| [1] |
LAMMERT F, GURUSAMY K, KO CW, et al. Gallstones[J]. Nat Rev Dis Primers, 2016, 2: 16024. DOI: 10.1038/nrdp.2016.24. |
| [2] |
COSTA CJ, NGUYEN MTT, VAZIRI H, et al. Genetics of gallstone disease and their clinical significance: A narrative review[J]. J Clin Transl Hepatol, 2024, 12( 3): 316- 326. DOI: 10.14218/JCTH.2023.00563. |
| [3] |
KATSIKA D, GRJIBOVSKI A, EINARSSON C, et al. Genetic and environmental influences on symptomatic gallstone disease: A Swedish study of 43, 141 twin pairs[J]. Hepatology, 2005, 41( 5): 1138- 1143. DOI: 10.1002/hep.20654. |
| [4] |
BUSTOS BI, PÉREZ-PALMA E, BUCH S, et al. Variants in ABCG8 and TRAF3 genes confer risk for gallstone disease in admixed Latinos with Mapuche Native American ancestry[J]. Sci Rep, 2019, 9( 1): 772. DOI: 10.1038/s41598-018-35852-z. |
| [5] |
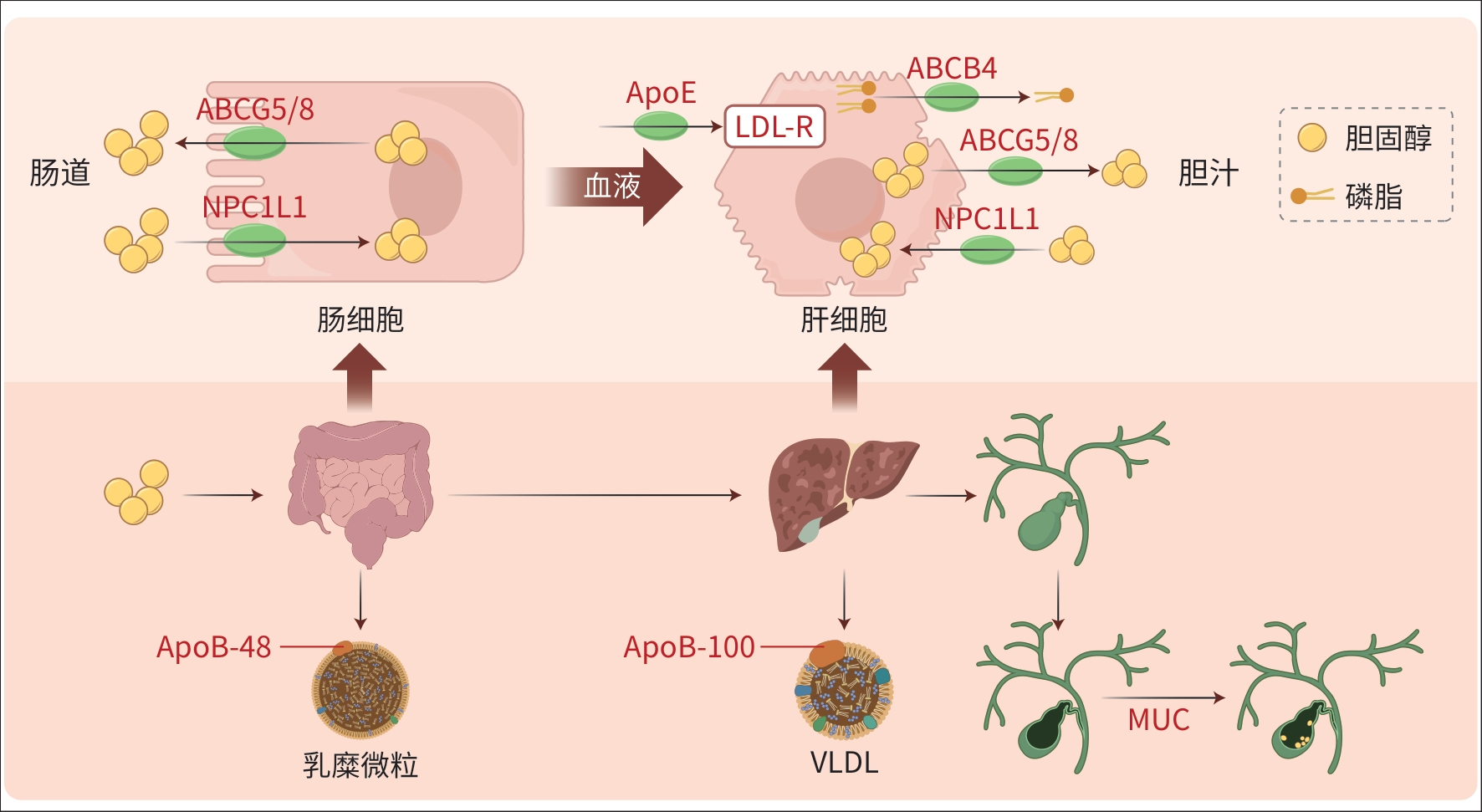
WANG HH, LIU M, PORTINCASA P, et al. Recent advances in the critical role of the sterol efflux transporters ABCG5/G8 in health and disease[J]. Adv Exp Med Biol, 2020, 1276: 105- 136. DOI: 10.1007/978-981-15-6082-8_8. |
| [6] |
SUN H, WARREN J, YIP J, et al. Factors influencing gallstone formation: A review of the literature[J]. Biomolecules, 2022, 12( 4): 550. DOI: 10.3390/biom12040550. |
| [7] |
BYDLOWSKI SP, LEVY D. Association of ABCG5 and ABCG8 transporters with sitosterolemia[J]. Adv Exp Med Biol, 2024, 1440: 31- 42. DOI: 10.1007/978-3-031-43883-7_2. |
| [8] |
SRIVASTAVA A, SRIVASTAVA A, SRIVASTAVA K, et al. Role of ABCG8 D19H(rs11887534) variant in gallstone susceptibility in northern India[J]. J Gastroenterol Hepatol, 2010, 25( 11): 1758- 1762. DOI: 10.1111/j.1440-1746.2010.06349.x. |
| [9] |
GRÜNHAGE F, ACALOVSCHI M, TIRZIU S, et al. Increased gallstone risk in humans conferred by common variant of hepatic ATP-binding cassette transporter for cholesterol[J]. Hepatology, 2007, 46( 3): 793- 801. DOI: 10.1002/hep.21847. |
| [10] |
WEBER SN, BOPP C, KRAWCZYK M, et al. Genetics of gallstone disease revisited: Updated inventory of human lithogenic genes[J]. Curr Opin Gastroenterol, 2019, 35( 2): 82- 87. DOI: 10.1097/MOG.00000000-00000511. |
| [11] |
LIANG KW, HUANG HH, WANG LE, et al. Risk of gallstones based on ABCG8 rs11887534 single nucleotide polymorphism among Taiwanese men and women[J]. BMC Gastroenterol, 2021, 21( 1): 468. DOI: 10.1186/s12876-021-02060-5. |
| [12] |
ALY DM, FTEAH AM, ASSALY NM AL, et al. Correlation of serum biochemical characteristics and ABCG8 genetic variant(rs 11887534) with gall stone compositions and risk of gallstone disease in Egyptian patients[J]. Asian J Surg, 2023, 46( 9): 3560- 3567. DOI: 10.1016/j.asjsur.2023.05.156. |
| [13] |
KIM MH, LEE EJ, KIM SJ, et al. Macrophage inhibitory cytokine-1 aggravates diet-induced gallstone formation via increased ABCG5/ABCG8 expression[J]. PLoS One, 2023, 18( 6): e0287146. DOI: 10.1371/journal.pone.0287146. |
| [14] |
ZHANG DK, LI YH, HE SF, et al. Association between ABCB4 variants and intrahepatic cholestasis of pregnancy[J]. Sci Rep, 2025, 15( 1): 3300. DOI: 10.1038/s41598-025-87909-5. |
| [15] |
WANG HH, PORTINCASA P, LIU M, et al. Genetic analysis of ABCB4 mutations and variants related to the pathogenesis and pathophysiology of low phospholipid-associated cholelithiasis[J]. Genes(Basel), 2022, 13( 6): 1047. DOI: 10.3390/genes13061047. |
| [16] |
NAYAGAM JS, FOSKETT P, STRAUTNIEKS S, et al. Clinical phenotype of adult-onset liver disease in patients with variants in ABCB4, ABCB11, and ATP8B1[J]. Hepatol Commun, 2022, 6( 10): 2654- 2664. DOI: 10.1002/hep4.2051. |
| [17] |
REN ZX, ZHAO L, ZHAO ML, et al. Increased intestinal bile acid absorption contributes to age-related cognitive impairment[J]. Cell Rep Med, 2024, 5( 5): 101543. DOI: 10.1016/j.xcrm.2024.101543. |
| [18] |
STICOVA E, JIRSA M. ABCB4 disease: Many faces of one gene deficiency[J]. Ann Hepatol, 2020, 19( 2): 126- 133. DOI: 10.1016/j.aohep.2019.09.010. |
| [19] |
ZHAN L, PAN YZ, CHEN L, et al. Prevalence of ABCB4 polymorphisms in gallstone disease in Han-Chinese population[J]. Am J Transl Res, 2016, 8( 2): 1218- 1227.
|
| [20] |
GUDBJARTSSON DF, HELGASON H, GUDJONSSON SA, et al. Large-scale whole-genome sequencing of the Icelandic population[J]. Nat Genet, 2015, 47( 5): 435- 444. DOI: 10.1038/ng.3247. |
| [21] |
STÄTTERMAYER AF, HALILBASIC E, WRBA F, et al. Variants in ABCB4(MDR3) across the spectrum of cholestatic liver diseases in adults[J]. J Hepatol, 2020, 73( 3): 651- 663. DOI: 10.1016/j.jhep.2020.04.036. |
| [22] |
AVENA A, PUGGELLI S, MORRIS M, et al. ABCB4 variants in adult patients with cholestatic disease are frequent and underdiagnosed[J]. Dig Liver Dis, 2021, 53( 3): 329- 344. DOI: 10.1016/j.dld.2020.12.003. |
| [23] |
ZHANG RS, LIU WJ, ZENG J, et al. Recent advances in the screening methods of NPC1L1 inhibitors[J]. Biomed Pharmacother, 2022, 155: 113732. DOI: 10.1016/j.biopha.2022.113732. |
| [24] |
XU CL, FU FY, SHE YH, et al. NPC1L1 plays a novel role in nonalcoholic fatty liver disease[J]. ACS Omega, 2023, 8( 51): 48586- 48589. DOI: 10.1021/acsomega.3c07337. |
| [25] |
HU MQ, YANG F, HUANG YW, et al. Structural insights into the mechanism of human NPC1L1-mediated cholesterol uptake[J]. Sci Adv, 2021, 7( 29): eabg3188. DOI: 10.1126/sciadv.abg3188. |
| [26] |
GE L, QI W, WANG LJ, et al. Flotillins play an essential role in Niemann-Pick C1-like 1-mediated cholesterol uptake[J]. Proc Natl Acad Sci USA, 2011, 108( 2): 551- 556. DOI: 10.1073/pnas.1014434108. |
| [27] |
GE L, WANG J, QI W, et al. The cholesterol absorption inhibitor ezetimibe acts by blocking the sterol-induced internalization of NPC1L1[J]. Cell Metab, 2008, 7( 6): 508- 519. DOI: 10.1016/j.cmet.2008.04.001. |
| [28] |
XIAO J, DONG LW, LIU S, et al. Bile acids-mediated intracellular cholesterol transport promotes intestinal cholesterol absorption and NPC1L1 recycling[J]. Nat Commun, 2023, 14( 1): 6469. DOI: 10.1038/s41467-023-42179-5. |
| [29] |
ZHANG YY, FU ZY, WEI J, et al. A LIMA1 variant promotes low plasma LDL cholesterol and decreases intestinal cholesterol absorption[J]. Science, 2018, 360( 6393): 1087- 1092. DOI: 10.1126/science.aao6575. |
| [30] |
WU J, CUI W, CAI Q, et al. The NPC1L1 polymorphism 1679C>G is associated with gallstone disease in Chinese patients[J]. PLoS One, 2016, 11( 1): e0147562. DOI: 10.1371/journal.pone.0147562. |
| [31] |
HUANG CS, YU XC, FORDSTROM P, et al. Cryo-EM structures of NPC1L1 reveal mechanisms of cholesterol transport and ezetimibe inhibition[J]. Sci Adv, 2020, 6( 25): eabb1989. DOI: 10.1126/sciadv.abb1989. |
| [32] |
NISSINEN MJ, PITKÄNEN N, SIMONEN P, et al. Genetic polymorphism of sterol transporters in children with future gallstones[J]. Dig Liver Dis, 2018, 50( 9): 954- 960. DOI: 10.1016/j.dld.2018.04.007. |
| [33] |
LAURIDSEN BK, STENDER S, FRIKKE-SCHMIDT R, et al. Genetic variation in the cholesterol transporter NPC1L1, ischaemic vascular disease, and gallstone disease[J]. Eur Heart J, 2015, 36( 25): 1601- 1608. DOI: 10.1093/eurheartj/ehv108. |
| [34] |
CANNON CP, BLAZING MA, GIUGLIANO RP, et al. Ezetimibe added to statin therapy after acute coronary syndromes[J]. N Engl J Med, 2015, 372( 25): 2387- 2397. DOI: 10.1056/NEJMoa1410489. |
| [35] |
SHEN WY, SHAO WT, WANG QH, et al. Dietary diosgenin transcriptionally down-regulated intestinal NPC1L1 expression to prevent cholesterol gallstone formation in mice[J]. J Biomed Sci, 2023, 30( 1): 44. DOI: 10.1186/s12929-023-00933-3. |
| [36] |
SONG B, LIU NQ, CHENG Y, et al. Generation of induced pluripotent stem cell GZHMCi002-A from peripheral blood mononuclear cells with APOB mutation[J]. Stem Cell Res, 2020, 49: 102054. DOI: 10.1016/j.scr.2020.102054. |
| [37] |
GIANAZZA E, ZOANNI B, MALLIA A, et al. Proteomic studies on apoB-containing lipoprotein in cardiovascular research: A comprehensive review[J]. Mass Spectrom Rev, 2023, 42( 4): 1397- 1423. DOI: 10.1002/mas.21747. |
| [38] |
STRØM TB, ASPRUSTEN E, LAERDAHL JK, et al. Missense mutation Q384K in the APOB gene affecting the large lipid transfer module of apoB reduces the secretion of apoB-100 in the liver without reducing the secretion of apoB-48 in the intestine[J]. J Clin Lipidol, 2023, 17( 6): 800- 807. DOI: 10.1016/j.jacl.2023.08.009. |
| [39] |
NIU CQ, LUO Z, YU LQ, et al. Associations of the APOB rs693 and rs17240441 polymorphisms with plasma APOB and lipid levels: A meta-analysis[J]. Lipids Health Dis, 2017, 16( 1): 166. DOI: 10.1186/s12944-017-0558-7. |
| [40] |
CHAUHAN T, MITTAL RD, MITTAL B. Association of common single nucleotide polymorphisms of candidate genes with gallstone disease: A meta-analysis[J]. Indian J Clin Biochem, 2020, 35( 3): 290- 311. DOI: 10.1007/s12291-019-00832-1. |
| [41] |
ZHU HF, YU LH, FENG LS. Association of apolipoprotein B XbaI(rs693) polymorphism and gallstone disease risk based on a comprehensive analysis[J]. Genes Environ, 2021, 43( 1): 17. DOI: 10.1186/s41021-021-00189-z. |
| [42] |
KACPERCZYK M, KMIECIAK A, KRATZ EM. The role of ApoE expression and variability of its glycosylation in human reproductive health in the light of current information[J]. Int J Mol Sci, 2021, 22( 13): 7197. DOI: 10.3390/ijms22137197. |
| [43] |
NASCIMENTO JCR, MATOS GA, PEREIRA LC, et al. Impact of apolipoprotein E genetic polymorphisms on liver disease: An essential review[J]. Ann Hepatol, 2020, 19( 1): 24- 30. DOI: 10.1016/j.aohep.2019.07.011. |
| [44] |
KOTHARI S, BALA N, PATEL AB, et al. The LDL receptor binding domain of apolipoprotein E directs the relative orientation of its C-terminal segment in reconstituted nascent HDL[J]. Biochim Biophys Acta Biomembr, 2021, 1863( 7): 183618. DOI: 10.1016/j.bbamem.2021.183618. |
| [45] |
XUE P, NIU WQ, JIANG ZY, et al. A meta-analysis of apolipoprotein E gene ε2/ε3/ε4 polymorphism for gallbladder stone disease[J]. PLoS One, 2012, 7( 9): e45849. DOI: 10.1371/journal.pone.0045849. |
| [46] |
LUMSDEN AL, MULUGETA A, ZHOU A, et al. Apolipoprotein E(APOE) genotype-associated disease risks: A phenome-wide, registry-based, case-control study utilising the UK Biobank[J]. EBioMedicine, 2020, 59: 102954. DOI: 10.1016/j.ebiom.2020.102954. |
| [47] |
DWIVEDI S, MADESHIYA AK, SINGH S, et al. Association of APOE-219G>T and-427T>C polymorphic variants in transcriptional regulatory region of APOE gene with gallbladder stone: A north Indian case-control study[J]. Meta Gene, 2018, 16: 248- 254. DOI: 10.1016/j.mgene.2018.04.002. |
| [48] |
SUN LB, ZHANG YH, LI WY, et al. Mucin glycans: A target for cancer therapy[J]. Molecules, 2023, 28( 20): 7033. DOI: 10.3390/molecules28-207033. |
| [49] |
YOO KS, CHOI HS, JUN DW, et al. MUC expression in gallbladder epithelial tissues in cholesterol-associated gallbladder disease[J]. Gut Liver, 2016, 10( 5): 851- 858. DOI: 10.5009/gnl15600. |
| [50] |
CHUANG SC, HSI E, LEE KT. Mucin genes in gallstone disease[J]. Clin Chim Acta, 2012, 413( 19-20): 1466- 1471. DOI: 10.1016/j.cca.2012.06.015. |
| [51] |
CHUANG SC, JUO SH, HSI E, et al. Multiple mucin genes polymorphisms are associated with gallstone disease in Chinese men[J]. Clin Chim Acta, 2011, 412( 7-8): 599- 603. DOI: 10.1016/j.cca.2010.12.008. |
| [52] |
REN GQ, FAN YM, ZHONG RZ, et al. Relationship between mucin gene polymorphisms and different types of gallbladder stones[J]. BMC Med Genomics, 2025, 18( 1): 22. DOI: 10.1186/s12920-025-02090-y. |






 DownLoad:
DownLoad: