| [1] |
MURAI H, KODAMA T, MAESAKA K, et al. Multiomics identifies the link between intratumor steatosis and the exhausted tumor immune microenvironment in hepatocellular carcinoma[J]. Hepatology, 2023, 77( 1): 77- 91. DOI: 10.1002/hep.32573. |
| [2] |
LI BH, LI YZ, ZHOU HJ, et al. Multiomics identifies metabolic subtypes based on fatty acid degradation allocating personalized treatment in hepatocellular carcinoma[J]. Hepatology, 2024, 79( 2): 289- 306. DOI: 10.1097/HEP.0000000000000553. |
| [3] |
SANKAR K, GONG J, OSIPOV A, et al. Recent advances in the management of hepatocellular carcinoma[J]. Clin Mol Hepatol, 2024, 30( 1): 1- 15. DOI: 10.3350/cmh.2023.0125. |
| [4] |
HILL A, OLUMBA F, CHAPMAN W. Transplantation for hepatocellular carcinoma[J]. Surg Clin North Am, 2024, 104( 1): 103- 111. DOI: 10.1016/j.suc.2023.09.002. |
| [5] |
YILMA M, MEHTA N. Optimal liver transplantation criteria for hepatocellular carcinoma[J]. Surg Oncol Clin N Am, 2024, 33( 1): 133- 142. DOI: 10.1016/j.soc.2023.06.011. |
| [6] |
TRAN NH, MUÑOZ S, THOMPSON S, et al. Hepatocellular carcinoma downstaging for liver transplantation in the era of systemic combined therapy with anti-VEGF/TKI and immunotherapy[J]. Hepatology, 2022, 76( 4): 1203- 1218. DOI: 10.1002/hep.32613. |
| [7] |
KARDASHIAN A, FLORMAN SS, HAYDEL B, et al. Liver transplantation outcomes in a U.S. multicenter cohort of 789 patients with hepatocellular carcinoma presenting beyond Milan criteria[J]. Hepatology, 2020, 72( 6): 2014- 2028. DOI: 10.1002/hep.31210. |
| [8] |
IVANICS T, CLAASEN MPAW, SAMSTEIN B, et al. Living donor liver transplantation for hepatocellular carcinoma within and outside traditional selection criteria: A multicentric North American experience[J]. Ann Surg, 2024, 279( 1): 104- 111. DOI: 10.1097/SLA.0000000000006049. |
| [9] |
CHOI J, JO C, LIM YS. Tenofovir versus entecavir on recurrence of hepatitis B virus-related hepatocellular carcinoma after surgical resection[J]. Hepatology, 2021, 73( 2): 661- 673. DOI: 10.1002/hep.31289. |
| [10] |
ZHU P, LIAO W, ZHANG WG, et al. A prospective study using propensity score matching to compare long-term survival outcomes after robotic-assisted, laparoscopic, or open liver resection for patients with BCLC stage 0-a hepatocellular carcinoma[J]. Ann Surg, 2023, 277( 1): e103- e111. DOI: 10.1097/SLA.0000000000005380. |
| [11] |
RASIC G, de GEUS SWL, BEAULIEU-JONES B, et al. A nationwide propensity score analysis comparing ablation and resection for hepatocellular carcinoma[J]. J Surg Oncol, 2023, 127( 7): 1125- 1134. DOI: 10.1002/jso.27232. |
| [12] |
XU JB, QI FZ, XU G, et al. Adjuvant interferon therapy after surgical treatment for hepatitis B/C virus-related hepatocellular carcinoma: A meta-analysis[J]. Hepatol Res, 2014, 44( 2): 209- 217. DOI: 10.1111/hepr.12109. |
| [13] |
YANG S, LIN Q, LIN W, et al. Effect of adjuvant interferon therapy on hepatitis B virus-related hepatocellular carcinoma: A systematic review[J]. World J Surg Oncol, 2016, 14( 1): 159. DOI: 10.1186/s12957-016-0912-7. |
| [14] |
ADWAN H, HAMMANN L, VOGL TJ. Microwave ablation of recurrent hepatocellular carcinoma after curative surgical resection[J]. J Clin Med, 2023, 12( 7): 2560. DOI: 10.3390/jcm12072560. |
| [15] |
RYU T, TAKAMI Y, WADA Y, et al. Combined hepatectomy and microwave ablation for multifocal hepatocellular carcinoma: Long-term outcomes and prognostic factors[J]. Asian J Surg, 2021, 44( 1): 186- 191. DOI: 10.1016/j.asjsur.2020.05.008. |
| [16] |
WANG Z, LIU M, ZHANG DZ, et al. Microwave ablation versus laparoscopic resection as first-line therapy for solitary 3-5-cm HCC[J]. Hepatology, 2022, 76( 1): 66- 77. DOI: 10.1002/hep.32323. |
| [17] |
WICKS JS, DALE BS, RUFFOLO L, et al. Comparable and complimentary modalities for treatment of small-sized HCC: Surgical resection, radiofrequency ablation, and microwave ablation[J]. J Clin Med, 2023, 12( 15): 5006. DOI: 10.3390/jcm12155006. |
| [18] |
LIU KW, ZHENG H, SUI XZ, et al. Microwave ablation versus surgical resection for subcapsular hepatocellular carcinoma: A propensity score-matched study of long-term therapeutic outcomes[J]. Eur Radiol, 2023, 33( 3): 1938- 1948. DOI: 10.1007/s00330-022-09135-1. |
| [19] |
DING WZ, YU J, LIU FY, et al. Percutaneous microwave ablation versus robot-assisted hepatectomy for early hepatocellular carcinoma: A real-world single-center study[J]. Dig Liver Dis, 2022, 54( 2): 243- 250. DOI: 10.1016/j.dld.2021.04.008. |
| [20] |
TONG Y, CAI R, LI JX, et al. Liver resection versus microwave ablation for hepatocellular carcinoma in ideal candidates for ablation per Barcelona Clinic Liver Cancer staging: A propensity score matching and inverse probability of treatment weighting analysis[J]. Aliment Pharmacol Ther, 2022, 56( 11-12): 1602- 1614. DOI: 10.1111/apt.17263. |
| [21] |
WANG WQ, LV X, LI J, et al. Repeat hepatectomy versus microwave ablation for solitary and small(≤3 cm) recurrent hepatocellular carcinoma with early or late recurrence: A propensity score matched study[J]. Eur J Surg Oncol, 2023, 49( 5): 1001- 1008. DOI: 10.1016/j.ejso.2022.12.016. |
| [22] |
LIN YZ, SHI HY, MU XH. Diagnosis of small primary liver cancer under the background of liver cirrhosis by dual-source CT hepatic artery three-phase scanning and enhanced perfusion scanning[J]. J Pract Hepatol, 2023, 26( 3): 412- 415. DOI: 10.3969/j.issn.1672-5069.2023.03.028. |
| [23] |
|
| [24] |
ZHANG QB, ZHANG XG, JIANG RD, et al. Microwave ablation versus hepatic resection for the treatment of hepatocellular carcinoma and oesophageal variceal bleeding in cirrhotic patients[J]. Int J Hyperthermia, 2017, 33( 3): 255- 262. DOI: 10.1080/02656736.2016.1257824. |
| [25] |
ZHANG EL, YANG F, WU ZB, et al. Therapeutic efficacy of percutaneous microwave coagulation versus liver resection for single hepatocellular carcinoma ≤3 cm with Child-Pugh A cirrhosis[J]. Eur J Surg Oncol, 2016, 42( 5): 690- 697. DOI: 10.1016/j.ejso.2016.02.251. |
| [26] |
YANG F, ZHANG EL, XIAO ZY, et al. Therapeutic outcomes of surgical resection versus percutaneous microwave coagulation therapy for single small hepatocellular carcinoma with cirrhosis(250 cases)[J]. Acta Med Univ Sci Technol Huazhong, 2016, 45( 2): 185- 189. DOI: 10.3870/j.issn.1672-0741.2016.02.014. |
| [27] |
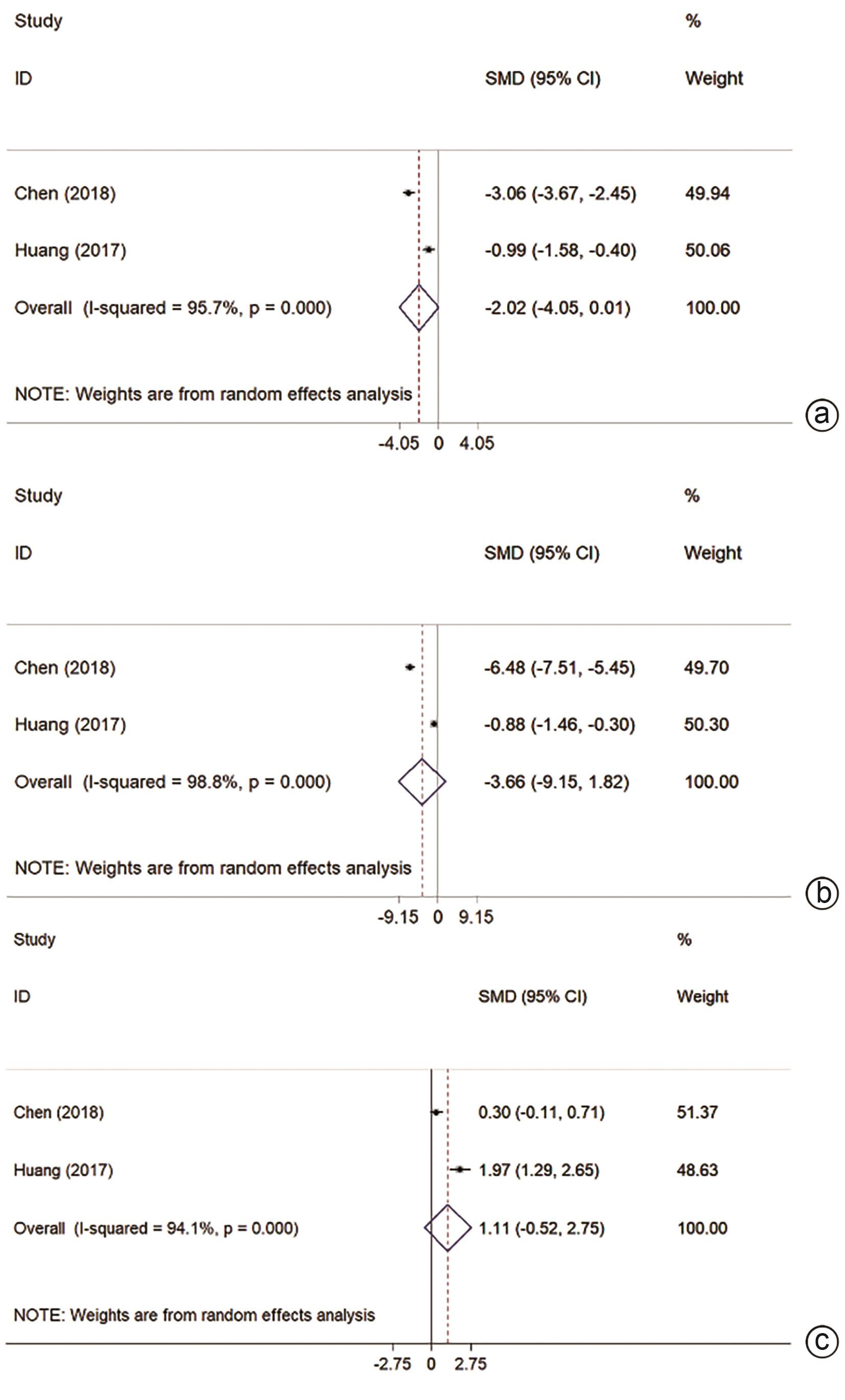
HUANG Y, CHEN J, LIU XS. Clinical efficacy of laparoscopic microwave ablation in the treatment of small hepatocellular carcinoma with cirrhosis[J]. Chin J Minim Invasive Surg, 2017, 17( 6): 504- 508. DOI: 10.3969/j.issn.1009-6604.2017.06.008. |
| [28] |
LIAO LF, XUE JZ, LI SK. Survival analysis of percutan eous microwave ablation for patients with small hepatocellular carcinoma with underlying liver cirrhosis[J]. J Pract Hepatol, 2018, 21( 2): 257- 260. DOI: 10.3969/j.issn.1672-5069.2018.02.025. |
| [29] |
CHEN HJ, CHEN Y, ZHANG SQ, et al. Comparison of microwave ablation and surgical resection in the treatment of 92 cases of small hepatocellular carcinoma complicated with cirrhosis[J]. Med J Commun, 2018, 32( 2): 163- 165.
陈红健, 陈橼, 张素青, 等. 微波消融与手术切除治疗小肝癌合并肝硬化92例效果比较[J]. 交通医学, 2018, 32( 2): 163- 165.
|
| [30] |
WANG HP, JIA J. Comparative analysis of microwave ablation and surgical resection in the treatment of 90 cases of small hepatocellular carcinoma complicated with cirrhosis[J/CD]. Electron J Clin Med Lit, 2019, 6( 94): 52. DOI: 10.16281/j.cnki.jocml.2019.94.043. |
| [31] |
HUANG ZM, ZHU CH, LI J. Clinical observation of microwave ablation and surgical resection in the treatment of small hepatocellular carcinoma with resectable cirrhosis[J]. Shenzhen J Integr Tradit Chin West Med, 2016, 26( 23): 16- 18, 199. DOI: 10.16458/j.cnki.1007-0893.2016.23.008. |
| [32] |
|
| [33] |
|
| [34] |
General Office of National Health Commission. Standard for diagnosis and treatment of primary liver cancer(2022 edition)[J]. J Clin Hepatol, 2022, 38( 2): 288- 303. DOI: 10.3969/j.issn.1001-5256.2022.02.009. |
| [35] |
XIONG K, ZHU LP, LU Y, et al. Network Meta-analysis on the efficacy and safety of surgical resection and thermal ablations for hepatocellular carcinoma in China[J]. Chin J Hepatobiliary Surg, 2019, 25( 11): 823- 827. DOI: 10.3760/cma.j.issn.1007-8118.2019.11.007. |
| [36] |
ZHANG T, HU H, JIA YS, et al. Efficacy and safety of radiofrequency ablation and surgery for hepatocellular carcinoma in patients with cirrhosis: A meta-analysis[J]. Medicine, 2022, 101( 52): e32470. DOI: 10.1097/MD.0000000000032470. |
| [37] |
WANG WX, ZHANG FZ, XU XX, et al. Comparison on efficacy of TACE combined with radiofrequency ablation or microwave ablation for primary hepatocellular carcinoma: Meta-analysis[J]. Chin J Interv Imag Ther, 2023, 20( 8): 467- 472. DOI: 10.13929/j.issn.1672-8475.2023.08.005. |








 DownLoad:
DownLoad: