| [1] |
HU CY, MO ZX. Research progress on pharmacological actions and mechanism of berberine[J]. China Ind Econ, 2017, 23( 20): 213- 219. DOI: 10.13422/j.cnki.syfjx.2017200213. |
| [2] |
WONGBUTDEE J. Physiological effects of berberine[J]. Thai Pharm Health Sci J, 2008( 4): 78- 83.
|
| [3] |
YAO J, KONG WJ, JIANG JD. Learning from berberine: Treating chronic diseases through multiple targets[J]. Sci China Life Sci, 2015, 58( 9): 854- 859. DOI: 10.1007/s11427-013-4568-z. |
| [4] |
SHEN QM. Physiological function of liver[J]. Liver Dr, 2022( 4): 35- 37.
沈启明. 肝脏的生理功能[J]. 肝博士, 2022( 4): 35- 37.
|
| [5] |
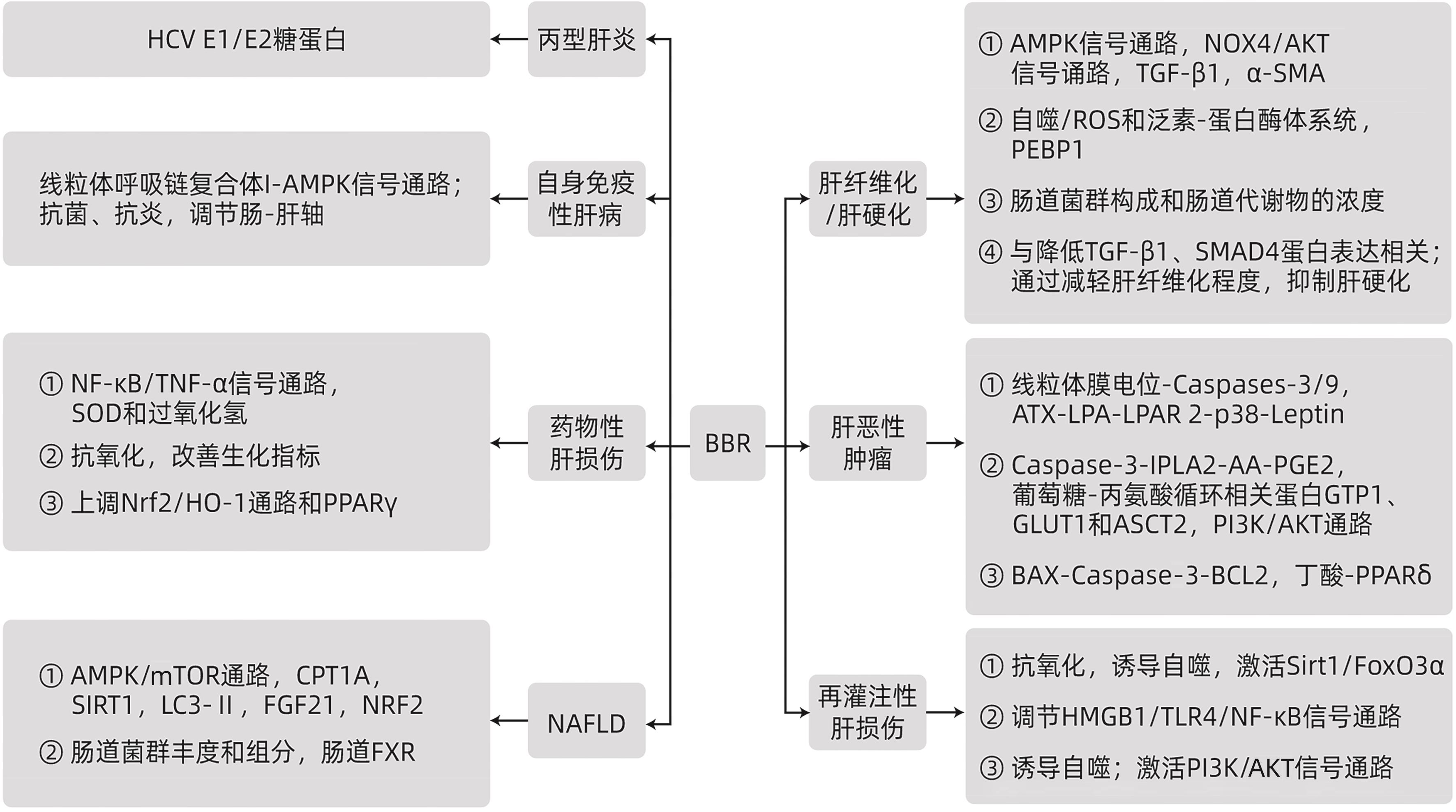
ZHOU MT, DENG Y, LIU MC, et al. The pharmacological activity of berberine, a review for liver protection[J]. Eur J Pharmacol, 2021, 890: 173655. DOI: 10.1016/j.ejphar.2020.173655. |
| [6] |
LAN SH, TANG QY, LI NN, et al. Mechanism of action of Xiaochaihu Decoction in the treatment of hepatitis B based on network pharmacology[J]. J Clin Hepatol, 2021, 37( 10): 2308- 2315. DOI: 10.3969/j.issn.1001-5256.2021.10.010. |
| [7] |
|
| [8] |
LI F, LI B, ZHU QY. Research progress on the epidemiological characteristics and diagnosis of hepatitis C in China[J]. Int J Virol, 2023, 30( 6): 509- 511. DOI: 10.3760/cma.j.issn.1673-4092.2023.06.014. |
| [9] |
HUNG TC, JASSEY A, LIU CH, et al. Berberine inhibits hepatitis C virus entry by targeting the viral E2 glycoprotein[J]. Phytomedicine, 2019, 53: 62- 69. DOI: 10.1016/j.phymed.2018.09.025. |
| [10] |
WANG YY, ZHOU L, LI YN, et al. The effects of berberine on concanavalin A-induced autoimmune hepatitis(AIH) in mice and the adenosine 5'-monophosphate(AMP)-activated protein kinase(AMPK) pathway[J]. Med Sci Monit, 2017, 23: 6150- 6161. DOI: 10.12659/msm.907377. |
| [11] |
KOWDLEY KV, FORMAN L, EKSTEEN B, et al. A randomized, dose-finding, proof-of-concept study of berberine ursodeoxycholate in patients with primary sclerosing cholangitis[J]. Am J Gastroenterol, 2022, 117( 11): 1805- 1815. DOI: 10.14309/ajg.0000000000001956. |
| [12] |
PHOGAT A, SINGH J, KUMAR V, et al. Berberine mitigates acetamiprid-induced hepatotoxicity and inflammation via regulating endogenous antioxidants and NF-κB/TNF-α signaling in rats[J]. Environ Sci Pollut Res Int, 2023, 30( 37): 87412- 87423. DOI: 10.1007/s11356-023-28279-1. |
| [13] |
MAHMOUD AM, HOZAYEN WG, RAMADAN SM. Berberine ameliorates methotrexate-induced liver injury by activating Nrf2/HO-1 pathway and PPARγ, and suppressing oxidative stress and apoptosis in rats[J]. Biomed Pharmacother, 2017, 94: 280- 291. DOI: 10.1016/j.biopha.2017.07.101. |
| [14] |
KOPERSKA A, WESOŁEK A, MOSZAK M, et al. Berberine in non-alcoholic fatty liver disease-a review[J]. Nutrients, 2022, 14( 17): 3459. DOI: 10.3390/nu14173459. |
| [15] |
WANG CE, XU WT, GONG J, et al. Research progress in the treatment of nonalcoholic fatty liver disease[J]. Clin J Med Offic, 2022, 50( 9): 897- 899, 903. DOI: 10.16680/j.1671-3826.2022.09.06. |
| [16] |
ZHU XP, BIAN H, WANG L, et al. Berberine attenuates nonalcoholic hepatic steatosis through the AMPK-SREBP-1c-SCD1 pathway[J]. Free Radic Biol Med, 2019, 141: 192- 204. DOI: 10.1016/j.freeradbiomed.2019.06.019. |
| [17] |
WANG P, LI RK, LI YQ, et al. Berberine alleviates non-alcoholic hepatic steatosis partially by promoting SIRT1 deacetylation of CPT1A in mice[J]. Gastroenterol Rep, 2023, 11: goad032. DOI: 10.1093/gastro/goad032. |
| [18] |
SUN YX, XIA MF, YAN HM, et al. Berberine attenuates hepatic steatosis and enhances energy expenditure in mice by inducing autophagy and fibroblast growth factor 21[J]. Br J Pharmacol, 2018, 175( 2): 374- 387. DOI: 10.1111/bph.14079. |
| [19] |
ZHU L, XU JJ, LI HD, et al. Berberine ameliorates abnormal lipid metabolism via the adenosine monophosphate-activated protein kinase/sirtuin 1 pathway in alcohol-related liver disease[J]. Lab Invest, 2023, 103( 4): 100041. DOI: 10.1016/j.labinv.2022.100041. |
| [20] |
CHEN Y, LI Q, ZHAO SW, et al. Berberine protects mice against type 2 diabetes by promoting PPARγ-FGF21-GLUT2-regulated insulin sensitivity and glucose/lipid homeostasis[J]. Biochem Pharmacol, 2023, 218: 115928. DOI: 10.1016/j.bcp.2023.115928. |
| [21] |
KHATER SI, ALMANAA TN, FATTAH DMA, et al. Liposome-encapsulated berberine alleviates liver injury in type 2 diabetes via promoting AMPK/mTOR-mediated autophagy and reducing ER stress: Morphometric and immunohistochemical scoring[J]. Antioxidants, 2023, 12( 6): 1220. DOI: 10.3390/antiox12061220. |
| [22] |
CAI YJ, YANG QN, YU YQ, et al. Efficacy and underlying mechanisms of berberine against lipid metabolic diseases: A review[J]. Front Pharmacol, 2023, 14: 1283784. DOI: 10.3389/fphar.2023.1283784. |
| [23] |
YUAN XL, WANG J, TANG XY, et al. Berberine ameliorates nonalcoholic fatty liver disease by a global modulation of hepatic mRNA and lncRNA expression profiles[J]. J Transl Med, 2015, 13: 24. DOI: 10.1186/s12967-015-0383-6. |
| [24] |
DAI L, LU S, SHEN TB, et al. Methyltransferase SETD2 mediates hepatoprotection of berberine against steatosis[J]. Ann Transl Med, 2022, 10( 10): 552. DOI: 10.21037/atm-22-1753. |
| [25] |
YANG FJ, GAO RM, LUO XX, et al. Berberine influences multiple diseases by modifying gut microbiota[J]. Front Nutr, 2023, 10: 1187718. DOI: 10.3389/fnut.2023.1187718. |
| [26] |
ZHANG YY, YAN JJ, ZHANG P, et al. Berberine maintains gut microbiota homeostasis and ameliorates liver inflammation in experimental non-alcoholic fatty liver disease[J]. Chin J Gastroenterol, 2018, 23( 4): 209- 215. DOI: 10.3969/j.issn.1008-7125.2018.04.004. |
| [27] |
GUO HH, SHEN HR, WANG LL, et al. Berberine is a potential alternative for metformin with good regulatory effect on lipids in treating metabolic diseases[J]. Biomed Pharmacother, 2023, 163: 114754. DOI: 10.1016/j.biopha.2023.114754. |
| [28] |
WANG C, YANG YT, CHEN JY, et al. Berberine protects against high-energy and low-protein diet-induced hepatic steatosis: Modulation of gut microbiota and bile acid metabolism in laying hens[J]. Int J Mol Sci, 2023, 24( 24): 17304. DOI: 10.3390/ijms242417304. |
| [29] |
YI JZ, WU SY, TAN SW, et al. Berberine alleviates liver fibrosis through inducing ferrous redox to activate ROS-mediated hepatic stellate cells ferroptosis[J]. Cell Death Discov, 2021, 7( 1): 374. DOI: 10.1038/s41420-021-00768-7. |
| [30] |
LI J, PAN Y, KAN MJ, et al. Hepatoprotective effects of berberine on liver fibrosis via activation of AMP-activated protein kinase[J]. Life Sci, 2014, 98( 1): 24- 30. DOI: 10.1016/j.lfs.2013.12.211. |
| [31] |
LIU XZ, WANG LF, TAN SW, et al. Therapeutic effects of berberine on liver fibrosis are associated with lipid metabolism and intestinal flora[J]. Front Pharmacol, 2022, 13: 814871. DOI: 10.3389/fphar.2022.814871. |
| [32] |
XIE ZP, ZHOU Y, LIN M, et al. Binding of berberine to PEBP1 synergizes with sorafenib to induce the ferroptosis of hepatic stellate cells[J]. Amino Acids, 2023, 55( 12): 1867- 1878. DOI: 10.1007/s00726-023-03345-7. |
| [33] |
DOU Q, LI Y, WANG YY, et al. Effect of berberine on protecting liver function and inhibiting inflammation in cirrhotic rats[j]. J Guangzhou Univ Tradit Chin Med, 2021, 38( 12): 2708- 2715. DOI: 10.13359/j.cnki.gzxbtcm.2021.12.027. |
| [34] |
WANG N, FENG YB, ZHU MF, et al. Berberine induces autophagic cell death and mitochondrial apoptosis in liver cancer cells: The cellular mechanism[J]. J Cell Biochem, 2010, 111( 6): 1426- 1436. DOI: 10.1002/jcb.22869. |
| [35] |
REN G, GUO JH, FENG CL, et al. Berberine inhibits carcinogenesis through antagonizing the ATX-LPA-LPAR2-p38-leptin axis in a mouse hepatoma model[J]. Mol Ther Oncolytics, 2022, 26: 372- 386. DOI: 10.1016/j.omto.2022.08.001. |
| [36] |
GUO W, TAN HY, LI S, et al. Glutamic-pyruvic transaminase 1 facilitates alternative fuels for hepatocellular carcinoma growth-a small molecule inhibitor, berberine[J]. Cancers, 2020, 12( 7): 1854. DOI: 10.3390/cancers12071854. |
| [37] |
ZHENG HL. Inhibitory effect of berberine on hepatocellular carcinoma metastasis and its mechanism by suppressing the‘phoenix rising’pathway[D]. Changchun: Jilin University, 2016.
郑慧琳. 黄连素对“凤凰涅槃”信号通路引起肝癌转移的抑制作用及机制探讨[D]. 长春: 吉林大学, 2016.
|
| [38] |
DU HY, GU JY, PENG Q, et al. Berberine suppresses EMT in liver and gastric carcinoma cells through combination with TGFβR regulating TGF-β/smad pathway[J]. Oxid Med Cell Longev, 2021, 2021: 2337818. DOI: 10.1155/2021/2337818. |
| [39] |
SHOU JW, SHAW PC. Berberine activates PPARδ and promotes gut microbiota-derived butyric acid to suppress hepatocellular carcinoma[J]. Phytomedicine, 2023, 115: 154842. DOI: 10.1016/j.phymed.2023.154842. |
| [40] |
LIN YB, SHENG MW, WENG YQ, et al. Berberine protects against ischemia/reperfusion injury after orthotopic liver transplantation via activating Sirt1/FoxO3α induced autophagy[J]. Biochem Biophys Res Commun, 2017, 483( 2): 885- 891. DOI: 10.1016/j.bbrc.2017.01.028. |
| [41] |
GENDY AM, ELNAGAR MR, ALLAM MM, et al. Berberine-loaded nanostructured lipid carriers mitigate warm hepatic ischemia/reperfusion-induced lesion through modulation of HMGB1/TLR4/NF-κB signaling and autophagy[J]. Biomed Pharmacother, 2022, 145: 112122. DOI: 10.1016/j.biopha.2021.112122. |
| [42] |
SHENG M, ZHOU Y, YU W, et al. Protective effect of Berberine pretreatment in hepatic ischemia/reperfusion injury of rat[J]. Transplant Proc, 2015, 47( 2): 275- 282. DOI: 10.1016/j.transproceed.2015.01.010. |







 DownLoad:
DownLoad: