| [1] |
QIU ZX, HUANG LX, WANG XX, et al. Exploring the pathogenesis of autoimmune liver diseases from the heterogeneity of target cells[J]. J Clin Transl Hepatol, 2024, 12( 7): 659- 666. DOI: 10.14218/JCTH.2023.00531. |
| [2] |
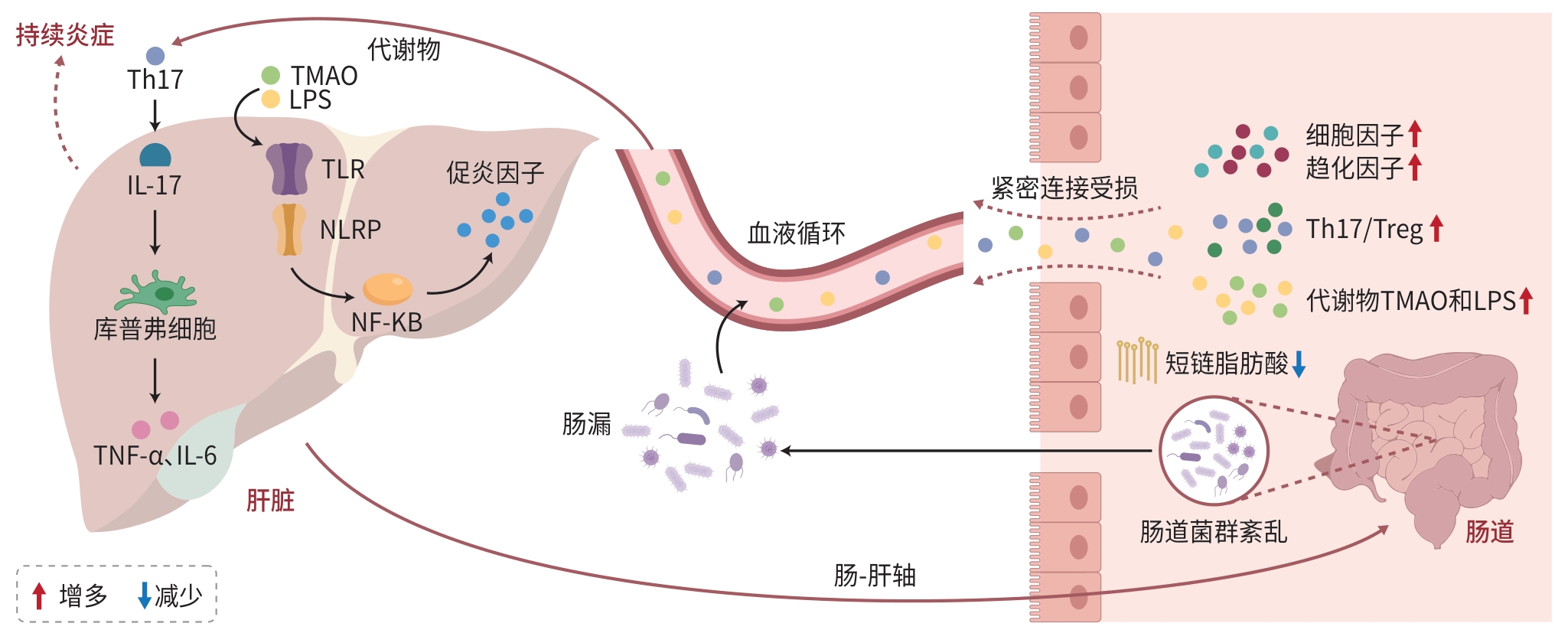
ZHAO YJ, XIE L, ZHANG YT, et al. Pyroptosis: A new bridge connecting gut microbiota and liver diseases[J]. J Clin Hepatol, 2024, 40( 9): 1908- 1915. DOI: 10.12449/JCH240930. 赵奕杰, 谢露, 张亚亭, 等. 细胞焦亡: 连接肠道菌群与肝脏疾病的新桥梁[J]. 临床肝胆病杂志, 2024, 40( 9): 1908- 1915. DOI: 10.12449/JCH240930. |
| [3] |
LI R, MAO ZS, YE XJ, et al. Human gut microbiome and liver diseases: From correlation to causation[J]. Microorganisms, 2021, 9( 5): 1017. DOI: 10.3390/microorganisms9051017. |
| [4] |
CHENG ZL, YANG L, CHU HK. The gut microbiota: A novel player in autoimmune hepatitis[J]. Front Cell Infect Microbiol, 2022, 12: 947382. DOI: 10.3389/fcimb.2022.947382. |
| [5] |
BERINGER A, MIOSSEC P. IL-17 and IL-17-producing cells and liver diseases, with focus on autoimmune liver diseases[J]. Autoimmun Rev, 2018, 17( 12): 1176- 1185. DOI: 10.1016/j.autrev.2018.06.008. |
| [6] |
YANG Y, CHOI J, CHEN Y, et al. E. coli and the etiology of human PBC: Antimitochondrial antibodies and spreading determinants[J]. Hepatology, 2022, 75( 2): 266- 279. DOI: 10.1002/hep.32172. |
| [7] |
TERJUNG B, SPENGLER U. Atypical p-ANCA in PSC and AIH: A Hint Toward a“leaky gut”[J]. Clin Rev Allergy Immunol, 2009, 36( 1): 40- 51. DOI: 10.1007/s12016-008-8088-8. |
| [8] |
GOEL R, EAPEN CE. Recognizing dysfunctional innate and adaptive immune responses contributing to liver damage in patients with cirrhosis[J]. J Clin Exp Hepatol, 2022, 12( 3): 993- 1002. DOI: 10.1016/j.jceh.2021.10.001. |
| [9] |
LIU H, ZHAO J, ZHANG WJ, et al. Impacts of sodium butyrate on intestinal mucosal barrier and intestinal microbial community in a weaned piglet model[J]. Front Microbiol, 2022, 13: 1041885. DOI: 10.3389/fmicb.2022.1041885. |
| [10] |
KAYAMA H, OKUMURA R, TAKEDA K. Interaction between the microbiota, epithelia, and immune cells in the intestine[J]. Annu Rev Immunol, 2020, 38: 23- 48. DOI: 10.1146/annurev-immunol-070119-115104. |
| [11] |
INAMINE T, SCHNABL B. Immunoglobulin A and liver diseases[J]. J Gastroenterol, 2018, 53( 6): 691- 700. DOI: 10.1007/s00535-017-1400-8. |
| [12] |
LAPIDOT Y, AMIR A, BEN-SIMON S, et al. Alterations of the salivary and fecal microbiome in patients with primary sclerosing cholangitis[J]. Hepatol Int, 2021, 15( 1): 191- 201. DOI: 10.1007/s12072-020-10089-z. |
| [13] |
ÖZDIRIK B, SCHERF M, BRUMERCEK A, et al. Biliary microbial patterns in primary sclerosing cholangitis are linked to poorer transplant-free survival[J]. Hepatol Commun, 2023, 7( 6): e0156. DOI: 10.1097/HC9.000-0000000000156. |
| [14] |
BABU G, MOHANTY B. Neurotensin modulation of lipopolysaccharide induced inflammation of gut-liver axis: Evaluation using neurotensin receptor agonist and antagonist[J]. Neuropeptides, 2023, 97: 102297. DOI: 10.1016/j.npep.2022.102297. |
| [15] |
VERMA S, REDDY P, SOWDHAMINI R. Integrated approaches for the recognition of small molecule inhibitors for Toll-like receptor 4[J]. Comput Struct Biotechnol J, 2023, 21: 3680- 3689. DOI: 10.1016/j.csbj.2023.07.026. |
| [16] |
KIM YS, HURLEY EH, PARK Y, et al. Primary sclerosing cholangitis(PSC) and inflammatory bowel disease(IBD): A condition exemplifying the crosstalk of the gut-liver axis[J]. Exp Mol Med, 2023, 55( 7): 1380- 1387. DOI: 10.1038/s12276-023-01042-9. |
| [17] |
KUMMEN M, THINGHOLM LB, RÜHLEMANN MC, et al. Altered gut microbial metabolism of essential nutrients in primary sclerosing cholangitis[J]. Gastroenterology, 2021, 160( 5): 1784- 1798. e 0. DOI: 10.1053/j.gastro.2020.12.058. |
| [18] |
KOTLYAROV S. Importance of the gut microbiota in the gut-liver axis in normal and liver disease[J]. World J Hepatol, 2024, 16( 6): 878- 882. DOI: 10.4254/wjh.v16.i6.878. |
| [19] |
BIAGIOLI M, CARINO A, FIORUCCI C, et al. GPBAR1 functions as gatekeeper for liver NKT cells and provides counterregulatory signals in mouse models of immune-mediated hepatitis[J]. Cell Mol Gastroenterol Hepatol, 2019, 8( 3): 447- 473. DOI: 10.1016/j.jcmgh.2019.06.003. |
| [20] |
PAIK D, YAO LN, ZHANG YC, et al. Human gut bacteria produce Τ Η17-modulating bile acid metabolites[J]. Nature, 2022, 603( 7903): 907- 912. DOI: 10.1038/s41586-022-04480-z. |
| [21] |
ZHANG L, YANG L, CHU HK. Targeting gut microbiota for the treatment of primary biliary cholangitis: From bench to bedside[J]. J Clin Transl Hepatol, 2023, 11( 4): 958- 966. DOI: 10.14218/JCTH.2022.00408. |
| [22] |
LIWINSKI T, ZENOUZI R, JOHN C, et al. Alterations of the bile microbiome in primary sclerosing cholangitis[J]. Gut, 2020, 69( 4): 665- 672. DOI: 10.1136/gutjnl-2019-318416. |
| [23] |
JIANG BR, YUAN GH, WU JL, et al. Prevotella copri ameliorates cholestasis and liver fibrosis in primary sclerosing cholangitis by enhancing the FXR signalling pathway[J]. Biochim Biophys Acta Mol Basis Dis, 2022, 1868( 3): 166320. DOI: 10.1016/j.bbadis.2021.166320. |
| [24] |
RAHIMPOUR S, NASIRI-TOOSI M, KHALILI H, et al. A triple blinded, randomized, placebo-controlled clinical trial to evaluate the efficacy and safety of oral vancomycin in primary sclerosing cholangitis: A pilot study[J]. J Gastrointestin Liver Dis, 2016, 25( 4): 457- 464. DOI: 10.15403/jgld.2014.1121.254.rah. |
| [25] |
BRITTO SL, HOFFMAN KL, TESSIER ME, et al. Microbiome responses to vancomycin treatment in a child with primary sclerosing cholangitis and ulcerative colitis[J]. ACG Case Rep J, 2021, 8( 5): e00577. DOI: 10.14309/crj.0000000000000577. |
| [26] |
FÄRKKILÄ M, KARVONEN AL, NURMI H, et al. Metronidazole and ursodeoxycholic acid for primary sclerosing cholangitis: A randomized placebo-controlled trial[J]. Hepatology, 2004, 40( 6): 1379- 1386. DOI: 10.1002/hep.20457. |
| [27] |
di GIORGIO A, TULONE A, NICASTRO E, et al. Use of oral vancomycin in children with autoimmune liver disease: A single centre experience[J]. World J Hepatol, 2021, 13( 12): 2113- 2127. DOI: 10.4254/wjh.v13.i12.2113. |
| [28] |
LI LP, KANG YB. The gut microbiome and autoimmune hepatitis: Implications for early diagnostic biomarkers and novel therapies[J]. Mol Nutr Food Res, 2023, 67( 24): e2300043. DOI: 10.1002/mnfr.20-2300043. |
| [29] |
PHILIPS CA, AUGUSTINE P, PHADKE N. Healthy donor fecal microbiota transplantation for recurrent bacterial cholangitis in primary sclerosing cholangitis- a single case report[J]. J Clin Transl Hepatol, 2018, 6( 4): 438- 441. DOI: 10.14218/JCTH.2018.00033. |
| [30] |
ALLEGRETTI JR, KASSAM Z, CARRELLAS M, et al. Fecal microbiota transplantation in patients with primary sclerosing cholangitis: A pilot clinical trial[J]. Am J Gastroenterol, 2019, 114( 7): 1071- 1079. DOI: 10.14309/ajg.0000000000000115. |
| [31] |
JIA W, LI YT, CHEUNG KCP, et al. Bile acid signaling in the regulation of whole body metabolic and immunological homeostasis[J]. Sci China Life Sci, 2024, 67( 5): 865- 878. DOI: 10.1007/s11427-023-2353-0. |
| [32] |
ZHANG HX, LIU M, LIU X, et al. Bifidobacterium animalis ssp. lactis 420 mitigates autoimmune hepatitis through regulating intestinal barrier and liver immune cells[J]. Front Immunol, 2020, 11: 569104. DOI: 10.3389/fimmu.2020.569104. |
| [33] |
MA L, ZHANG LW, ZHUANG Y, et al. Lactobacillus improves the effects of prednisone on autoimmune hepatitis via gut microbiota-mediated follicular helper T cells[J]. Cell Commun Signal, 2022, 20( 1): 83. DOI: 10.1186/s12964-021-00819-7. |
| [34] |
KANG YB, KUANG XY, YAN H, et al. A novel synbiotic alleviates autoimmune hepatitis by modulating the gut microbiota-liver axis and inhibiting the hepatic TLR4/NF-κB/NLRP3 signaling pathway[J]. mSystems, 2023, 8( 2). DOI: 10.1128/msystems.01127-22. |
| [35] |
RODRÍGUEZ-PASTÉN A, PÉREZ-HERNÁNDEZ N, AÑORVE-MORGA J, et al. The activity of prebiotics and probiotics in hepatogastrointestinal disorders and diseases associated with metabolic syndrome[J]. Int J Mol Sci, 2022, 23( 13): 7229. DOI: 10.3390/ijms23137229. |
| [36] |
BOGATIC D, BRYANT RV, LYNCH KD, et al. Systematic review: Microbial manipulation as therapy for primary sclerosing cholangitis[J]. Aliment Pharmacol Ther, 2023, 57( 1): 23- 36. DOI: 10.1111/apt.17251. |
| [37] |
LI C, NIU ZH, ZOU MJ, et al. Probiotics, prebiotics, and synbiotics regulate the intestinal microbiota differentially and restore the relative abundance of specific gut microorganisms[J]. J Dairy Sci, 2020, 103( 7): 5816- 5829. DOI: 10.3168/jds.2019-18003. |
| [38] |
HUANG GF, YANG JH. Relationship between autoantibodies and biochemical responses to different doses of ursodeoxycholic acid for the treatment of primary biliary cholangitis[J]. Med J Chin People’s Liberat Army, 2022, 47( 2): 143- 149. DOI: 10.11855/j.issn.0577-7402.2022.02.0143. |
| [39] |
Chinese Society of Hepatology, Chinese Medical Association. Guideline on the management of cholestasis liver diseases(2021)[J]. J Clin Hepatol, 2022, 38( 1): 62- 69. DOI: 10.3969/j.issn.1001-5256.2022.01.010. |
| [40] |
WU JW, LYU SX, GUO D, et al. Protective effects of YCHD on the autoimmune hepatitis mice model induced by Ad-CYP2D6 through modulating the Th1/Treg ratio and intestinal flora[J]. Front Immunol, 2024, 15: 1488125. DOI: 10.3389/fimmu.2024.1488125. |
| [41] |
ZHOU XH, GONG DY, ZHONG S. Protective effect of modified Yinchenhao decoction against acute liver injury in rats by inhibiting TLR4 signaling pathway[J]. J Shanxi Med Univ, 2021, 52( 9): 1143- 1148. DOI: 10.13753/j.issn.1007-6611.2021.09.009. |
| [42] |
YANG H, LIU QQ, LIU HX, et al. Berberine alleviates concanavalin A-induced autoimmune hepatitis in mice by modulating the gut microbiota[J]. Hepatol Commun, 2024, 8( 4): e0381. DOI: 10.1097/HC9.0000000000000381. |
| [43] |
ZENG X, LIU MH, XIONG Y, et al. Pien Tze Huang alleviates Concanavalin A-induced autoimmune hepatitis by regulating intestinal microbiota and memory regulatory T cells[J]. World J Gastroenterol, 2023, 29( 45): 5988- 6016. DOI: 10.3748/wjg.v29.i45.5988. |
| [44] |
Expert Committee on Hepatology, Doctor Society of Integrative Medicine, Chinese Medical Doctor Association. Experts consensus on integrated traditional Chinese and Western medicine diagnosis and treatment of primary biliary cholangitis[J]. J Clin Hepatol, 2024, 40( 9): 1757- 1766. DOI: 10.12449/JCH240907. 中国医师协会中西医结合医师分会肝病学专家委员会. 原发性胆汁性胆管炎中西医结合诊疗专家共识[J]. 临床肝胆病杂志, 2024, 40( 9): 1757- 1766. DOI: 10.12449/JCH240907. |
| [45] |
GÓRSKI A, JOŃCZYK-MATYSIAK E, ŁUSIAK-SZELACHOWSKA M, et al. Therapeutic potential of phages in autoimmune liver diseases[J]. Clin Exp Immunol, 2018, 192( 1): 1- 6. DOI: 10.1111/cei.13092. |
| [46] |
NIE QX, LUO X, WANG K, et al. Gut symbionts alleviate MASH through a secondary bile acid biosynthetic pathway[J]. Cell, 2024, 187( 11): 2717- 2734. e 33. DOI: 10.1016/j.cell.2024.03.034. |
| [47] |
FUJIKI J, SCHNABL B. Phage therapy: Targeting intestinal bacterial microbiota for the treatment of liver diseases[J]. JHEP Rep, 2023, 5( 12): 100909. DOI: 10.1016/j.jhepr.2023.100909. |
| [48] |
WU ZH, SUN Y, HUANG WB, et al. Direct and indirect effects of estrogens, androgens and intestinal microbiota on colorectal cancer[J]. Front Cell Infect Microbiol, 2024, 14: 1458033. DOI: 10.3389/fcimb.2024.1458033. |
| [49] |
ZHANG HX, LIU M, LIU X, et al. Bifidobacterium animalis ssp. lactis 420 mitigates autoimmune hepatitis through regulating intestinal barrier and liver immune cells[J]. Front Immunol, 2020, 11: 569104. DOI: 10.3389/fimmu.2020.569104. |
| [50] |
ZU Y, YANG JY, ZHANG CL, et al. The pathological mechanisms of estrogen-induced cholestasis: Current perspectives[J]. Front Pharmacol, 2021, 12: 761255. DOI: 10.3389/fphar.2021.761255. |






 DownLoad:
DownLoad: