线粒体功能障碍在肝纤维化发病中的作用机制
DOI: 10.12449/JCH260124
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:洪雨蝶负责设计论文框架,撰写论文;郭锦晨负责拟定写作思路;施卫兵指导撰写文章并定稿;孙宇洁负责起草文章大纲;王佳敏负责整理机制图思路;高甜甜负责审阅文章。
Research advances in mitochondrial dysfunction in the pathogenesis of hepatic fibrosis
-
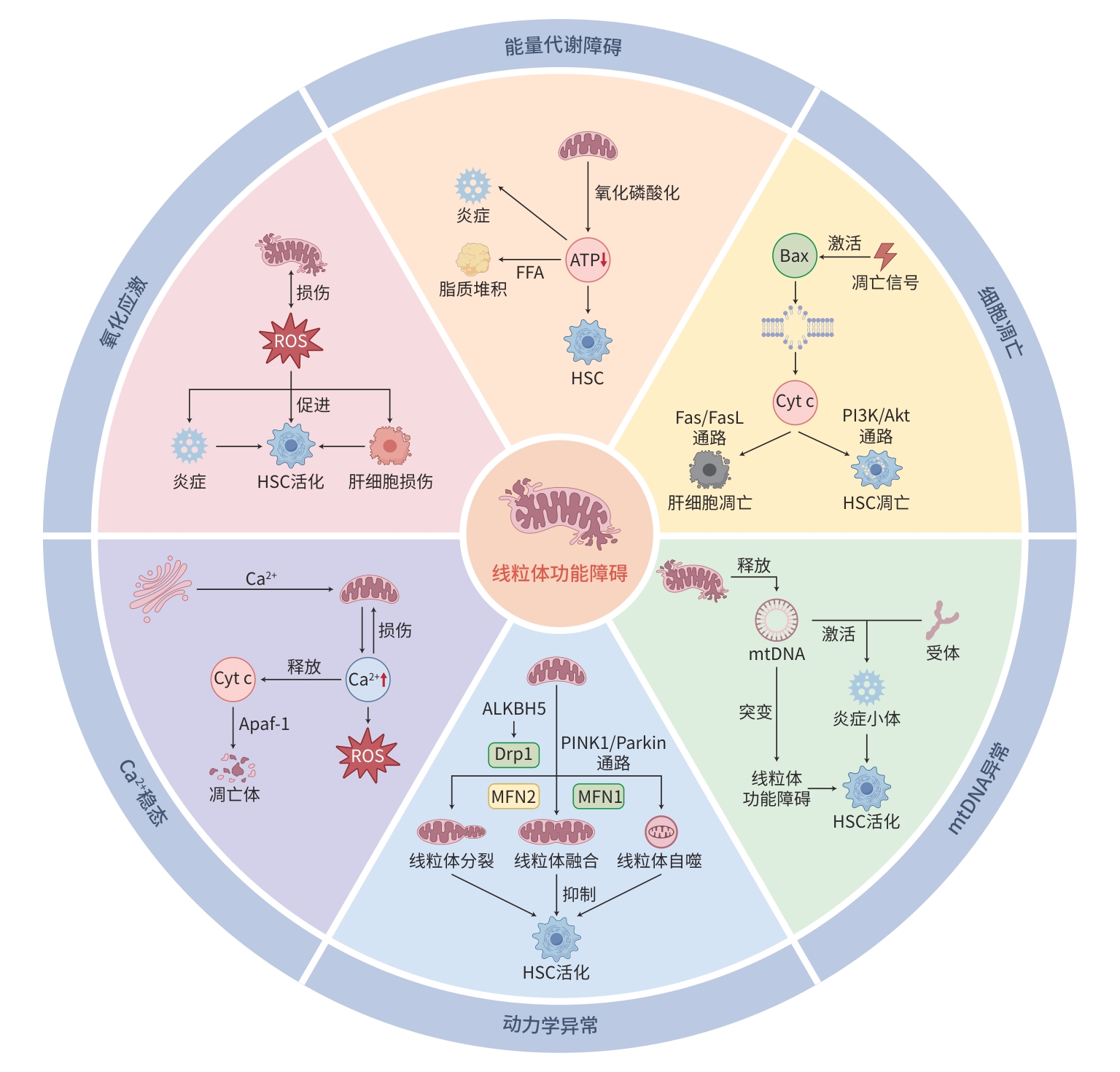
摘要: 肝纤维化是在多种致病因素的影响下,肝内纤维结缔组织过度堆积并异常增生,可进展为肝硬化、门静脉高压及肝癌。其病理机制涉及肝细胞损伤、炎症细胞浸润与炎症介质释放、肝星状细胞活化以及细胞外基质堆积等。近年研究关注线粒体功能障碍在该疾病发展,包括代谢紊乱与能量不足、氧化应激、线粒体动态失衡、自噬功能改变等机制驱动肝纤维化的分子通路,这些均能引起肝损伤。本文综述了线粒体功能障碍在肝纤维化发病机制中的最新进展,可为临床治疗提供新治疗策略。Abstract: Hepatic fibrosis refers to excessive accumulation and abnormal proliferation of fibrous connective tissue in the liver triggered by multiple pathogenic factors, and it may progress to liver cirrhosis, portal hypertension, and liver cancer. The pathological mechanisms of hepatic fibrosis involve hepatocyte injury, inflammatory cell infiltration with the release of inflammatory mediators, hepatic stellate cell activation, and extracellular matrix deposition. Recent studies have focused on mitochondrial dysfunction in disease progression, including the molecular pathways for hepatic fibrosis driven by metabolic disorders, energy deficiency, oxidative stress, mitochondrial dynamic imbalance, and autophagic dysfunction, all of which can induce liver injury. This article reviews the latest advances in hepatic fibrosis, in order to provide new therapeutic strategies for clinical management.
-
Key words:
- Hepatic Fibrosis /
- Mitochondria /
- Pathologic Processes
-
[1] WU XN, XUE F, ZHANG N, et al. Global burden of liver cirrhosis and other chronic liver diseases caused by specific etiologies from 1990 to 2019[J]. BMC Public Health, 2024, 24( 1): 363. DOI: 10.1186/s12889-024-17948-6. [2] UDOMSINPRASERT W, SOBHONSLIDSUK A, JITTIKOON J, et al. Cellular senescence in liver fibrosis: Implications for age-related chronic liver diseases[J]. Expert Opin Ther Targets, 2021, 25( 9): 799- 813. DOI: 10.1080/14728222.2021.1992385. [3] SU R, FU HL, ZHANG QX, et al. Amplifying hepatic L-aspartate levels suppresses CCl(4)-induced liver fibrosis by reversing glucocorticoid receptor β-mediated mitochondrial malfunction[J]. Pharmacol Res, 2024, 206: 107294. DOI: 10.1016/j.phrs.2024.107294. [4] THOMPSON B, BATES E. Surprise finding reveals mitochondrial‘energy factories’ come in two different types[J]. Nature, 2024. DOI: 10.1038/d41586-024-03646-1.[ Epub ahead of print] [5] NESTEROV S, CHESNOKOV Y, KAMYSHINSKY R, et al. Ordered clusters of the complete oxidative phosphorylation system in cardiac mitochondria[J]. Int J Mol Sci, 2021, 22( 3): 1462. DOI: 10.3390/ijms22031462. [6] WILHELMSEN I, COMBRIAT T, DALMAO-FERNANDEZ A, et al. The effects of TGF-β-induced activation and starvation of vitamin A and palmitic acid on human stem cell-derived hepatic stellate cells[J]. Stem Cell Res Ther, 2024, 15( 1): 223. DOI: 10.1186/s13287-024-03852-8. [7] NGUYEN G, PARK SY, DO DV, et al. Gemigliptin alleviates succinate-induced hepatic stellate cell activation by ameliorating mitochondrial dysfunction[J]. Endocrinol Metab, 2022, 37( 6): 918- 928. DOI: 10.3803/EnM.2022.1530. [8] KORY N, WYANT GA, PRAKASH G, et al. SFXN1 is a mitochondrial serine transporter required for one-carbon metabolism[J]. Science, 2018, 362( 6416): eaat9528. DOI: 10.1126/science.aat9528. [9] RUAN XX, LIAO XM, DENG ZJ, et al. Experimental study of translocase of inner mitochondrial membrane 13 regulating the activation and proliferation of hepatic stellate cells[J]. J Guangxi Med Univ, 2023, 40( 5): 756- 761. DOI: 10.16190/j.cnki.45-1211/r.2023.05.007.阮仙仙, 廖晓敏, 邓哲君, 等. 线粒体内膜转位酶13调控肝星状细胞活化和增殖的实验研究[J]. 广西医科大学学报, 2023, 40( 5): 756- 761. DOI: 10.16190/j.cnki.45-1211/r.2023.05.007. [10] BAE M, KIM MB, LEE JY. Fucoxanthin attenuates the reprogramming of energy metabolism during the activation of hepatic stellate cells[J]. Nutrients, 2022, 14( 9): 1902. DOI: 10.3390/nu14091902. [11] LI F, LIU X, BAI N, et al. Irisin attenuates liver fibrosis by regulating energy metabolism and HMGB1/β-catenin signaling in hepatic stellate cells[J]. Eur J Pharmacol, 2025, 998: 177519. DOI: 10.1016/j.ejphar.2025.177519. [12] MU CY, WANG SJ, WANG ZH, et al. Mechanisms and therapeutic targets of mitochondria in the progression of metabolic dysfunction-associated steatotic liver disease[J]. Ann Hepatol, 2025, 30( 1): 101774. DOI: 10.1016/j.aohep.2024.101774. [13] DENG YY, ZHANG Z, YANG H, et al. Mycophenolic acid induces the intestinal epithelial barrier damage through mitochondrial ROS[J]. Oxid Med Cell Longev, 2022, 2022: 4195699. DOI: 10.1155/2022/4195699. [14] SHARMA S, ZHANG XM, AZHAR G, et al. Valine improves mitochondrial function and protects against oxidative stress[J]. Biosci Biotechnol Biochem, 2024, 88( 2): 168- 176. DOI: 10.1093/bbb/zbad169. [15] LUO SF, YANG B, XU HL, et al. Lithospermic acid improves liver fibrosis through Piezo1-mediated oxidative stress and inflammation[J]. Phytomedicine, 2024, 134: 155974. DOI: 10.1016/j.phy med.2024.155974. [16] PING DB, QI JS, SUN X, et al. Protective effect of all-trans retinoic acid on natural killer cells damaged by oxidative stress in liver fibrosis[J]. Chin J Immunol, 2024, 40( 7): 1359- 1363. DOI: 10.3969/j.issn.1000-484X.2024.07.003.平大冰, 齐婧姝, 孙鑫, 等. 全反式维甲酸对肝纤维化氧化应激损伤自然杀伤细胞的保护作用[J]. 中国免疫学杂志, 2024, 40( 7): 1359- 1363. DOI: 10.3969/j.issn.1000-484X.2024.07.003. [17] WANG T, ZHOU X, KUANG G, et al. Paeoniflorin modulates oxidative stress, inflammation and hepatic stellate cells activation to alleviate CCl4-induced hepatic fibrosis by upregulation of heme oxygenase-1 in mice[J]. J Pharm Pharmacol, 2021, 73( 3): 338- 346. DOI: 10.1093/jpp/rgaa042. [18] ZHANG LZ, ZHANG YH, CHANG XX, et al. Imbalance in mitochondrial dynamics induced by low PGC-1α expression contributes to hepatocyte EMT and liver fibrosis[J]. Cell Death Dis, 2020, 11( 4): 226. DOI: 10.1038/s41419-020-2429-9. [19] MORCILLO P, CORDERO H, IJOMONE OM, et al. Defective mitochondrial dynamics underlie manganese-induced neurotoxicity[J]. Mol Neurobiol, 2021, 58( 7): 3270- 3289. DOI: 10.1007/s12035-021-02341-w. [20] CASTRO-SEPULVEDA M, FERNÁNDEZ-VERDEJO R, ZBINDEN-FONCEA H, et al. Mitochondria-SR interaction and mitochondrial fusion/fission in the regulation of skeletal muscle metabolism[J]. Metabolism, 2023, 144: 155578. DOI: 10.1016/j.metabol.2023.155578. [21] CHEN P, YUAN MQ, YAO LC, et al. Human umbilical cord-derived mesenchymal stem cells ameliorate liver fibrosis by improving mitochondrial function via Slc25a47-Sirt3 signaling pathway[J]. Biomed Pharmacother, 2024, 171: 116133. DOI: 10.1016/j.biopha.2024.116133. [22] JIA L, YANG Y, SUN F, et al. Mitochondrial quality control in liver fibrosis: Epigenetic hallmarks and therapeutic strategies[J]. Cell Signal, 2024, 115: 111035. DOI: 10.1016/j.cellsig.2024.111035. [23] GHANI M, SZABÓ B, ALKHATIBE M, et al. Serine 39 in the GTP-binding domain of Drp1 is involved in shaping mitochondrial morphology[J]. FEBS Open Bio, 2024, 14( 7): 1147- 1165. DOI: 10.1002/2211-5463.13820. [24] ZHOU H, ZHU P, WANG J, et al. DNA-PKcs promotes alcohol-related liver disease by activating Drp1-related mitochondrial fission and repressing FUNDC1-required mitophagy[J]. Signal Transduct Targ Ther, 2019, 4( 1): 12. DOI: 10.1038/s41392-019-0094-1. [25] WANG J, YANG Y, SUN F, et al. ALKBH5 attenuates mitochondrial fission and ameliorates liver fibrosis by reducing Drp1 methylation[J]. Pharmacol Res, 2023, 187: 106608. DOI: 10.1016/j.phrs.2022.106608. [26] LI LF, YU J, LI R, et al. Apoptosis, mitochondrial autophagy, fission, and fusion maintain mitochondrial homeostasis in mouse liver under tail suspension conditions[J]. Int J Mol Sci, 2024, 25( 20): 11196. DOI: 10.3390/ijms252011196. [27] KUNLAYAWUTIPONG T, APAIJAI N, TEPMALAI K, et al. Imbalance of mitochondrial fusion in peripheral blood mononuclear cells is associated with liver fibrosis in patients with metabolic dysfunction-associated steatohepatitis[J]. Heliyon, 2024, 10( 6): e27557. DOI: 10.1016/j.heliyon.2024.e27557. [28] YE HT, CAI TW, SHEN Y, et al. MST1 knockdown inhibits osteoarthritis progression through Parkin-mediated mitophagy and Nrf2/NF-κB signalling pathway[J]. J Cell Mol Med, 2024, 28( 11): e18476. DOI: 10.1111/jcmm.18476. [29] LI PP, LI S, WANG L, et al. Mitochondrial dysfunction in hearing loss: Oxidative stress, autophagy and NLRP3 inflammasome[J]. Front Cell Dev Biol, 2023, 11: 1119773. DOI: 10.3389/fcell.2023.1119773. [30] WU Y. Research on metformin improving liver fibrosis caused by schistosomiasis through regulating mitophagy[D]. Wuhan: Huazhong University of Science and Technology, 2020.吴悠. 二甲双胍通过调节线粒体自噬而改善血吸虫病肝纤维化的研究[D]. 武汉: 华中科技大学, 2020. [31] DOU SD, ZHANG JN, XIE XL, et al. MitoQ inhibits hepatic stellate cell activation and liver fibrosis by enhancing PINK1/parkin-mediated mitophagy[J]. Open Med, 2021, 16( 1): 1718- 1727. DOI: 10.1515/med-2021-0394. [32] WANG ZJ, YU H, HAO JJ, et al. PM2.5 promotes Drp1-mediated mitophagy to induce hepatic stellate cell activation and hepatic fibrosis via regulating miR-411[J]. Exp Cell Res, 2021, 407( 2): 112828. DOI: 10.1016/j.yexcr.2021.112828. [33] AN ZX, HE YL, WANG F, et al. Effects of fupi Rougan recipe and its disassembled recipes on expression of mitochondrial autophagy-related proteins in liver tissue of rats with hepatic fibrosis[J]. Chin Arch Tradit Chin Med, 2022, 40( 2): 11- 15, insert back 15- 18. DOI: 10.13193/j.issn.1673-7717.2022.02.003.安祯祥, 何远利, 王芳, 等. 扶脾柔肝方及拆方对肝纤维化大鼠肝组织线粒体自噬相关蛋白表达的影响[J]. 中华中医药学刊, 2022, 40( 2): 11- 15, 后插15-后插 18. DOI: 10.13193/j.issn.1673-7717.2022.02.003. [34] ZHANG WF. Exploring the role and mechanism of mitochondrial autophagy in the inhibition of liver fibrosis by Rigid Liver Fibrosis Granules through the miR-135a/FOXO1/PINK1 pathway[D]. Nanning: Guangxi University of Chinese Medicine, 2024.张文富. 基于miR-135a/FOXO1/PINK1通路探讨线粒体自噬在柔肝化纤颗粒抑制肝纤维化中的作用及机制[D]. 南宁: 广西中医药大学, 2024. [35] HUANG YG, YU FL. Effects of melatonin on mitochondrial autophagy in rats with hepatic fibrosis induced by carbon tetrachloride[J]. Chin J Clin Pharmacol, 2019, 35( 11): 1149- 1152. DOI: 10.13699/j.cnki.1001-6821.2019.11.016.黄宜贵, 余方流. 褪黑素对四氯化碳诱导的肝纤维化大鼠线粒体自噬的影响[J]. 中国临床药理学杂志, 2019, 35( 11): 1149- 1152. DOI: 10.13699/j.cnki.1001-6821.2019.11.016. [36] WEISER A, HERMANT A, BERMONT F, et al. The mitochondrial calcium uniporter(MCU) activates mitochondrial respiration and enhances mobility by regulating mitochondrial redox state[J]. Redox Biol, 2023, 64: 102759. DOI: 10.1016/j.redox.2023.102759. [37] JIANG C, SHEN J, WANG C, et al. Mechanism of aconitine mediated neuronal apoptosis induced by mitochondrial calcium overload caused by MCU[J]. Toxicol Lett, 2023, 384: 86- 95. DOI: 10.1016/j.toxlet.2023.07.014. [38] WALKON LL, STRUBBE-RIVERA JO, BAZIL JN. Calcium overload and mitochondrial metabolism[J]. Biomolecules, 2022, 12( 12): 1891. DOI: 10.3390/biom12121891. [39] LI SW, MA Y, YE SZ, et al. Polystyrene microplastics trigger hepatocyte apoptosis and abnormal glycolytic flux via ROS-driven calcium overload[J]. J Hazard Mater, 2021, 417: 126025. DOI: 10.1016/j.jhazmat.2021.126025. [40] SALAZAR-RAMÍREZ F, BERNAL-RAMIREZ J, LUEVANO LA, et al. Increased oxidative stress mediated by catecholamine-induced mitochondrial calcium overload leads to mitochondrial and cellular dysfunction which ultimately promotes arrhythmia generation[J]. J Am Coll Cardiol, 2023, 81( 8): 300. DOI: 10.1016/S0735-1097(23)00744-1. [41] YU YF, BAI LN, JIAO JW, et al. Research progress in traditional Chinese medicine in the prevention and treatment of non-alcoholic steatohepatitis based on mitochondrial regulation mechanism[J]. J Changchun Univ Chin Med, 2025, 41( 4): 456- 460. DOI: 10.13463/j.cnki.cczyy.2025.04.022.于云飞, 白洛宁, 焦靖雯, 等. 基于线粒体调控机制对中药防治NASH的研究进展[J]. 长春中医药大学学报, 2025, 41( 4): 456- 460. DOI: 10.13463/j.cnki.cczyy.2025.04.022. [42] PAN S, WANG B, YU M, et al. Hydrogen alleviates myocardial infarction by impeding apoptosis via ROS-mediated mitochondrial endogenous pathway[J]. Free Radic Res, 2025, 59( 3): 226- 238. DOI: 10.1080/10715762.2025.2474014. [43] ZHAO JN, PENG JH, LIU P, et al. Effect of Cordyceps polysaccharides on hepatocyte apoptosis induced by tumor necrosis factor-α[J]. J Clin Hepatol, 2021, 37( 6): 1368- 1372. DOI: 10.3969/j.issn.1001-5256.2021.06.029.赵佳男, 彭景华, 刘平, 等. 虫草多糖对肿瘤坏死因子α诱导肝细胞凋亡的影响[J]. 临床肝胆病杂志, 2021, 37( 6): 1368- 1372. DOI: 10.3969/j.issn.1001-5256.2021.06.029. [44] SUKHAMWANG A, INTHANON S, DEJKRIENGKRAIKUL P, et al. Anti-cancer potential of isoflavone-enriched fraction from traditional Thai fermented soybean against hela cervical cancer cells[J]. Int J Mol Sci, 2024, 25( 17): 9277. DOI: 10.3390/ijms25179277. [45] SU Y, LU S, HOU CJ, et al. Mitigation of liver fibrosis via hepatic stellate cells mitochondrial apoptosis induced by metformin[J]. Int Immunopharmacol, 2022, 108: 108683. DOI: 10.1016/j.intimp.2022.108683. [46] SONG JH, LV HN, LIU BB, et al. Let-7 suppresses liver fibrosis by inhibiting hepatocyte apoptosis and TGF-β production[J]. Mol Metab, 2023, 78: 101828. DOI: 10.1016/j.molmet.2023.101828. [47] WU SX, CHEN WN, JING ZT, et al. Hepatitis B spliced protein(HBSP) suppresses fas-mediated hepatocyte apoptosis via activation of PI3K/Akt signaling[J]. J Virol, 2018, 92( 23): e01273-18. DOI: 10.1128/JVI.01273-18. [48] JIANG MJ, HUANG CM, WU Q, et al. Sini San ameliorates CCl4-induced liver fibrosis in mice by inhibiting AKT-mediated hepatocyte apoptosis[J]. J Ethnopharmacol, 2023, 303: 115965. DOI: 10.1016/j.jep.2022.115965. [49] LEE SW, KIM SM, HUR W, et al. Tenofovir disoproxil fumarate directly ameliorates liver fibrosis by inducing hepatic stellate cell apoptosis via downregulation of PI3K/Akt/mTOR signaling pathway[J]. PLoS One, 2021, 16( 12): e0261067. DOI: 10.1371/journal.pone.0261067. [50] WANG J, CHU ES, LAN HY, et al. 207 microRNA-29b prevents liver fibrosis by attenuating hepatic stellate cell activation and inducing apoptosis in vitro and in mice[J]. Gastroenterology, 2013, 144( 5): S-938. DOI: 10.1016/S0016-5085(13)63488-5. [51] LIU MK, YE JH, YANG F, et al. Based on the Sam50-MICOS-ATAD3-mtDNA axis: Exploring oligomeric proanthocyanidins to alleviate molybdenum and cadmium co-induced liver inflammation in sheep[J]. Int J Biol Macromol, 2025, 304( Pt 2): 141035. DOI: 10.1016/j.ijbiomac.2025.141035. [52] de GAETANO A, SOLODKA K, ZANINI G, et al. Molecular mechanisms of mtDNA-mediated inflammation[J]. Cells, 2021, 10( 11): 2898. DOI: 10.3390/cells10112898. [53] ZHENG YM, XIE YD, LI JY, et al. CMPK2 promotes NLRP3 inflammasome activation via mtDNA-STING pathway in house dust mite-induced allergic rhinitis[J]. Clin Transl Med, 2025, 15( 1): e70180. DOI: 10.1002/ctm2.70180. [54] ZHAO Y, WANG ZC, FENG DC, et al. p66Shc contributes to liver fibrosis through the regulation of mitochondrial reactive oxygen species[J]. Theranostics, 2019, 9( 5): 1510- 1522. DOI: 10.7150/thno.29620. [55] ZHU KX, LIU L, ZHANG XH, et al. The relationship between mitochondria DNA mutation and alcoholic liver damage in rats[J]. J Toxicol, 2008, 22( 2): 114- 116. DOI: 10.16421/j.cnki.1002-3127.2008.02.027.朱孔锡, 刘莉, 张喜红, 等. 线粒体DNA突变与大鼠乙醇性肝纤维化的关系[J]. 毒理学杂志, 2008, 22( 2): 114- 116. DOI: 10.16421/j.cnki.1002-3127.2008.02.027. -



 PDF下载 ( 855 KB)
PDF下载 ( 855 KB)

 下载:
下载:


