| [1] |
WANG FS, FAN JG, ZHANG Z, et al. The global burden of liver disease: The major impact of China[J]. Hepatology, 2014, 60( 6): 2099- 2108. DOI: 10.1002/hep.27406. |
| [2] |
DEVARBHAVI H, ASRANI SK, ARAB JP, et al. Global burden of liver disease: 2023 update[J]. J Hepatol, 2023, 79( 2): 516- 537. DOI: 10.1016/j.jhep.2023.03.017. |
| [3] |
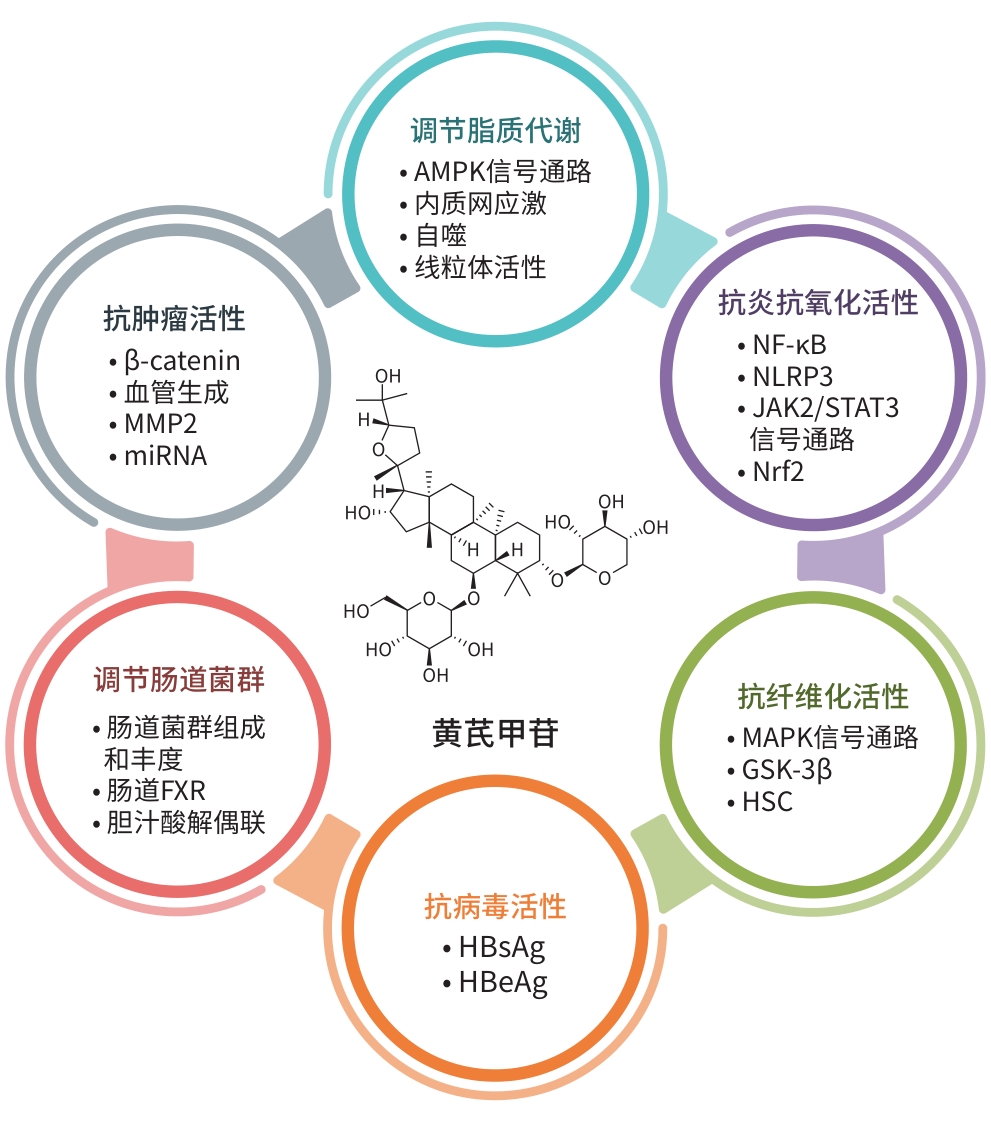
SHI H, ZHOU P, GAO G, et al. Astragaloside IV prevents acute myocardial infarction by inhibiting the TLR4/MyD88/NF-κB signaling pathway[J]. J Food Biochem, 2021, 45( 7): e13757. DOI: 10.1111/jfbc.13757. |
| [4] |
SHEN Q, FANG J, GUO H, et al. Astragaloside IV attenuates podocyte apoptosis through ameliorating mitochondrial dysfunction by up-regulated Nrf2-ARE/TFAM signaling in diabetic kidney disease[J]. Free Radic Biol Med, 2023, 203: 45- 57. DOI: 10.1016/j.freeradbiomed.2023.03.022. |
| [5] |
GUO JN, LE YF, YUAN AN, et al. Astragaloside IV ameliorates cisplatin-induced liver injury by modulating ferroptosis-dependent pathways[J]. J Ethnopharmacol, 2024, 328: 118080. DOI: 10.1016/j.jep.2024.118080. |
| [6] |
LIU X, DING YP, JIANG CX, et al. Astragaloside IV ameliorates radiation-induced nerve cell damage by activating the BDNF/TrkB signaling pathway[J]. Phytother Res, 2023, 37( 9): 4102- 4116. DOI: 10.1002/ptr.7872. |
| [7] |
WANG JY, PU XY, ZHUANG HW, et al. Astragaloside IV alleviates septic myocardial injury through DUSP1-Prohibitin 2 mediated mitochondrial quality control and ER-autophagy[J]. J Adv Res, 2025, 75: 561- 580. DOI: 10.1016/j.jare.2024.10.030. |
| [8] |
KIM J, YANG G, KIM Y, et al. AMPK activators: Mechanisms of action and physiological activities[J]. Exp Mol Med, 2016, 48( 4): e224. DOI: 10.1038/emm.2016.16. |
| [9] |
ZHOU M, LIU X, WU YJ, et al. Mechanism of astragaloside Ⅳ on db/db mice with type 2 diabetes mellitus and non-alcoholic fatty liver disease based on AMPK signaling pathway[J]. Chin J Exp Tradit Med Form, 2024, 30( 5): 72- 79. DOI: 10.13422/j.cnki.syfjx.20232039. |
| [10] |
ZHOU B, ZHOU DL, WEI XH, et al. Astragaloside IV attenuates free fatty acid-induced ER stress and lipid accumulation in hepatocytes via AMPK activation[J]. Acta Pharmacol Sin, 2017, 38( 7): 998- 1008. DOI: 10.1038/aps.2016.175. |
| [11] |
AJOOLABADY A, KAPLOWITZ N, LEBEAUPIN C, et al. Endoplasmic reticulum stress in liver diseases[J]. Hepatology, 2023, 77( 2): 619- 639. DOI: 10.1002/hep.32562. |
| [12] |
WANG M, KAUFMAN RJ. Protein misfolding in the endoplasmic reticulum as a conduit to human disease[J]. Nature, 2016, 529( 7586): 326- 335. DOI: 10.1038/nature17041. |
| [13] |
LEBEAUPIN C, VALLÉE D, HAZARI Y, et al. Endoplasmic reticulum stress signalling and the pathogenesis of non-alcoholic fatty liver disease[J]. J Hepatol, 2018, 69( 4): 927- 947. DOI: 10.1016/j.jhep.2018.06.008. |
| [14] |
LEE JH, LEE J. Endoplasmic reticulum(ER) stress and its role in pancreatic β-cell dysfunction and senescence in type 2 diabetes[J]. Int J Mol Sci, 2022, 23( 9): 4843. DOI: 10.3390/ijms23094843. |
| [15] |
JALAL IA, ELKHOELY A, MOHAMED SK, et al. Linagliptin and secoisolariciresinol diglucoside attenuate hyperlipidemia and cardiac hypertrophy induced by a high-methionine diet in rats via suppression of hyperhomocysteinemia-induced endoplasmic reticulum stress[J]. Front Pharmacol, 2023, 14: 1275730. DOI: 10.3389/fphar.2023.1275730. |
| [16] |
GLICK D, BARTH S, MACLEOD KF. Autophagy: Cellular and molecular mechanisms[J]. J Pathol, 2010, 221( 1): 3- 12. DOI: 10.1002/path.2697. |
| [17] |
XIAO ZL, LU CX, ZHOU DN, et al. Role of lipophagy in the prevention and treatment of nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2024, 40( 7): 1450- 1458. DOI: 10.12449/JCH240725. 肖智利, 卢晨霞, 周丹妮, 等. 脂肪自噬在非酒精性脂肪性肝病防治中的作用[J]. 临床肝胆病杂志, 2024, 40( 7): 1450- 1458. DOI: 10.12449/JCH240725. |
| [18] |
SINHA RA. Autophagy: A cellular guardian against hepatic lipotoxicity[J]. Genes(Basel), 2023, 14( 3): 553. DOI: 10.3390/genes14030553. |
| [19] |
ZHU YF, SU Y, ZHANG J, et al. Astragaloside IV alleviates liver injury in type 2 diabetes due to promotion of AMPK/mTOR-mediated autophagy[J]. Mol Med Rep, 2021, 23( 6): 437. DOI: 10.3892/mmr.2021.12076. |
| [20] |
LIU G, WANG YH, ZHANG T, et al. Astragaloside-IV promotes autophagy via the Akt/mTOR pathway to improve cellular lipid deposition[J]. Medicine(Baltimore), 2024, 103( 16): e37846. DOI: 10.1097/MD.0000000000037846. |
| [21] |
MANSOURI A, GATTOLLIAT CH, ASSELAH T. Mitochondrial dysfunction and signaling in chronic liver diseases[J]. Gastroenterology, 2018, 155( 3): 629- 647. DOI: 10.1053/j.gastro.2018.06.083. |
| [22] |
LUO ZX, WANG YQ, XUE MZ, et al. Astragaloside IV ameliorates fat metabolism in the liver of ageing mice through targeting mitochondrial activity[J]. J Cell Mol Med, 2021, 25( 18): 8863- 8876. DOI: 10.1111/jcmm.16847. |
| [23] |
VALENTA T, HAUSMANN G, BASLER K. The many faces and functions of β-catenin[J]. EMBO J, 2012, 31( 12): 2714- 2736. DOI: 10.1038/emboj.2012.150. |
| [24] |
HE T, WANG FF, LIU ZQ, et al. Astragaloside affects HepG-2 cell proliferation and apoptosis through Wnt/β-catenin pathway[J]. World Chin Med, 2020, 15( 24): 3787- 3791. DOI: 10.3969/j.issn.1673-7202.2020.24.011. |
| [25] |
QIN CD, MA DN, REN ZG, et al. Astragaloside IV inhibits metastasis in hepatoma cells through the suppression of epithelial-mesenchymal transition via the Akt/GSK-3β/β-catenin pathway[J]. Oncol Rep, 2017, 37( 3): 1725- 1735. DOI: 10.3892/or.2017.5389. |
| [26] |
|
| [27] |
ZHANG S, TANG DC, ZANG WH, et al. Synergistic inhibitory effect of traditional Chinese medicine astragaloside IV and curcumin on tumor growth and angiogenesis in an orthotopic nude-mouse model of human hepatocellular carcinoma[J]. Anticancer Res, 2017, 37( 2): 465- 473. DOI: 10.21873/anticanres.11338. |
| [28] |
OGIHARA T, MIZOI K, KAMIOKA H, et al. Physiological roles of ERM proteins and transcriptional regulators in supporting membrane expression of efflux transporters as factors of drug resistance in cancer[J]. Cancers(Basel), 2020, 12( 11): 3352. DOI: 10.3390/cancers12113352. |
| [29] |
LESLIE EM, DEELEY RG, COLE SPC. Multidrug resistance proteins: Role of P-glycoprotein, MRP1, MRP2, and BCRP(ABCG2) in tissue defense[J]. Toxicol Appl Pharmacol, 2005, 204( 3): 216- 237. DOI: 10.1016/j.taap.2004.10.012. |
| [30] |
QU XY, GAO H, ZHAI JH, et al. Astragaloside IV enhances cisplatin chemosensitivity in hepatocellular carcinoma by suppressing MRP2[J]. Eur J Pharm Sci, 2020, 148: 105325. DOI: 10.1016/j.ejps.2020.105325. |
| [31] |
FU YJ, MACKOWIAK B, FENG DC, et al. MicroRNA-223 attenuates hepatocarcinogenesis by blocking hypoxia-driven angiogenesis and immunosuppression[J]. Gut, 2023, 72( 10): 1942- 1958. DOI: 10.1136/gutjnl-2022-327924. |
| [32] |
YUAN ML, ZHANG XS, YUE FX, et al. CircNOLC1 promotes colorectal cancer liver metastasis by interacting with AZGP1 and sponging miR-212-5p to regulate reprogramming of the oxidative pentose phosphate pathway[J]. Adv Sci(Weinh), 2023, 10( 33): e2205229. DOI: 10.1002/advs.202205229. |
| [33] |
DINAMI R, POMPILI L, PETTI E, et al. MiR-182-3p targets TRF2 and impairs tumor growth of triple-negative breast cancer[J]. EMBO Mol Med, 2023, 15( 1): e16033. DOI: 10.15252/emmm.202216033. |
| [34] |
MA Y, LI Y, WU TT, et al. Astragaloside IV attenuates programmed death-ligand 1-mediated immunosuppression during liver cancer development via the miR-135b-5p/CNDP1 axis[J]. Cancers(Basel), 2023, 15( 20): 5048. DOI: 10.3390/cancers15205048. |
| [35] |
MIN YQ, LI S, LIU XH, et al. Research advances in the cascade interaction between reactive oxygen species/reactive nitrogen species and the NF-κB signaling pathway in liver fibrosis[J]. J Clin Hepatol, 2023, 39( 6): 1454- 1460. DOI: 10.3969/j.issn.1001-5256.2023.06.031. |
| [36] |
CHENG MX, CHEN ZZ, CAI YL, et al. Astragaloside IV protects against ischemia reperfusion in a murine model of orthotopic liver transplantation[J]. Transplant Proc, 2011, 43( 5): 1456- 1461. DOI: 10.1016/j.transproceed.2011.02.066. |
| [37] |
LIU YL, ZHANG QZ, WANG YR, et al. Astragaloside IV improves high-fat diet-induced hepatic steatosis in nonalcoholic fatty liver disease rats by regulating inflammatory factors level via TLR4/NF-κB signaling pathway[J]. Front Pharmacol, 2021, 11: 605064. DOI: 10.3389/fphar.2020.605064. |
| [38] |
|
| [39] |
WU S, WEN F, ZHONG XB, et al. Astragaloside IV ameliorate acute alcohol-induced liver injury in mice via modulating gut microbiota and regulating NLRP3/caspase-1 signaling pathway[J]. Ann Med, 2023, 55( 1): 2216942. DOI: 10.1080/07853890.2023.2216942. |
| [40] |
DING YP, DONG XQ, YIFAN MA, et al. Astragaloside IV plays a role in reducing radiation-induced liver inflammation in mice by inhibiting thioredoxin-interacting protein/nod-like receptor protein 3 signaling pathway[J]. J Tradit Chin Med, 2023, 43( 1): 87- 94. DOI: 10.19852/j.cnki.jtcm.2023.01.008. |
| [41] |
QU XY, GAO H, TAO LN, et al. Astragaloside IV protects against cisplatin-induced liver and kidney injury via autophagy-mediated inhibition of NLRP3 in rats[J]. J Toxicol Sci, 2019, 44( 3): 167- 175. DOI: 10.2131/jts.44.167. |
| [42] |
YAN Y, ZHANG LB, MA R, et al. Jolkinolide B ameliorates rheumatoid arthritis by regulating the JAK2/STAT3 signaling pathway[J]. Phytomedicine, 2024, 124: 155311. DOI: 10.1016/j.phymed.2023.155311. |
| [43] |
ZHANG HY, CHANG XR. Astragaloside Ⅳ inhibits JAK2/STAT3 signaling pathway and alleviates severe acute pancreatitis-associated acute liver injury in rats[J]. Chin J Pathophysiol, 2016, 32( 6): 984- 989. DOI: 10.3969/j.issn.1000-4718.2016.06.004. |
| [44] |
LI XM, WANG XL, HAN CY, et al. Astragaloside IV suppresses collagen production of activated hepatic stellate cells via oxidative stress-mediated p38 MAPK pathway[J]. Free Radic Biol Med, 2013, 60: 168- 176. DOI: 10.1016/j.freeradbiomed.2013.02.027. |
| [45] |
ZHAO XM, ZHANG J, LIANG YN, et al. Astragaloside IV synergizes with ferulic acid to alleviate hepatic fibrosis in bile duct-ligated cirrhotic rats[J]. Dig Dis Sci, 2020, 65( 10): 2925- 2936. DOI: 10.1007/s10620-019-06017-3. |
| [46] |
EZHILARASAN D. Hepatic stellate cells in the injured liver: Perspectives beyond hepatic fibrosis[J]. J Cell Physiol, 2022, 237( 1): 436- 449. DOI: 10.1002/jcp.30582. |
| [47] |
WANG SG, LI JY, HUANG H, et al. Anti-hepatitis B virus activities of astragaloside IV isolated from Radix Astragali[J]. Biol Pharm Bull, 2009, 32( 1): 132- 135. DOI: 10.1248/bpb.32.132. |
| [48] |
ZHAI YY, ZHOU WL, YAN X, et al. Astragaloside IV ameliorates diet-induced hepatic steatosis in obese mice by inhibiting intestinal FXR via intestinal flora remodeling[J]. Phytomedicine, 2022, 107: 154444. DOI: 10.1016/j.phymed.2022.154444. |
| [49] |
NIU KQ, CHANG H, LYU GF, et al. Inhibitory effect of astragaloside Ⅳ on cisplatin-induced liver injury in mice and its mechanism[J]. J Jilin Univ(Med Ed), 2025, 51( 2): 370- 377. DOI: 10.13481/j.1671-587X.20250211. |
| [50] |
LI L, HUANG WX, WANG SK, et al. Astragaloside IV attenuates acetaminophen-induced liver injuries in mice by activating the Nrf2 signaling pathway[J]. Molecules, 2018, 23( 8): 2032. DOI: 10.3390/molecules23082032. |






 DownLoad:
DownLoad: