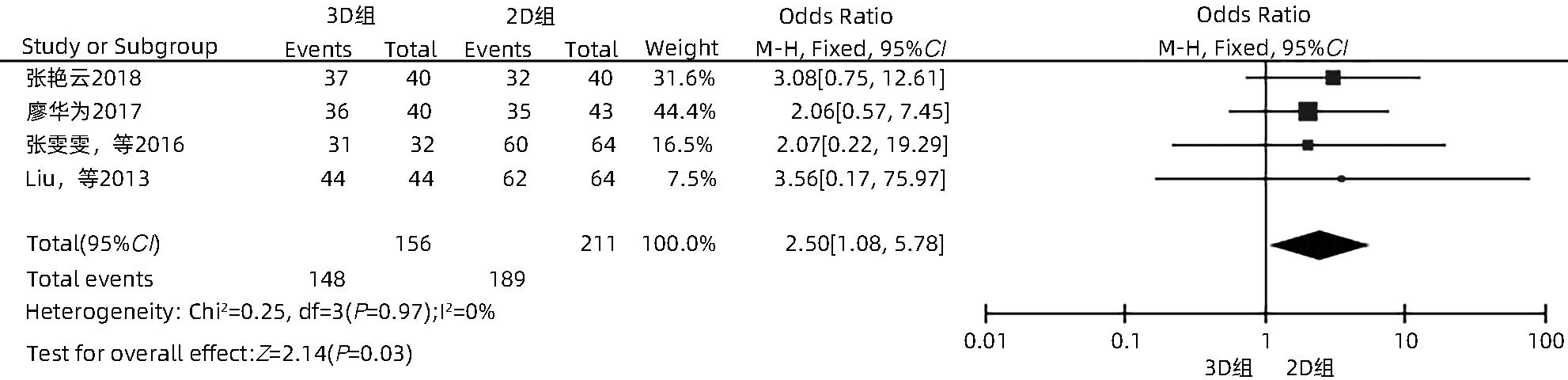
ZHANG YY. To explore the clinical effect of microwave ablation guided by ultrasound combined with three-dimensional imaging technology in the treatment of large liver cancer[J]. Cap Food Med, 2018, 25( 17): 69. DOI: 10.3969/j.issn.1005-8257.2018.17.052. |
| [18] |
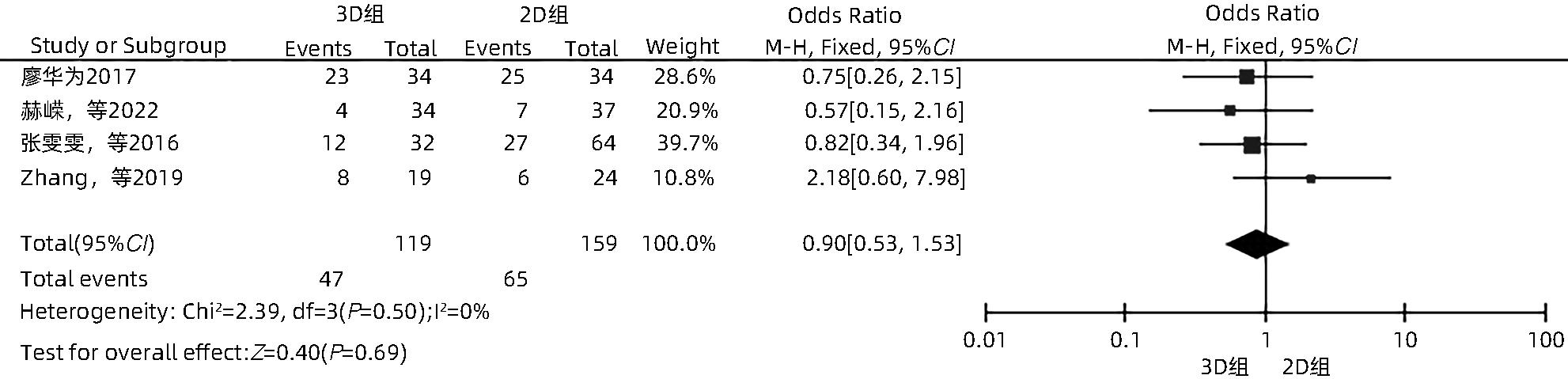
LIAO HW. Study on three-dimensional visualization technology in microwave ablation of liver cancer[J]. World Latest Med Inf, 2017, 17( 61): 46. DOI: 10.19613/j.cnki.1671-3141.2017.61.033. |
| [19] |
HE R, JIA Z, JIANG L, et al. Application of the three-dimensional visualization ablation planning system in radiofrequency ablation for hepatocellular carcinoma[J]. J Clin Hepatol, 2022, 38( 9): 2046- 2052. DOI: 10.3969/j.issn.1001-5256.2022.09.019. |
| [20] |
HAN Y, LIU CB, LI J. Ultrasound-guided percutaneous microwave ablation assisted by three-dimensional visualization operative planning for liver cancer abutting diaphragmatic dome[J]. Chin J Gastroenterol Hepatol, 2021, 30( 11): 1256- 1261. DOI: 10.3969/j.issn.1006-5709.2021.11.011. |
| [21] |
ZHANG WW, WANG HG, SHI XJ, et al. Significance of three-dimensional reconstruction as a method of preoperative planning of laparoscopic radiofrequency ablation[J]. Chin J Surg, 2016, 54( 9): 692- 699. DOI: 10.3760/cma.j.issn.0529-5815.2016.09.009. |
| [22] |
WANG XD, ZHAO P. Comparison between two-dimensional and three-dimensional contrast-enhanced ultrasound radiofrequency ablation in application of hepatocellular carcinoma[J]. J Sun Yat Sen Univ Med Sci, 2014, 35( 4): 602- 606.
王晓东, 赵萍. 二维与三维超声造影在原发性肝癌射频治疗中的应用比较[J]. 中山大学学报(医学科学版), 2014, 35( 4): 602- 606.
|
| [23] |
LIU FY, LIANG P, YU XL, et al. A three-dimensional visualisation preoperative treatment planning system in microwave ablation for liver cancer: A preliminary clinical application[J]. Int J Hyperthermia, 2013, 29( 7): 671- 677. DOI: 10.3109/02656736.2013.834383. |
| [24] |
AN C, LI X, ZHANG M, et al. 3D visualization ablation planning system assisted microwave ablation for hepatocellular carcinoma(Diameter>3): A precise clinical application[J]. BMC Cancer, 2020, 20( 1): 44. DOI: 10.1186/s12885-020-6519-y. |
| [25] |
LIANG P, WANG Y. Microwave ablation of hepatocellular carcinoma[J]. Oncology, 2007, 72( Suppl 1): 124- 131. DOI: 10.1159/000111718. |
| [26] |
FENSTER A, SURRY K, SMITH W, et al. 3D ultrasound imaging: Applications in image-guided therapy and biopsy[J]. Comput Graph, 2002, 26( 4): 557- 568. DOI: 10.1016/s0097-8493(02)00101-2. |
| [27] |
YUAN YC, YUAN XC, WANG Q, et al. Ultrasound-guided percutaneous microwave ablation assisted by three-dimensional planning system combined with transhepatic arterial chemoembolization for treating single large hepatocellular carcinoma: A primary study of survival[J/CD]. Chin J Med Ultrasound(Electronic Edition), 2020, 17( 4): 315- 319. DOI: 10.3877/cma.j.issn.1672-6448.2020.04.005. |
| [28] |
ROBERTS DW, STROHBEHN JW, HATCH JF, et al. A frameless stereotaxic integration of computerized tomographic imaging and the operating microscope[J]. J Neurosurg, 1986, 65( 4): 545- 549. DOI: 10.3171/jns.1986.65.4.0545. |
| [29] |
JIANG JH, PEI L, JIANG RY. Clinical efficacy and safety of 3D vascular reconstruction combined with 3D navigation in laparoscopic hepatectomy: Systematic review and meta-analysis[J]. J Gastrointest Oncol, 2022, 13( 3): 1215- 1223. DOI: 10.21037/jgo-22-198. |
| [30] |
ZHAO QX, YU J, DONG LN, et al. Analysis of recurrent hepatocellular carcinoma treated by microwave ablation assisted by three-dimensional visualization[J]. Chin J Pract Surg, 2019, 39( 10): 1068- 1070, 1076. DOI: 10.19538/j.cjps.issn1005-2208.2019.10.18. |
| [31] |
BALE R, SCHULLIAN P, EBERLE G, et al. Stereotactic radiofrequency ablation of hepatocellular carcinoma: A histopathological study in explanted livers[J]. Hepatology, 2019, 70( 3): 840- 850. DOI: 10.1002/hep.30406. |
| [32] |
LAIMER G, SCHULLIAN P, JASCHKE N, et al. Minimal ablative margin(MAM) assessment with image fusion: An independent predictor for local tumor progression in hepatocellular carcinoma after stereotactic radiofrequency ablation[J]. Eur Radiol, 2020, 30( 5): 2463- 2472. DOI: 10.1007/s00330-019-06609-7. |
| [33] |
HOCQUELET A, TRILLAUD H, FRULIO N, et al. Three-dimensional measurement of hepatocellular carcinoma ablation zones and margins for predicting local tumor progression[J]. J Vasc Interv Radiol, 2016, 27( 7): 1038- 1045. DOI: 10.1016/j.jvir.2016.02.031. |
| [34] |
PERRODIN S, LACHENMAYER A, MAURER M, et al. Percutaneous stereotactic image-guided microwave ablation for malignant liver lesions[J]. Sci Rep, 2019, 9( 1): 13836. DOI: 10.1038/s41598-019-50159-3. |
| [35] |
LIANG P, DONG BW, YU XL, et al. Prognostic factors for survival in patients with hepatocellular carcinoma after percutaneous microwave ablation[J]. Radiology, 2005, 235( 1): 299- 307. DOI: 10.1148/radiol.2351031944. |







 DownLoad:
DownLoad: