| [1] |
ESLAM M, SANYAL AJ, GEORGE J, et al. MAFLD:A consensus-driven proposed nomenclature for metabolic associated fatty liver disease[J]. Gastroenterology, 2020, 158( 7): 1999- 2014.e1. DOI: 10.1053/j.gastro.2019.11.312. |
| [2] |
ESLAM M, FAN JG, YU ML, et al. The Asian Pacific association for the study of the liver clinical practice guidelines for the diagnosis and management of metabolic dysfunction-associated fatty liver disease[J]. Hepatol Int, 2025, 19( 2): 261- 301. DOI: 10.1007/s12072-024-10774-3. |
| [3] |
RINELLA ME, LAZARUS JV, RATZIU V, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature[J]. Ann Hepatol, 2024, 29( 1): 101133. DOI: 10.1016/j.aohep.2023.101133. |
| [4] |
Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of metabolic dysfunction-associated(non- alcoholic)fatty liver disease(Version 2024)[J]. J Prac Hepatol, 2024, 27( 4): 494- 510. DOI: 10.3760/cma.j.cn501113-20240327-00163. |
| [5] |
ISRAELSEN M, FRANCQUE S, TSOCHATZIS EA, et al. Steatotic liver disease[J]. Lancet, 2024, 404( 10464): 1761- 1778. DOI: 10.1016/S0140-6736(24)01811-7. |
| [6] |
WU XN, XUE F, ZHANG N, et al. Global burden of liver cirrhosis and other chronic liver diseases caused by specific etiologies from 1990 to 2019[J]. BMC Public Health, 2024, 24( 1): 363. DOI: 10.1186/s12889-024-17948-6. |
| [7] |
MIAO L, TARGHER G, BYRNE CD, et al. Current status and future trends of the global burden of MASLD[J]. Trends Endocrinol Metab, 2024, 35( 8): 697- 707. DOI: 10.1016/j.tem.2024.02.007. |
| [8] |
SIMON TG, ROELSTRAETE B, KHALILI H, et al. Mortality in biopsy-confirmed nonalcoholic fatty liver disease: Results from a nationwide cohort[J]. Gut, 2021, 70( 7): 1375- 1382. DOI: 10.1136/gutjnl-2020-322786. |
| [9] |
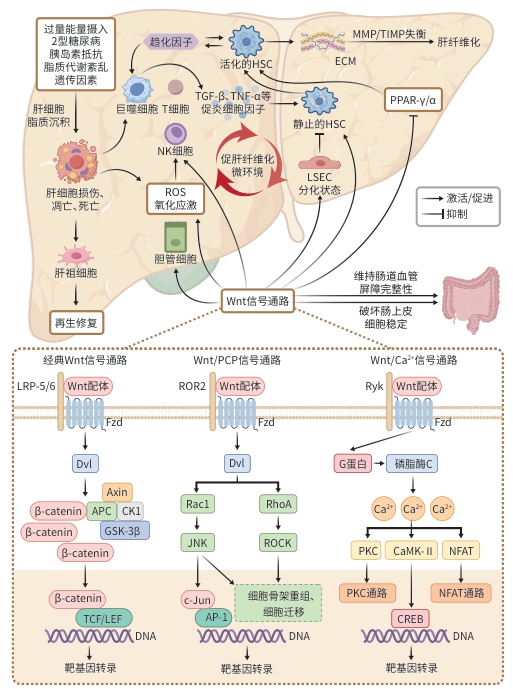
SHREE HARINI K, EZHILARASAN D. Wnt/beta-catenin signaling and its modulators in nonalcoholic fatty liver diseases[J]. Hepatobiliary Pancreat Dis Int, 2023, 22( 4): 333- 345. DOI: 10.1016/j.hbpd.2022.10.003. |
| [10] |
PERUGORRIA MJ, OLAIZOLA P, LABIANO I, et al. Wnt-β-catenin signalling in liver development, health and disease[J]. Nat Rev Gastroenterol Hepatol, 2019, 16( 2): 121- 136. DOI: 10.1038/s41575-018-0075-9. |
| [11] |
|
| [12] |
QIN K, YU M, FAN JM, et al. Canonical and noncanonical Wnt signaling: Multilayered mediators, signaling mechanisms and major signaling crosstalk[J]. Genes Dis, 2023, 11( 1): 103- 134. DOI: 10.1016/j.gendis.2023.01.030. |
| [13] |
ISHITANI T, KISHIDA S, HYODO-MIURA J, et al. The TAK1-NLK mitogen-activated protein kinase cascade functions in the Wnt-5a/Ca(2+) pathway to antagonize Wnt/beta-catenin signaling[J]. Mol Cell Biol, 2003, 23( 1): 131- 139. DOI: 10.1128/MCB.23.1.131-139.2003. |
| [14] |
SCHWABE RF, TABAS I, PAJVANI UB. Mechanisms of fibrosis development in nonalcoholic steatohepatitis[J]. Gastroenterology, 2020, 158( 7): 1913- 1928. DOI: 10.1053/j.gastro.2019.11.311. |
| [15] |
BOUREBABA N, MARYCZ K. Hepatic stellate cells role in the course of metabolic disorders development- A molecular overview[J]. Pharmacol Res, 2021, 170: 105739. DOI: 10.1016/j.phrs.2021.105739. |
| [16] |
LI YQ, TANG WJ, ZHOU YJ. Role of intestinal microbiota and metabolites in the development, progression, and treatment of nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2023, 39( 8): 1805- 1810. DOI: 10.3969/j.issn.1001-5256.2023.08.006. |
| [17] |
DU JH, REN WG, ZHANG QS, et al. Heme oxygenase-1 suppresses Wnt signaling pathway in nonalcoholic steatohepatitis-related liver fibrosis[J]. Biomed Res Int, 2020, 2020: 4910601. DOI: 10.1155/2020/4910601. |
| [18] |
WANG FX, CHEN L, KONG DS, et al. Canonical Wnt signaling promotes HSC glycolysis and liver fibrosis through an LDH-A/HIF-1α transcriptional complex[J]. Hepatology, 2024, 79( 3) 606- 623. DOI: 10.1097/HEP.0000000000000569. |
| [19] |
ESMAIL MM, SAEED NM, MICHEL HE, et al. The ameliorative effect of niclosamide on bile duct ligation induced liver fibrosis via suppression of NOTCH and Wnt pathways[J]. Toxicol Lett, 2021, 347: 23- 35. DOI: 10.1016/j.toxlet.2021.04.018. |
| [20] |
PERKINS RS, SINGH R, ABELL AN, et al. The role of WNT10B in physiology and disease: A 10-year update[J]. Front Cell Dev Biol, 2023, 11: 1120365. DOI: 10.3389/fcell.2023.1120365. |
| [21] |
XI Y, LACANNA R, MA HY, et al. A WISP1 antibody inhibits MRTF signaling to prevent the progression of established liver fibrosis[J]. Cell Metab, 2022, 34( 9): 1377- 1393.e8. DOI: 10.1016/j.cmet.2022.07.009. |
| [22] |
MIAO JH, HUANG JW, LUO CW, et al. Klotho retards renal fibrosis through targeting mitochondrial dysfunction and cellular senescence in renal tubular cells[J]. Physiol Rep, 2021, 9( 2): e14696. DOI: 10.14814/phy2.14696. |
| [23] |
XU DN, ZHUANG SQ, CHEN HZ, et al. IL-33 regulates adipogenesis via Wnt/β-catenin/PPAR-γ signaling pathway in preadipocytes[J]. J Transl Med, 2024, 22( 1): 363. DOI: 10.1186/s12967-024-05180-0. |
| [24] |
TABAA MM EL, FAHEEM H, ELBALLAL MS, et al. The PPAR-α agonist oleoyethanolamide(OEA) ameliorates valproic acid-induced steatohepatitis in rats via suppressing Wnt3a/β-catenin and activating PGC-1α: Involvement of network pharmacology and molecular docking[J]. Eur J Pharmacol, 2025, 991: 177306. DOI: 10.1016/j.ejphar.2025.177306. |
| [25] |
MOTIZUKI M, YOKOYAMA T, SAITOH M, et al. The Snail signaling branch downstream of the TGF-β/Smad3 pathway mediates Rho activation and subsequent stress fiber formation[J]. J Biol Chem, 2024, 300( 1): 105580. DOI: 10.1016/j.jbc.2023.105580. |
| [26] |
LIU ZW, KUNA VK, XU B, et al. Wnt ligands 3a and 5a regulate proliferation and migration in human fetal liver progenitor cells[J]. Transl Gastroenterol Hepatol, 2021, 6: 56. DOI: 10.21037/tgh.2020.01.12. |
| [27] |
KE ZL, HUANG YB, XU J, et al. Escherichia coli NF73-1 disrupts the gut-vascular barrier and aggravates high-fat diet-induced fatty liver disease via inhibiting Wnt/β-catenin signalling pathway[J]. Liver Int, 2024, 44( 3): 776- 790. DOI: 10.1111/liv.15823. |
| [28] |
DONG X, LUO Y, LU S, et al. Ursodesoxycholic acid alleviates liver fibrosis via proregeneration by activation of the ID1-WNT2/HGF signaling pathway[J]. Clin Transl Med, 2021, 11( 2): e296. DOI: 10.1002/ctm2.296. |
| [29] |
CHEN T, SHI ZM, ZHAO YM, et al. LncRNA Airn maintains LSEC differentiation to alleviate liver fibrosis via the KLF2-ENOS-sGC pathway[J]. BMC Med, 2022, 20( 1): 335. DOI: 10.1186/s12916-022-02523-w. |
| [30] |
DUAN JL, RUAN B, YAN XC, et al. Endothelial Notch activation reshapes the angiocrine of sinusoidal endothelia to aggravate liver fibrosis and blunt regeneration in mice[J]. Hepatology, 2018, 68( 2): 677- 690. DOI: 10.1002/hep.29834. |
| [31] |
XU T, PAN LX, LI LY, et al. microRNA-708 modulates Hepatic Stellate Cells activation and enhances extracellular matrix accumulation via direct targeting TMEM88[J]. J Cell Mol Med, 2020, 24( 13): 7127- 7140. DOI: 10.1111/jcmm.15119. |
| [32] |
YUAN Y, HAN QJ, LI SY, et al. Wnt2b attenuates HSCs activation and liver fibrosis through negative regulating TLR4 signaling[J]. Sci Rep, 2017, 7( 1): 3952. DOI: 10.1038/s41598-017-04374-5. |
| [33] |
RIGUAL MDM, ANGULO-AGUADO M, ZAGORAC S, et al. Macrophages harness hepatocyte glutamate to boost liver regeneration[J]. Nature, 2025, 641( 8064): 1005- 1016. DOI: 10.1038/s41586-025-08778-6. |
| [34] |
ZHANG P, LIU JL, LEE A, et al. IL-22 resolves MASLD via enterocyte STAT3 restoration of diet-perturbed intestinal homeostasis[J]. Cell Metab, 2024, 36( 10): 2341- 2354.e6. DOI: 10.1016/j.cmet.2024.08.012. |
| [35] |
CHEN Y, GAO WK, SHU YY, et al. Mechanisms of ductular reaction in non-alcoholic steatohepatitis[J]. World J Gastroenterol, 2022, 28( 19): 2088- 2099. DOI: 10.3748/wjg.v28.i19.2088. |
| [36] |
WEI M, ZHANG CM, TIAN YJ, et al. Expression and function of WNT6: From development to disease[J]. Front Cell Dev Biol, 2020, 8: 558155. DOI: 10.3389/fcell.2020.558155. |
| [37] |
CATALANO T, SELVAGGI F, ESPOSITO DL, et al. Infectious agents induce Wnt/β-catenin pathway deregulation in primary liver cancers[J]. Microorganisms, 2023, 11( 7): 1632. DOI: 10.3390/microorganisms11071632. |
| [38] |
SHREE HARINI K, EZHILARASAN D, MANI U. Molecular insights on intracellular Wnt/β-catenin signaling in alcoholic liver disease[J]. Cell Biochem Funct, 2024, 42( 1): e3916. DOI: 10.1002/cbf.3916. |
| [39] |
LEI ZL, YANG LX, YANG YH, et al. Activation of Wnt/β-catenin pathway causes insulin resistance and increases lipogenesis in HepG2 cells via regulation of endoplasmic reticulum stress[J]. Biochem Biophys Res Commun, 2020, 526( 3): 764- 771. DOI: 10.1016/j.bbrc.2020.03.147. |
| [40] |
ASTARINI F DWI, RATNASARI N, WASITYASTUTI W. Update on non-alcoholic fatty liver disease-associated single nucleotide polymorphisms and their involvement in liver steatosis, inflammation, and fibrosis: A narrative review[J]. Iran Biomed J, 2022, 26( 4): 252- 268. DOI: 10.52547/ibj.3647. |
| [41] |
QIU YY, ZHANG J, ZENG FY, et al. Roles of the peroxisome proliferator-activated receptors(PPARs) in the pathogenesis of nonalcoholic fatty liver disease(NAFLD)[J]. Pharmacol Res, 2023, 192: 106786. DOI: 10.1016/j.phrs.2023.106786. |
| [42] |
TERATANI T, TOMITA K, SUZUKI T, et al. Aortic carboxypeptidase-like protein, a WNT ligand, exacerbates nonalcoholic steatohepatitis[J]. J Clin Invest, 2018, 128( 4): 1581- 1596. DOI: 10.1172/JCI92863. |
| [43] |
LI F, LI MW, WANG YS. Therapeutic paradigms and potential therapies for nonalcoholic steatohepatitis[J]. J Clin Hepatol, 2024, 40( 10): 2082- 2086. DOI: 10.12449/JCH241025. 李凤, 李茂微, 王雨杉. 非酒精性脂肪肝病的治疗模式和潜在疗法[J]. 临床肝胆病杂志, 2024, 40( 10): 2082- 2086. DOI: 10.12449/JCH241025. |
| [44] |
EL-DERANY MO, EL-DEMERDASH E. Pyrvinium pamoate attenuates non-alcoholic steatohepatitis: Insight on hedgehog/Gli and Wnt/β-catenin signaling crosstalk[J]. Biochem Pharmacol, 2020, 177: 113942. DOI: 10.1016/j.bcp.2020.113942. |
| [45] |
ZHANG MJ, HAUGHEY M, WANG NY, et al. Targeting the Wnt signaling pathway through R-spondin 3 identifies an anti-fibrosis treatment strategy for multiple organs[J]. PLoS One, 2020, 15( 3): e0229445. DOI: 10.1371/journal.pone.0229445. |
| [46] |
HE WW, YANG RG, LUO TT. Effect of ginsenoside Rg 1 on liver fibrosis in mice with non-alcoholic fatty liver disease[J]. J Chin Med Mater, 2021, 44( 5): 1208- 1212. DOI: 10.13863/j.issn1001-4454.2021.05.032. |
| [47] |
LI QJ, GONG YQ, WANG Y, et al. Sirt1 promotes the restoration of hepatic progenitor cell(HPC)-mediated liver fatty injury in NAFLD through activating the Wnt/β-catenin signal pathway[J]. Front Nutr, 2021, 8: 791861. DOI: 10.3389/fnut.2021.791861. |
| [48] |
YU J, ZHAO Y, XU LL, et al. Liraglutide attenuates hepatic oxidative stress, inflammation, and apoptosis in streptozotocin-induced diabetic mice by modulating the Wnt/β-catenin signaling pathway[J]. Mediators Inflamm, 2023, 2023: 8974960. DOI: 10.1155/2023/8974960. |
| [49] |
XUE C, CHU QF, SHI QM, et al. Wnt signaling pathways in biology and disease: Mechanisms and therapeutic advances[J]. Signal Transduct Target Ther, 2025, 10( 1): 106. DOI: 10.1038/s41392-025-02142-w. |
| [50] |
ZHENG GG, LIN SQ, WANG SJ, et al. Regulation of natural products on Wnt/β-catenin signaling pathway in diseases[J]. Am J Chin Med, 2025, 53( 3): 709- 735. DOI: 10.1142/S0192415X25500272. |
| [51] |
DUSPARA K, BOJANIC K, PEJIC JI, et al. Targeting the Wnt signaling pathway in liver fibrosis for drug options: An update[J]. J Clin Transl Hepatol, 2021, 9( 6): 960- 971. DOI: 10.14218/JCTH.2021.00065. |






 DownLoad:
DownLoad: