| [1] |
GADD VL, ALEKSIEVA N, FORBES SJ. Epithelial plasticity during liver injury and regeneration[J]. Cell Stem Cell, 2020, 27( 4): 557- 573. DOI: 10.1016/j.stem.2020.08.016. |
| [2] |
|
| [3] |
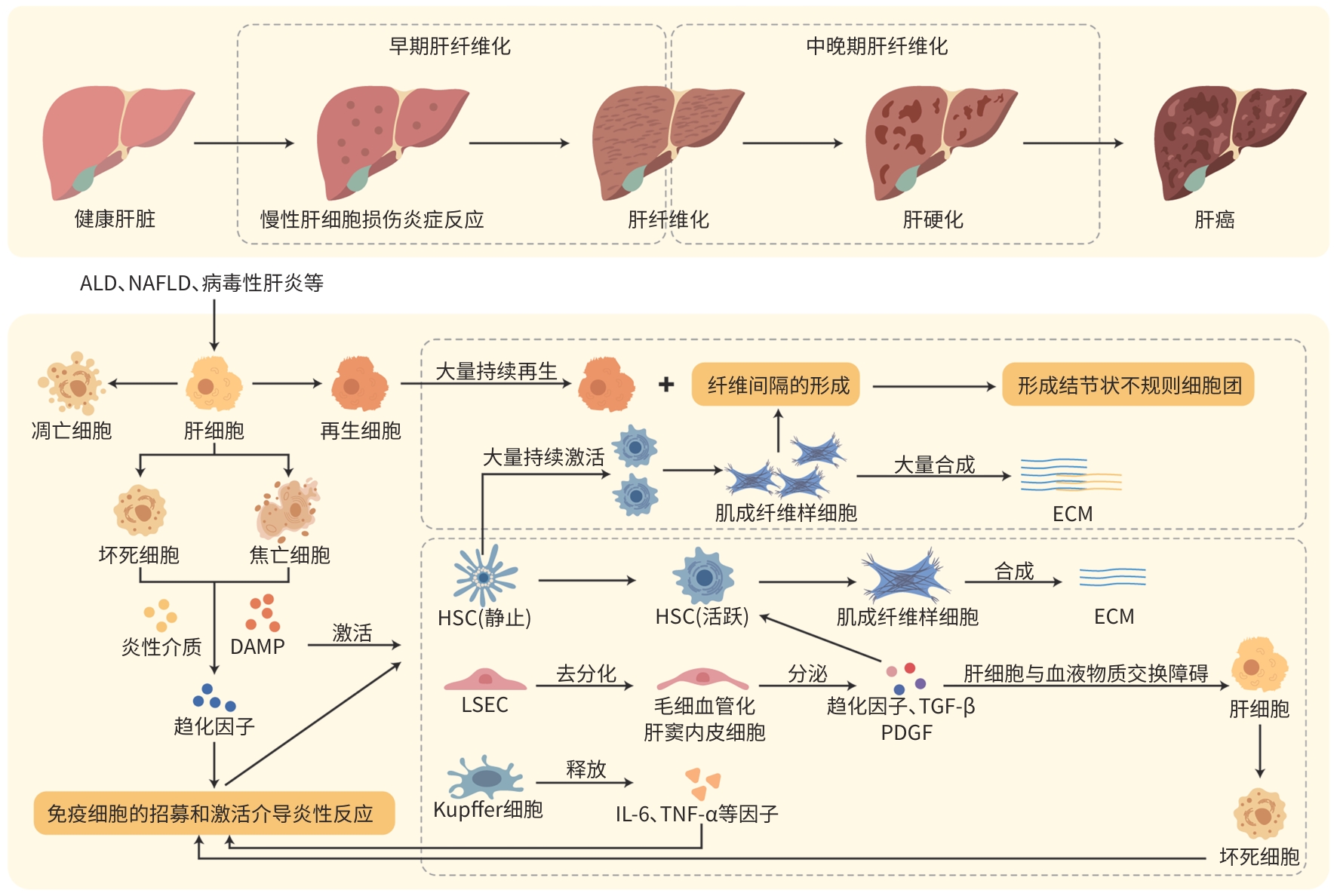
BATALLER R, BRENNER DA. Liver fibrosis[J]. J Clin Invest, 2005, 115( 2): 209- 218. DOI: 10.1172/jci24282. |
| [4] |
KUMAR S, DUAN QH, WU RX, et al. Pathophysiological communication between hepatocytes and non-parenchymal cells in liver injury from NAFLD to liver fibrosis[J]. Adv Drug Deliv Rev, 2021, 176: 113869. DOI: 10.1016/j.addr.2021.113869. |
| [5] |
WU BC, SODJI QH, OYELERE AK. Inflammation, fibrosis and cancer: Mechanisms, therapeutic options and challenges[J]. Cancers(Basel), 2022, 14( 3): 552. DOI: 10.3390/cancers14030552. |
| [6] |
LI Y, LU LG, CAI XB. Liver regeneration and cell transplantation for end-stage liver disease[J]. Biomolecules, 2021, 11( 12): 1907. DOI: 10.3390/biom11121907. |
| [7] |
DHAR D, BAGLIERI J, KISSELEVA T, et al. Mechanisms of liver fibrosis and its role in liver cancer[J]. Exp Biol Med(Maywood), 2020, 245( 2): 96- 108. DOI: 10.1177/1535370219898141. |
| [8] |
HIGASHI T, FRIEDMAN SL, HOSHIDA Y. Hepatic stellate cells as key target in liver fibrosis[J]. Adv Drug Deliv Rev, 2017, 121: 27- 42. DOI: 10.1016/j.addr.2017.05.007. |
| [9] |
MATSUDA M, SEKI E. Hepatic stellate cell-macrophage crosstalk in liver fibrosis and carcinogenesis[J]. Semin Liver Dis, 2020, 40( 3): 307- 320. DOI: 10.1055/s-0040-1708876. |
| [10] |
de HAAN W, DHEEDENE W, APELT K, et al. Endothelial Zeb2 preserves the hepatic angioarchitecture and protects against liver fibrosis[J]. Cardiovasc Res, 2022, 118( 5): 1262- 1275. DOI: 10.1093/cvr/cvab148. |
| [11] |
ROEHLEN N, CROUCHET E, BAUMERT TF. Liver fibrosis: Mechanistic concepts and therapeutic perspectives[J]. Cells, 2020, 9( 4): 875. DOI: 10.3390/cells9040875. |
| [12] |
MURAO A, AZIZ M, WANG HC, et al. Release mechanisms of major DAMPs[J]. Apoptosis, 2021, 26( 3-4): 152- 162. DOI: 10.1007/s10495-021-01663-3. |
| [13] |
SHI JJ, ZHAO Y, WANG K, et al. Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death[J]. Nature, 2015, 526( 7575): 660- 665. DOI: 10.1038/nature15514. |
| [14] |
HE S, TANG SL. WNT/β-catenin signaling in the development of liver cancers[J]. Biomed Pharmacother, 2020, 132: 110851. DOI: 10.1016/j.biopha.2020.110851. |
| [15] |
MACDONALD BT, TAMAI K, HE X. Wnt/beta-catenin signaling: Components, mechanisms, and diseases[J]. Dev Cell, 2009, 17( 1): 9- 26. DOI: 10.1016/j.devcel.2009.06.016. |
| [16] |
TESTERINK N, AJAT M, HOUWELING M, et al. Replacement of retinyl esters by polyunsaturated triacylglycerol species in lipid droplets of hepatic stellate cells during activation[J]. PLoS One, 2012, 7( 4): e34945. DOI: 10.1371/journal.pone.0034945. |
| [17] |
|
| [18] |
MOUNTFORD S, EFFENBERGER M, NOLL-PUCHTA H, et al. Modulation of Liver Inflammation and Fibrosis by Interleukin-37[J]. Front Immunol, 2021, 12: 603649. DOI: 10.3389/fimmu.2021.603649. |
| [19] |
YU YS, LIU Y, AN WS, et al. STING-mediated inflammation in Kupffer cells contributes to progression of nonalcoholic steatohepatitis[J]. J Clin Invest, 2019, 129( 2): 546- 555. DOI: 10.1172/JCI121842. |
| [20] |
FILLIOL A, PIQUET-PELLORCE C, RAGUÉNÈS-NICOL C, et al. RIPK1 protects hepatocytes from Kupffer cells-mediated TNF-induced apoptosis in mouse models of PAMP-induced hepatitis[J]. J Hepatol, 2017, 66( 6): 1205- 1213. DOI: 10.1016/j.jhep.2017.01.005. |
| [21] |
MAY D, DJONOV V, ZAMIR G, et al. A transgenic model for conditional induction and rescue of portal hypertension reveals a role of VEGF-mediated regulation of sinusoidal fenestrations[J]. PLoS One, 2011, 6( 7): e21478. DOI: 10.1371/journal.pone.0021478. |
| [22] |
FABREGAT I, CABALLERO-DÍAZ D. Transforming growth factor-β- induced cell plasticity in liver fibrosis and hepatocarcinogenesis[J]. Front Oncol, 2018, 8: 357. DOI: 10.3389/fonc.2018.00357. |
| [23] |
RODRÍGUEZ-RODRÍGUEZ DR, LOZANO-SEPULVEDA SA, DELGADO-MONTEMAYOR C, et al. Turnera diffusa extract attenuates profibrotic, extracellular matrix and mitochondrial markers in activated human hepatic stellate cells(HSC)[J]. Ann Hepatol, 2021, 22: 100281. DOI: 10.1016/j.aohep.2020.10.009. |
| [24] |
YANG CM, YANG CC, HSU WH, et al. Tumor necrosis factor-α-induced C-C motif chemokine ligand 20 expression through TNF receptor 1-dependent activation of EGFR/p38 MAPK and JNK1/2/FoxO1 or the NF-κB pathway in human cardiac fibroblasts[J]. Int J Mol Sci, 2022, 23( 16): 9086. DOI: 10.3390/ijms23169086. |
| [25] |
YAMASHITA M, PASSEGUÉ E. TNF-α coordinates hematopoietic stem cell survival and myeloid regeneration[J]. Cell Stem Cell, 2019, 25( 3): 357- 372. e 7. DOI: 10.1016/j.stem.2019.05.019. |
| [26] |
SCHMIDT-ARRAS D, ROSE-JOHN S. IL-6 pathway in the liver: From physiopathology to therapy[J]. J Hepatol, 2016, 64( 6): 1403- 1415. DOI: 10.1016/j.jhep.2016.02.004. |
| [27] |
YOUSEFI A, NAJAFI M, MOTAMED F, et al. Association of interleukin-6 and interleukin-1 family gene polymorphisms in autoimmune hepatitis[J]. Ann Hepatol, 2018, 17( 6): 1021- 1025. DOI: 10.5604/01.3001.0012.7202. |
| [28] |
KARLMARK KR, WEISKIRCHEN R, ZIMMERMANN HW, et al. Hepatic recruitment of the inflammatory Gr1+ monocyte subset upon liver injury promotes hepatic fibrosis[J]. Hepatology, 2009, 50( 1): 261- 274. DOI: 10.1002/hep.22950. |
| [29] |
KONG DS, ZHANG ZL, CHEN LP, et al. Curcumin blunts epithelial-mesenchymal transition of hepatocytes to alleviate hepatic fibrosis through regulating oxidative stress and autophagy[J]. Redox Biol, 2020, 36: 101600. DOI: 10.1016/j.redox.2020.101600. |
| [30] |
YING HZ, CHEN Q, ZHANG WY, et al. PDGF signaling pathway in hepatic fibrosis pathogenesis and therapeutics(Review)[J]. Mol Med Rep, 2017, 16( 6): 7879- 7889. DOI: 10.3892/mmr.2017.7641. |
| [31] |
WISZNIAK S, SCHWARZ Q. Exploring the intracrine functions of VEGF-A[J]. Biomolecules, 2021, 11( 1): 128. DOI: 10.3390/biom11010128. |
| [32] |
ZHOU WC, ZHANG QB, QIAO L. Pathogenesis of liver cirrhosis[J]. World J Gastroenterol, 2014, 20( 23): 7312- 7324. DOI: 10.3748/wjg.v20.i23.7312. |
| [33] |
IWAKIRI Y. Pathophysiology of portal hypertension[J]. Clin Liver Dis, 2014, 18( 2): 281- 291. DOI: 10.1016/j.cld.2013.12.001. |
| [34] |
GRESSNER AM, WEISKIRCHEN R. Modern pathogenetic concepts of liver fibrosis suggest stellate cells and TGF-beta as major players and therapeutic targets[J]. J Cell Mol Med, 2006, 10( 1): 76- 99. DOI: 10.1111/j.1582-4934.2006.tb00292.x. |
| [35] |
WOHLLEBER D, KNOLLE PA. The role of liver sinusoidal cells in local hepatic immune surveillance[J]. Clin Transl Immunology, 2016, 5( 12): e117. DOI: 10.1038/cti.2016.74. |
| [36] |
JEONG WI, PARK O, RADAEVA S, et al. STAT1 inhibits liver fibrosis in mice by inhibiting stellate cell proliferation and stimulating NK cell cytotoxicity[J]. Hepatology, 2006, 44( 6): 1441- 1451. DOI: 10.1002/hep.21419. |
| [37] |
MCCONNELL MJ, KOSTALLARI E, IBRAHIM SH, et al. The evolving role of liver sinusoidal endothelial cells in liver health and disease[J]. Hepatology, 2023, 78( 2): 649- 669. DOI: 10.1097/HEP.0000000000000207. |
| [38] |
MARTIN IV, BORKHAM-KAMPHORST E, ZOK S, et al. Platelet-derived growth factor(PDGF)-C neutralization reveals differential roles of PDGF receptors in liver and kidney fibrosis[J]. Am J Pathol, 2013, 182( 1): 107- 117. DOI: 10.1016/j.ajpath.2012.09.006. |
| [39] |
MENG Y, ZHAO T, ZHANG ZY, et al. The role of hepatic microenvironment in hepatic fibrosis development[J]. Ann Med, 2022, 54( 1): 2830- 2844. DOI: 10.1080/07853890.2022.2132418. |
| [40] |
DU WJ, ZHEN JH, ZENG ZQ, et al. Expression of interleukin-17 associated with disease progression and liver fibrosis with hepatitis B virus infection: IL-17 in HBV infection[J]. Diagn Pathol, 2013, 8: 40. DOI: 10.1186/1746-1596-8-40. |
| [41] |
YANG WC, WANG YX, ZHANG CG, et al. Maresin1 protect against ferroptosis-induced liver injury through ROS inhibition and Nrf2/HO-1/GPX4 activation[J]. Front Pharmacol, 2022, 13: 865689. DOI: 10.3389/fphar.2022.865689. |
| [42] |
YUAN SY, WEI C, LIU GF, et al. Sorafenib attenuates liver fibrosis by triggering hepatic stellate cell ferroptosis via HIF-1α/SLC7A11 pathway[J]. Cell Prolif, 2022, 55( 1): e13158. DOI: 10.1111/cpr.13158. |
| [43] |
NAGARAJA T, CHEN L, BALASUBRAMANIAN A, et al. Correction: Activation of the connective tissue growth factor(CTGF)-transforming growth factor β1(TGF-β1) axis in hepatitis C virus-expressing hepatocytes[J]. PLoS One, 2023, 18( 8): e0290786. DOI: 10.1371/journal.pone.0290786. |
| [44] |
LIEPELT A, TACKE F. Stromal cell-derived factor-1(SDF-1) as a target in liver diseases[J]. Am J Physiol Gastrointest Liver Physiol, 2016, 311( 2): G203- G209. DOI: 10.1152/ajpgi.00193.2016. |






 DownLoad:
DownLoad: