| [1] |
ISRAELSEN M, FRANCQUE S, TSOCHATZIS EA, et al. Steatotic liver disease[J]. Lancet, 2024, 404( 10464): 1761- 1778. DOI: 10.1016/S0140-6736(24)01811-7. |
| [2] |
HAGSTRÖM H, SHANG Y, HEGMAR H, et al. Natural history and progression of metabolic dysfunction-associated steatotic liver disease[J]. Lancet Gastroenterol Hepatol, 2024, 9( 10): 944- 956. DOI: 10.1016/S2468-1253(24)00193-6. |
| [3] |
DO A, ZAHRAWI F, MEHAL WZ. Therapeutic landscape of metabolic dysfunction-associated steatohepatitis(MASH)[J]. Nat Rev Drug Discov, 2025, 24( 3): 171- 189. DOI: 10.1038/s41573-024-01084-2. |
| [4] |
PARK MD, SILVIN A, GINHOUX F, et al. Macrophages in health and disease[J]. Cell, 2022, 185( 23): 4259- 4279. DOI: 10.1016/j.cell.2022.10.007. |
| [5] |
TARU V, SZABO G, MEHAL W, et al. Inflammasomes in chronic liver disease: Hepatic injury, fibrosis progression and systemic inflammation[J]. J Hepatol, 2024, 81( 5): 895- 910. DOI: 10.1016/j.jhep.2024.06.016. |
| [6] |
FABRE T, BARRON AMS, CHRISTENSEN SM, et al. Identification of a broadly fibrogenic macrophage subset induced by type 3 inflammation[J]. Sci Immunol, 2023, 8( 82): eadd8945. DOI: 10.1126/sciimmunol.add8945. |
| [7] |
CUI XY, SUN QH, ZHENG LH, et al. Role of triggering receptor expressed on myeloid cells 2 in acute and chronic liver diseases[J]. J Clin Hepatol, 2025, 41( 2): 383- 388. DOI: 10.12449/JCH250228. 崔馨月, 孙全昊, 郑丽红, 等. 髓系细胞触发受体2(TREM2)在急慢性肝病中的作用[J]. 临床肝胆病杂志, 2025, 41( 2): 383- 388. DOI: 10.12449/JCH250228. |
| [8] |
XIONG XL, KUANG H, ANSARI S, et al. Landscape of intercellular crosstalk in healthy and NASH liver revealed by single-cell secretome gene analysis[J]. Mol Cell, 2019, 75( 3): 644- 660.e5. DOI: 10.1016/j.molcel.2019.07.028. |
| [9] |
RAMACHANDRAN P, DOBIE R, WILSON-KANAMORI JR, et al. Resolving the fibrotic niche of human liver cirrhosis at single-cell level[J]. Nature, 2019, 575( 7783): 512- 518. DOI: 10.1038/s41586-019-1631-3. |
| [10] |
XIN X, CAI BY, CHEN C, et al. Effect of fuzheng Huayu capsule on experimental non-alcoholic fatty liver fibrosis in mice[J]. Chin J Exp Tradit Med Formulae, 2021, 27( 6): 37- 45. DOI: 10.13422/j.cnki.syfjx.20210202. |
| [11] |
BAILEY JD, SHAW A, MCNEILL E, et al. Isolation and culture of murine bone marrow-derived macrophages for nitric oxide and redox biology[J]. Nitric Oxide, 2020, 100: 17- 29. DOI: 10.1016/j.niox.2020.04.005. |
| [12] |
WATANABE Y, TSUCHIYA A, SEINO S, et al. Mesenchymal stem cells and induced bone marrow-derived macrophages synergistically improve liver fibrosis in mice[J]. STEM CELLS Transl Med, 2019, 8( 3): 271- 284. DOI: 10.1002/sctm.18-0105. |
| [13] |
ISHIYAMA S, HAYATSU M, TORIUMI T, et al. Assessing the combined impact of fatty liver-induced TGF-β1 and LPS-activated macrophages in fibrosis through a novel 3D serial section methodology[J]. Sci Rep, 2024, 14: 11404. DOI: 10.1038/s41598-024-60845-6. |
| [14] |
GUAN X, LIU W, CHEN JM, et al. Research advances in the clinical and basic research on Fuzheng Huayu prescription in treatment of chronic liver diseases[J]. J Clin Hepatol, 2021, 37( 6): 1449- 1453. DOI: 10.3969/j.issn.1001-5256.2021.06.048. |
| [15] |
RAO GC, PENG X, LI XQ, et al. Unmasking the Enigma of lipid metabolism in metabolic dysfunction-associated steatotic liver disease: From mechanism to the clinic[J]. Front Med, 2023, 10: 1294267. DOI: 10.3389/fmed.2023.1294267. |
| [16] |
DENK H, ABUJA PM, ZATLOUKAL K. Animal models of NAFLD from the pathologist’s point of view[J]. Biochim Biophys Acta BBA Mol Basis Dis, 2019, 1865( 5): 929- 942. DOI: 10.1016/j.bbadis.2018.04.024. |
| [17] |
TSUCHIDA T, LEE YA, FUJIWARA N, et al. A simple diet- and chemical-induced murine NASH model with rapid progression of steatohepatitis, fibrosis and liver cancer[J]. J Hepatol, 2018, 69( 2): 385- 395. DOI: 10.1016/j.jhep.2018.03.011. |
| [18] |
TSOUKA S, KUMAR P, SEUBNOOCH P, et al. Transcriptomics-driven metabolic pathway analysis reveals similar alterations in lipid metabolism in mouse MASH model and human[J]. Commun Med, 2024, 4: 39. DOI: 10.1038/s43856-024-00465-3. |
| [19] |
CHENG D, CHAI J, WANG HW, et al. Hepatic macrophages: Key players in the development and progression of liver fibrosis[J]. Liver Int, 2021, 41( 10): 2279- 2294. DOI: 10.1111/liv.14940. |
| [20] |
REMMERIE A, MARTENS L, THONÉ T, et al. Osteopontin expression identifies a subset of recruited macrophages distinct from kupffer cells in the fatty liver[J]. Immunity, 2020, 53( 3): 641- 657. e 14. DOI: 10.1016/j.immuni.2020.08.004. |
| [21] |
GUILLIAMS M, BONNARDEL J, HAEST B, et al. Spatial proteogenomics reveals distinct and evolutionarily conserved hepatic macrophage niches[J]. Cell, 2022, 185( 2): 379- 396. e 38. DOI: 10.1016/j.cell.2021.12.018. |
| [22] |
LINK F, LI YJ, ZHAO JL, et al. ECM1 attenuates hepatic fibrosis by interfering with mediators of latent TGF-1 activation[J]. Gut, 2025, 74( 3): 424- 439. DOI: 10.1136/gutjnl-2024-333213. |
| [23] |
LIU ZY, XIANG HY, XIANG DJ, et al. Revealing potential anti-fibrotic mechanism of Ganxianfang formula based on RNA sequence[J]. Chin Med, 2022, 17( 1): 23. DOI: 10.1186/s13020-022-00579-7. |
| [24] |
GADIPUDI LL, RAMAVATH NN, PROVERA A, et al. Annexin A1 treatment prevents the evolution to fibrosis of experimental nonalcoholic steatohepatitis[J]. Clin Sci, 2022, 136( 9): 643- 656. DOI: 10.1042/cs20211122. |
| [25] |
SEIDMAN JS, TROUTMAN TD, SAKAI M, et al. Niche-specific reprogramming of epigenetic landscapes drives myeloid cell diversity in nonalcoholic steatohepatitis[J]. Immunity, 2020, 52( 6): 1057- 1074.e7. DOI: 10.1016/j.immuni.2020.04.001. |
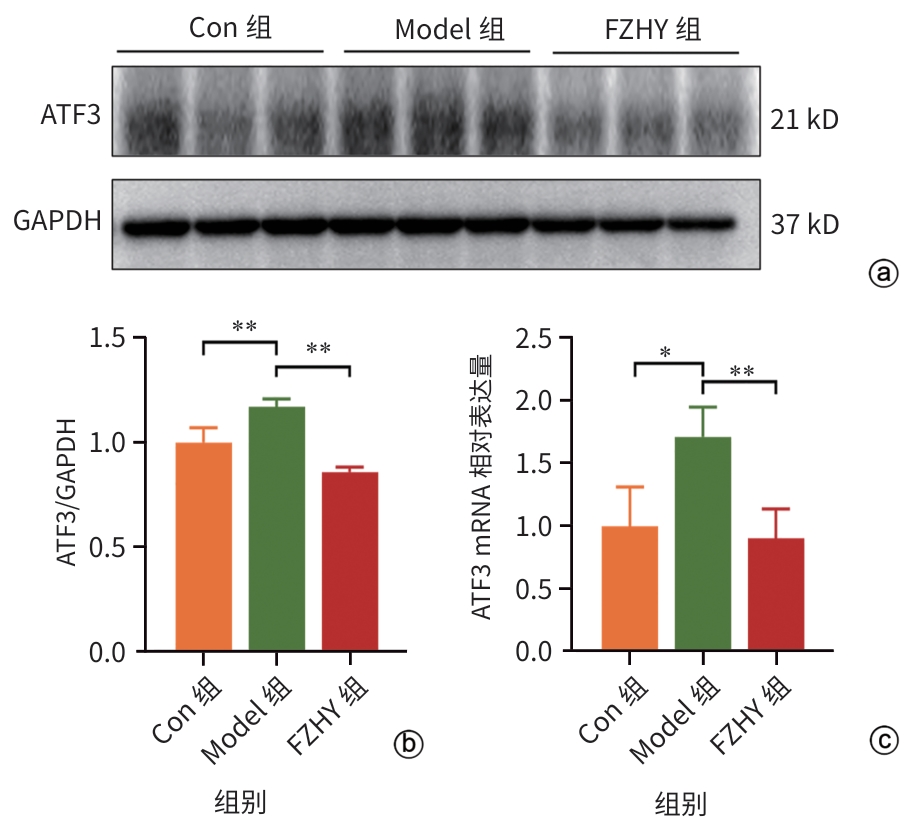
| [26] |
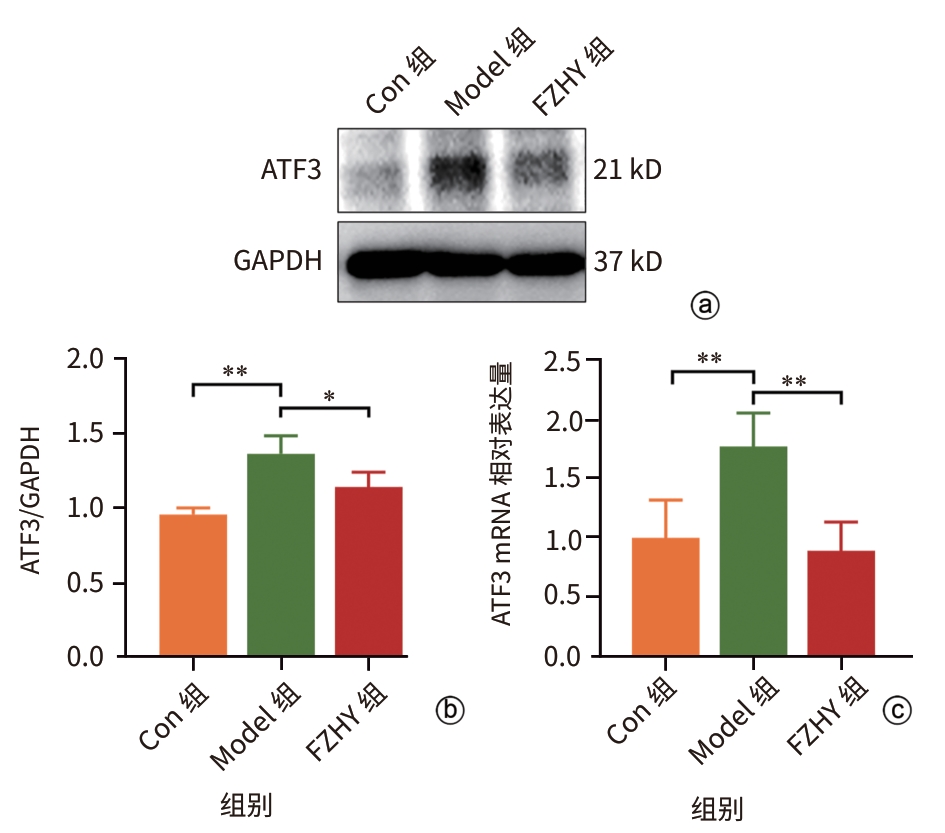
SHI ZM, ZHANG K, CHEN T, et al. Transcriptional factor ATF3 promotes liver fibrosis via activating hepatic stellate cells[J]. Cell Death Dis, 2020, 11: 1066. DOI: 10.1038/s41419-020-03271-6. |
| [27] |
LI XM, LIN LF, LI YF, et al. ATF3-mediated transactivation of CXCL14 in HSCs during liver fibrosis[J]. Clin Transl Med, 2024, 14( 10): e70040. DOI: 10.1002/ctm2.70040. |







 DownLoad:
DownLoad: