| [1] |
Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Gastroenterology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. Consensus on the diagnosis and therapy of hepatic fibrosis(2019)[J]. J Clin Hepatol, 2019, 35( 10): 2163- 2172. DOI: 10.3969/j.issn.1001-5256.2019.10.007. |
| [2] |
|
| [3] |
BEDOSSA P, DARGÈRE D, PARADIS V. Sampling variability of liver fibrosis in chronic hepatitis C[J]. Hepatology, 2003, 38( 6): 1449- 1457. DOI: 10.1053/jhep.2003.09022. |
| [4] |
|
| [5] |
LI ZC, HUANG Y, ZHANG ZY, et al. Analysis of prediction indicators and prediction model construction for severity of liver fibrosis[J]. Chin J Gen Surg, 2020, 29( 11): 1364- 1369. DOI: 10.7659/j.issn.1005-6947.2020.11.010. |
| [6] |
DONG SQ, MA QZ, WU CN, et al. Imaging quality of biliary tract and detecting diseases with hepatobiliary phase Gd-EOB-DTPA contrast-enhanced MR cholangiography based on 3D-VIBE and 3D-FLASH sequences[J]. Chin J Med Imag Technol, 2023, 39( 6): 866- 871. DOI: 10.13929/j.issn.1003-3289.2023.06.015. |
| [7] |
DU WT, REN WL, HU DD, et al. Research progress on reversible animal model of liver fibrosis[J/OL]. Chin J Liver Dis Electron Version, 2022, 14( 3): 18- 21. DOI: 10.3969/j.issn.1674-7380.2022.03.005. |
| [8] |
DEWIDAR B, MEYER C, DOOLEY S, et al. TGF-β in hepatic stellate cell activation and liver fibrogenesis-updated 2019[J]. Cells, 2019, 8( 11): 1419. DOI: 10.3390/cells8111419. |
| [9] |
LIU JH, LI XY, WANG ML, et al. Advantages and characteristics of traditional Chinese medicine in the treatment of liver fibrosis[J]. J Clin Hepatol, 2023, 39( 2): 267- 272. DOI: 10.3969/j.issn.1001-5256.2023.02.003. |
| [10] |
LU LG, YOU H, XIE WF, et al. Consensus on the diagnosis and therapy of hepatic fibrosis[J]. J Pract Hepatol, 2019, 22( 6): 793- 803.
陆伦根, 尤红, 谢渭芬, 等. 肝纤维化诊断及治疗共识(2019年)[J]. 实用肝脏病杂志, 2019, 22( 6): 793- 803.
|
| [11] |
SUN YM, CHEN SY, YOU H. Regression of liver fibrosis: Evidence and challenges[J]. Chin Med J, 2020, 133( 14): 1696- 1702. DOI: 10.1097/CM9.0000000000000835. |
| [12] |
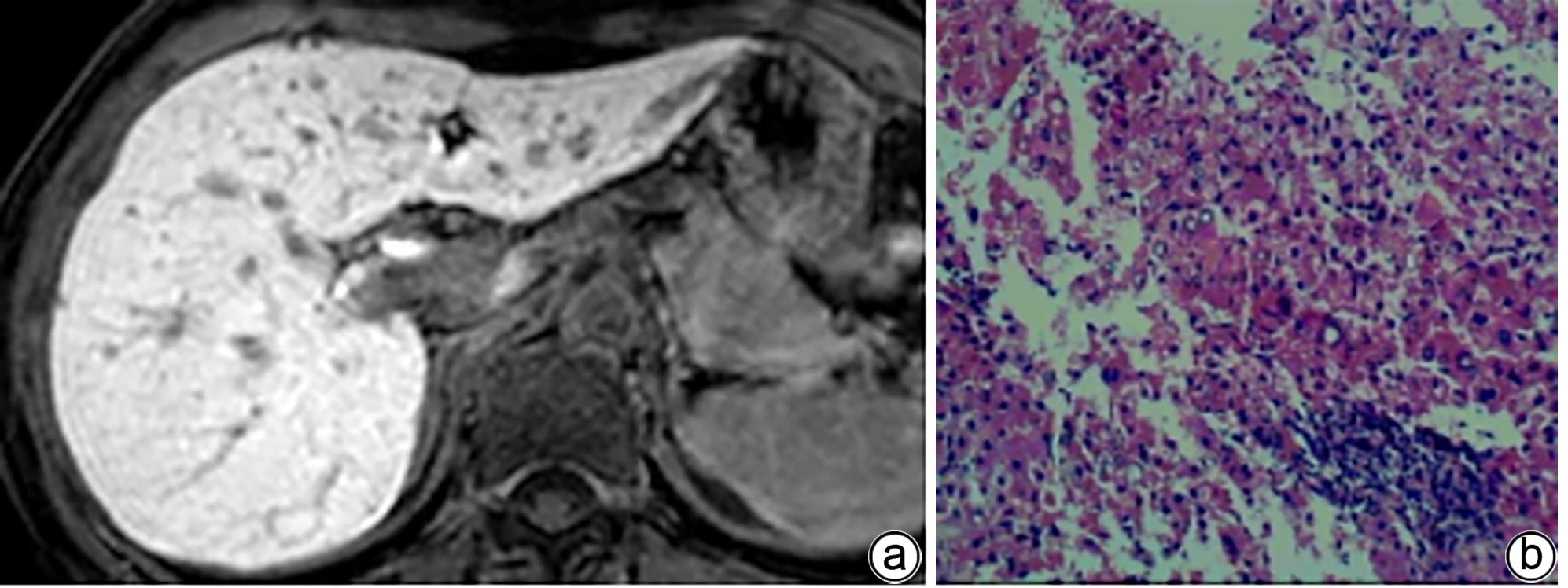
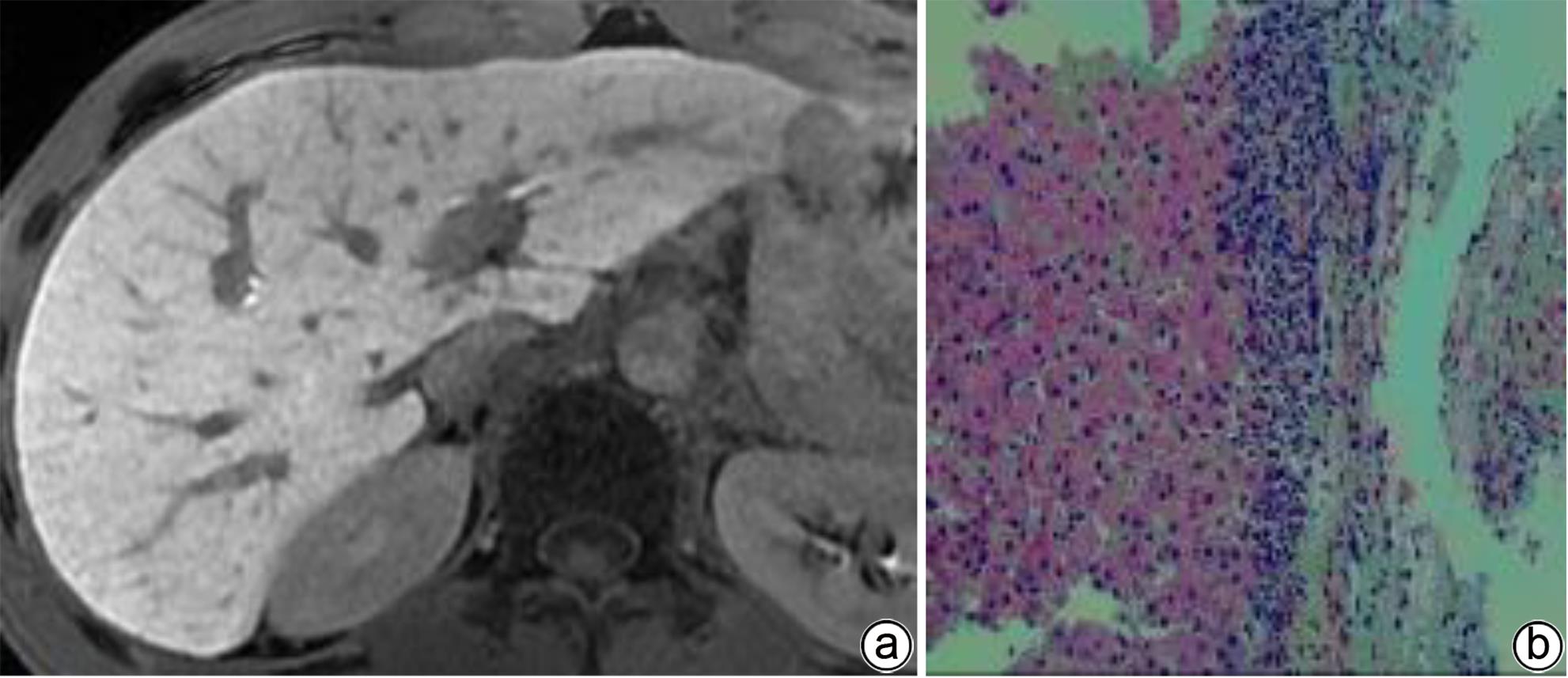
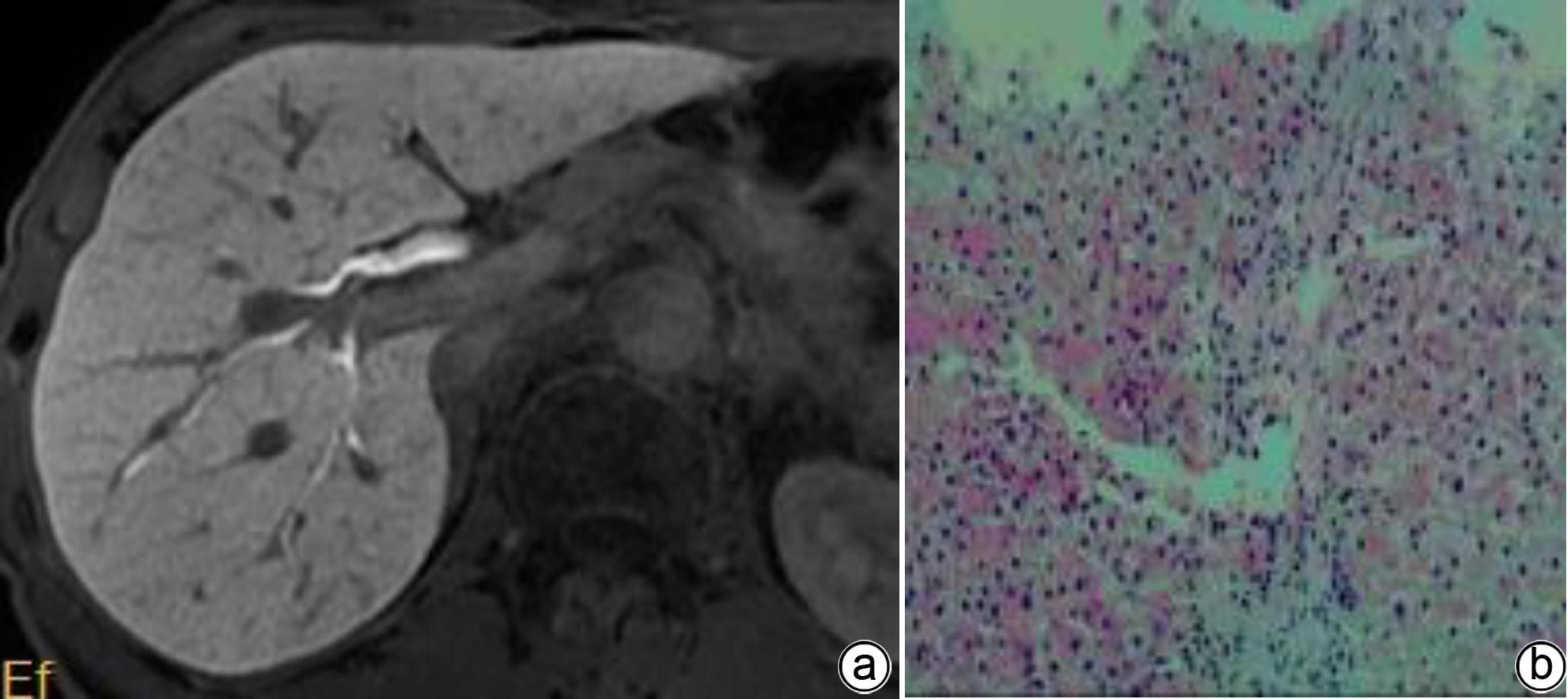
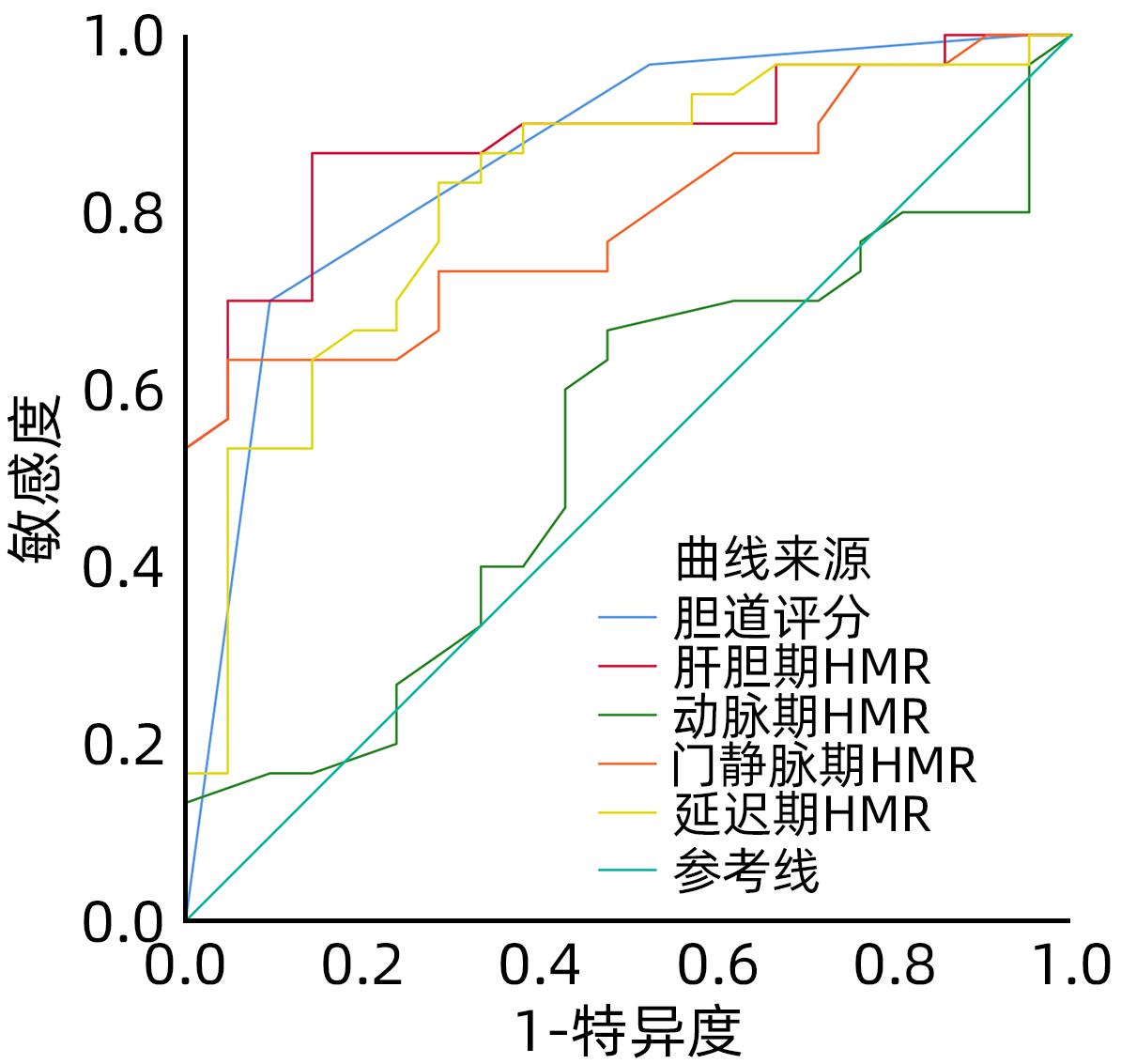
TONG HF, WANG ZH, CHEN H, et al. Prediction of the histological grades of liver fibrosis and cirrhosis by quantitative analysis of gadoxetic acid contrast-enhanced MRI[J]. J Wenzhou Med Univ, 2020, 50( 9): 717- 722. DOI: 10.3969/j.issn.2095-9400.2020.09.006. |
| [13] |
JIANG Y, SHU J, LU X, et al. A preliminary study for the quantitative assessment of chronic hepatitis by dynamic contrast-enhanced magnetic resonance imaging[J]. J Clin Radiol, 2019, 38( 7): 1324- 1329. DOI: 10.13437/j.cnki.jcr.20190731.014. |
| [14] |
ZHANG JY, LU J, ZHANG XQ, et al. Feasibility and repeatability of Gd-EOB-DTPA enhanced MRI in evaluating hepatic function[J]. J Nantong Univ Med Sci, 2021, 41( 6): 534- 538. DOI: 10.16424/j.cnki.cn32-1807/r.2021.06.013. |
| [15] |
WANG AR, WANG Q. The Current status of gadolinium disodium enhanced MRI in quantitative assessment of liver function[J]. Chin J Oncol Prev Treat, 2021, 13( 1): 94- 99. DOI: 10.3969/j.issn.1674-5671.2021.01.18. |
| [16] |
Foundation for Hepatitis Prevention and Control; Chinese Society of Infectious Disease and Chinese Society of Hepatology, Chinese Medical Association. Consensus on clinical application of transient elastography detecting liver fibrosis: A 2018 update[J]. Chin J Hepatol, 2019, 27( 3): 182- 191. DOI: 10.3760/cma.j.issn.1007-3418.2019.03.004. |
| [17] |
IMAJO K, KESSOKU T, HONDA Y, et al. Magnetic resonance imaging more accurately classifies steatosis and fibrosis in patients with nonalcoholic fatty liver disease than transient elastography[J]. Gastroenterology, 2016, 150( 3): 626- 637.e7. DOI: 10.1053/j.gastro.2015.11.048. |
| [18] |
LIU YR, WANG M, ZENG G, et al. Diagnostic efficacy of significant liver fibrosis by apparent diffusion coefficient in patients with primary sclerosing cholangitis[J]. J Pract Hepatol, 2021, 24( 3): 375- 378. DOI: 10.3969/j.issn.1672-5069.2021.03.018. |







 DownLoad:
DownLoad: