基于临床特征构建肝硬化食管胃底静脉曲张再出血的新型预测模型
DOI: 10.12449/JCH260112
Establishment of a new predictive model for esophagogastric variceal rebleeding in liver cirrhosis based on clinical features
-
摘要:
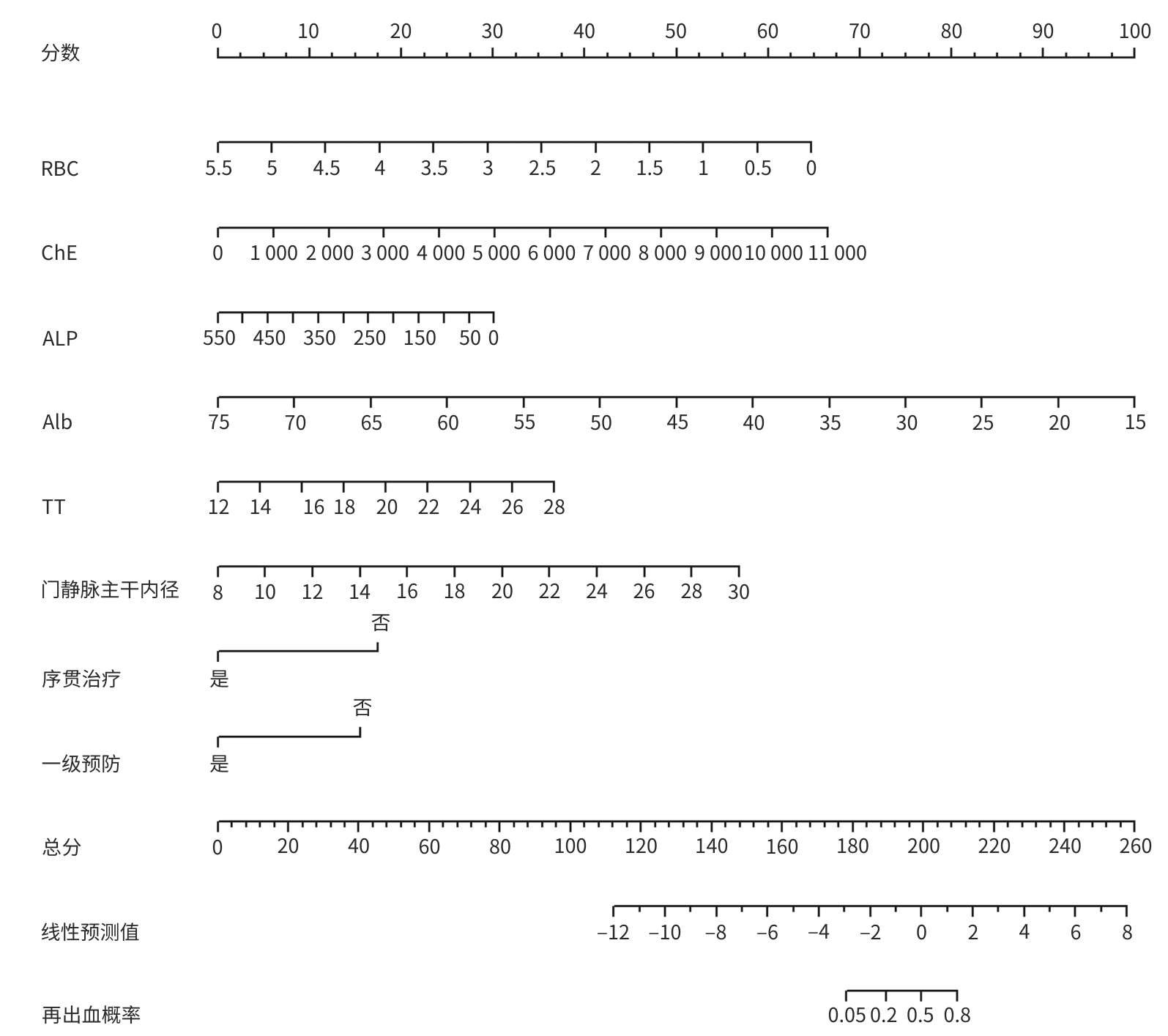
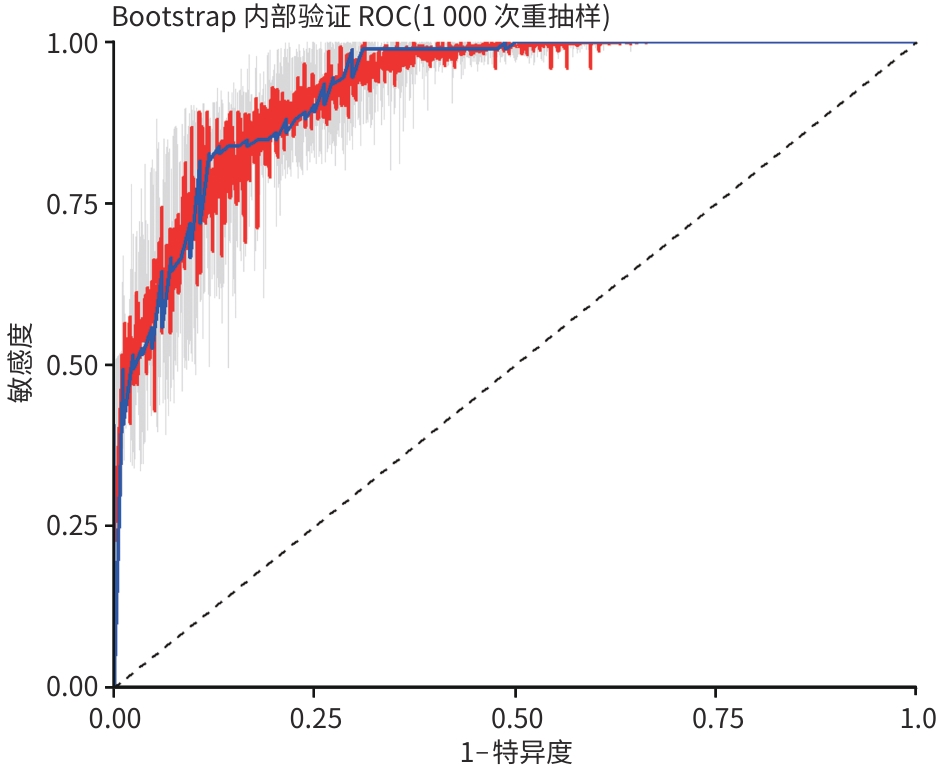
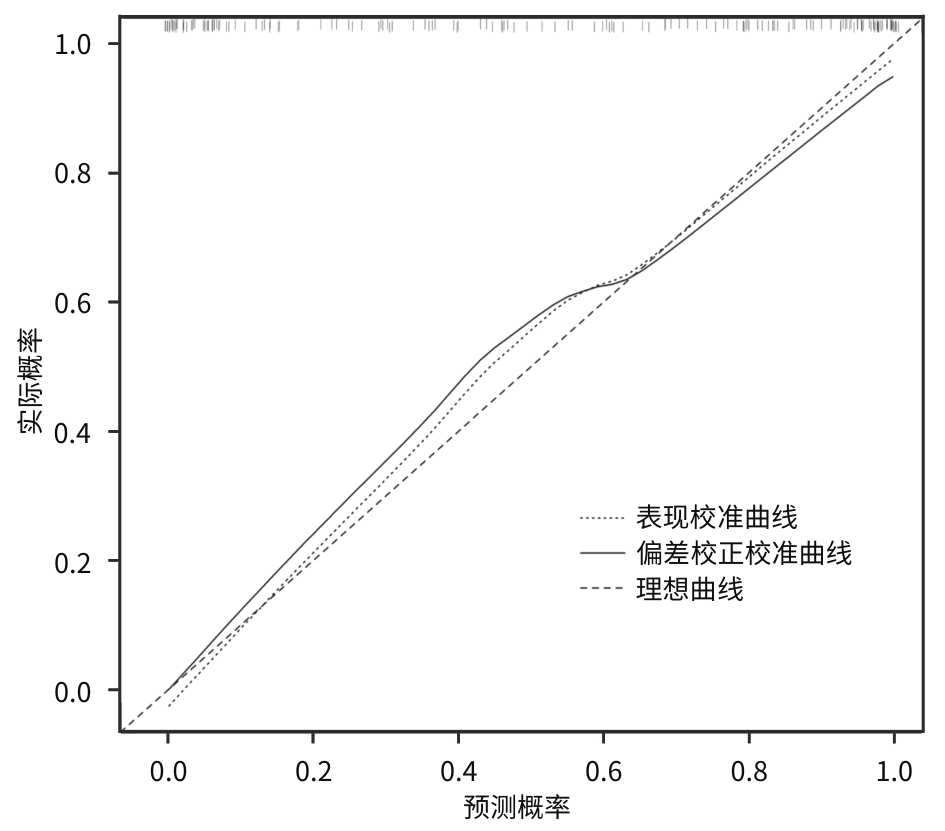
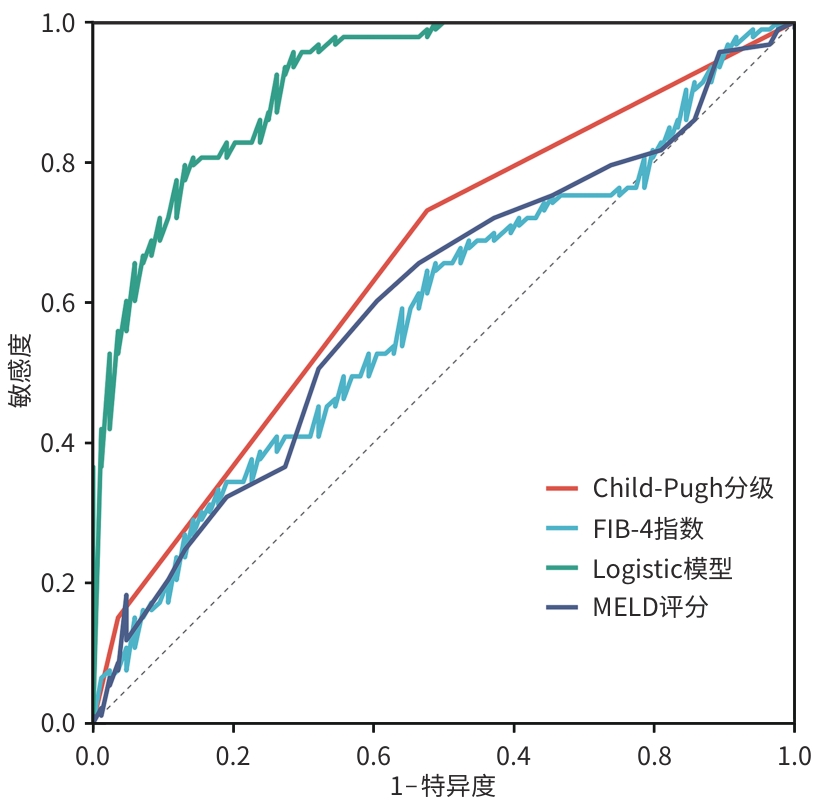
目的 通过筛选肝硬化食管胃底静脉曲张(EGVB)出血患者内镜治疗后再出血的独立预测因素,构建一种无创、简单且易行的新型临床预测模型,以期为个体化风险评估和临床干预策略制订提供依据。 方法 选取2018年9月—2023年10月在西安医学院第一附属医院诊治的肝硬化EGVB患者为研究对象,根据患者在内镜治疗后1年内是否再出血分为再出血组(n=93)和未再出血组(n=84),并收集患者相关临床资料。符合正态分布的计量资料两组间比较采用成组t检验;非正态分布的计量资料两组间比较采用Mann-Whitney U检验;计数资料两组间比较采用χ2检验。通过单因素、多因素分析结果构建Logistic模型,采用受试者操作特征曲线(ROC曲线)评价模型的准确性,利用R软件绘制列线图使模型可视化,应用Bootstrap法对模型进行内部验证。 结果 多因素分析结果显示,红细胞(RBC)、胆碱酯酶(ChE)、碱性磷酸酶(ALP)、白蛋白(Alb)、凝血酶时间(TT)、门静脉主干内径、序贯治疗和一级预防是再出血的独立预测因素。根据多因素分析结果构建Logistic模型为:logit(P)=-0.805-1.978(RBC)+0.001(ChE)-0.020(ALP)-0.314(Alb)+0.567(TT)+0.428(门静脉主干内径)-2.303[序贯治疗(是=1,否=0)]-2.368[一级预防(是=1,否=0)]。Logistic模型[曲线下面积(AUC)=0.928,P<0.001,95%置信区间(CI):0.893~0.964]在预测再出血方面优于终末期肝病模型评分(AUC=0.603,P=0.003,95%CI:0.520~0.687)、蔡尔德-皮尤分级(Child-Pugh分级)(AUC=0.650,P=0.001,95%CI:0.578~0.722)和肝纤维化4因子指数(AUC=0.587,P=0.045,95%CI:0.503~0.671)。其最佳截断值为0.607,敏感度为0.817,特异度为0.817。在内部验证中,模型仍具有很好的预测能力及准确性。 结论 实施序贯治疗、实施一级预防、RBC水平升高、Alb水平升高是再出血的保护因素,TT延长和门静脉主干内径增宽是危险因素,基于上述独立预测因素构建的Logistic模型可以对再出血进行预测,值得进一步应用于临床。 -
关键词:
- 肝硬化 /
- 食管和胃静脉曲张 /
- 胃肠出血 /
- Logistic模型
Abstract:Objective To establish a new noninvasive, simple, and convenient clinical predictive model by identifying independent predictive factors for rebleeding after endoscopic therapy in cirrhotic patients with esophagogastric variceal bleeding (EGVB), and to provide a basis for individualized risk assessment and development of clinical intervention strategies. Methods Cirrhotic patients with EGVB who were diagnosed and treated in The First Affiliated Hospital of Xi’an Medical University from September 2018 to October 2023 were enrolled as subjects, and according to whether the patient experienced rebleeding within 1 year after endoscopic therapy, they were divided into rebleeding group with 93 patients and non-rebleeding group with 84 patients. Clinical data were collected and analyzed. The independent samples t-test was used for comparison of normally distributed continuous data between two groups, and the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups; the chi-square test was used for comparison of categorical data between two groups. A Logistic model was established based on the results of the univariate and multivariate analyses, and the receiver operating characteristic (ROC) curve and the area under the ROC curve (AUC) were used to assess the accuracy of the model. R software was used to visualize the model by plotting a nomogram, and the Bootstrap method was used for internal validation of the model. Results The multivariate analysis showed that red blood cell count (RBC), cholinesterase (ChE), alkaline phosphatase (ALP), albumin (Alb), thrombin time (TT), portal vein trunk diameter, sequential therapy, and primary prevention were independent predictive factors for rebleeding. Based on the results of the multivariate analysis, a logistic model was established as logit(P)=-0.805-1.978×(RBC)+0.001×(ChE)-0.020×(ALP)-0.314×(Alb)+0.567×(TT)+0.428×(portal vein trunk diameter)-2.303×[sequential therapy (yes=1, no=0)]-2.368×[primary prevention (yes=1, no=0)]. The logistic model (AUC=0.928, 95% confidence interval [CI]: 0.893—0.964, P<0.001) had a better performance in predicting rebleeding than MELD score (AUC=0.603, 95%CI: 0.520—0.687, P=0.003), Child-Pugh class (AUC=0.650, 95%CI: 0.578—0.722, P=0.001), and FIB-4 index (AUC=0.587, 95%CI: 0.503—0.671, P=0.045). The model had an optimal cut-off value of 0.607, a sensitivity of 0.817, and a specificity of 0.817. Internal validation confirmed that the model had good predictive performance and accuracy. Conclusion Sequential therapy, implementation of primary prevention, an increase in RBC, and an increase in Alb are protective factors against rebleeding, while prolonged TT and widened main portal vein diameter are risk factors. The logistic model based on these independent predictive factors can predict rebleeding and thus holds promise for clinical application. -
表 1 未再出血组与再出血组基线特征比较
Table 1. Comparison of basic data between the non-rebleeding group and the rebleeding group
指标 未再出血组
(n=84)再出血组
(n=93)统计值 P值 年龄(岁) 55.73±12.90 57.99±13.02 t=-1.160 0.248 男[例(%)] 49(58.3) 58(62.4) χ2=0.300 0.584 吸烟[例(%)] 16(19.0) 23(24.7) χ2=0.830 0.362 饮酒[例(%)] 16(19.0) 18(19.4) χ2=0.003 0.959 病因[例(%)] χ2=0.096 0.992 乙型肝炎 58(69.0) 66(71.0) 丙型肝炎 13(15.5) 14(15.1) 酒精性肝炎 5(6.0) 5(5.4) 其他 8(9.5) 8(9.5) 表 2 未再出血组与再出血组并发症情况比较
Table 2. Comparison of complications between the non-rebleeding group and the rebleeding group
指标 未再出血组
(n=84)再出血组
(n=93)χ2值 P值 HE[例(%)] 2.949 0.248 无 84(100) 89(95.7) 1~2级 0(0.0) 2(2.2) 3~4级 0(0.0) 2(2.2) 腹水[例(%)] 5.137 0.120 无 54(64.3) 47(50.5) 少量 28(33.3) 38(40.9) 中量 2(2.4) 7(7.5) 大量 0(0.0) 1(1.1) PHG[例(%)] 2.013 0.156 无 38(45.2) 52(55.9) 有 46(54.8) 41(44.1) PVT[例(%)] 5.923 0.052 无 74(88.1) 69(74.2) 主干栓子 9(10.7) 20(21.5) 分支栓子 1(1.2) 4(4.3) 注:HE,肝性脑病;PHG,门静脉高压性胃病;PVT,门静脉血栓形成。
表 3 未再出血组与再出血组实验室指标比较
Table 3. Comparison of laboratory indicators between the non-rebleeding group and the rebleeding group
指标 未再出血组(n=84) 再出血组(n=93) 统计值 P值 WBC(×109/L) 3.175(2.185~4.618) 4.140(2.845~6.675) Z=-3.834 <0.001 中性粒细胞(×109/L) 1.745(1.213~2.600) 2.900(1.815~4.585) Z=-5.229 <0.001 淋巴细胞(×109/L) 0.755(0.543~1.225) 0.800(0.485~1.125) Z=-0.505 0.613 单核细胞(×109/L) 0.285(0.203~0.463) 0.340(0.235~0.585) Z=-1.593 0.111 RBC(×1012/L) 3.690(3.265~4.132) 2.790(2.460~3.160) Z=-6.307 <0.001 HGB(g/L) 102.50(84.00~122.75) 80.00(70.50~95.00) Z=-5.034 <0.001 PLT(×109/L) 70.5(54.0~97.0) 66.0(49.0~84.0) Z=-1.416 0.157 TBil(μmol/L) 21.19(15.25~29.30) 25.90(15.64~41.80) Z=-2.020 0.043 ChE(U/L) 4 216.81±1 392.30 3 560.54±1 542.97 t=-2.959 0.004 AST(U/L) 31.00(25.25~41.75) 31.00(22.00~42.00) Z=-0.579 0.563 ALT(U/L) 21.50(15.25~36.00) 21.00(14.00~38.50) Z=-0.651 0.516 AST/ALT 1.435(1.183~1.705) 1.470(1.205~1.900) Z=-1.075 0.282 ALP(U/L) 100.50(74.25~134.50) 78.00(62.00~107.00) Z=-3.454 0.001 GGT(U/L) 33.00(20.00~58.50) 28.00(20.00~47.00) Z=-0.692 0.489 Alb(g/L) 34.300(31.325~37.775) 29.700(25.600~34.050) Z=-5.365 <0.001 Cr(μmol/L) 57.450(48.025~71.350) 60.200(49.000~73.450) Z=-0.805 0.421 尿酸(μmol/L) 309.00(248.25~383.75) 284.00(237.00~350.00) Z=-1.165 0.244 PT(s) 18.888±2.998 20.582±3.574 t=-3.396 0.001 INR 1.424±0.258 1.570±0.330 t=-3.271 0.001 APTT(s) 35.170±4.393 32.643±5.709 t=3.275 0.001 TT(s) 17.261±1.842 18.605±2.334 t=-4.223 <0.001 D-D(mg/L) 0.680(0.315~1.955) 1.080(0.395~2.565) Z=-1.506 0.132 血氨(μmol/L) 50.210(37.085~64.423) 54.840(41.090~77.360) Z=-2.277 0.023 MELD评分(分) 6.62±4.84 8.95±5.51 t=-2.971 0.003 Child-Pugh分级[例(%)] χ2=15.107 0.001 A级 44(52.4) 25(36.9) B级 37(44.0) 54(58.1) C级 3(3.6) 14(15.1) FIB-4指数 5.177(3.852~7.325) 6.099(4.072~9.314) Z=-2.006 0.045 注:WBC,白细胞;RBC,红细胞;HGB,血红蛋白;PLT,血小板;TBil,总胆红素;ChE,胆碱酯酶;AST,天冬氨酸氨基转移酶;ALT,丙氨酸氨基转移酶;ALP,碱性磷酸酶;GGT,γ-谷氨酰转移酶;Alb,白蛋白;Cr,肌酐;PT,凝血酶原时间;INR,国际标准化比值;APTT,活化部分凝血活酶时间;TT,凝血酶时间;D-D,D-二聚体;MELD,终末期肝病模型;Child-Pugh分级,蔡尔德-皮尤分级;FIB-4,肝纤维化4因子指数。
表 4 未再出血组与再出血组影像学及胃镜指标比较
Table 4. Comparison of imaging and gastroscopic indexes between the non-rebleeding group and the rebleeding group
指标 未再出血组(n=84) 再出血组(n=93) 统计值 P值 门静脉主干内径(mm) 15.00(12.00~17.00) 17.00(15.00~19.00) Z=-4.191 <0.001 L[例(%)] χ2=10.417 0.183 Lei 2(2.4) 0(0.0) Lei,gf 2(2.4) 2(2.2) Lei,gf Lgf 0(0.0) 1(1.1) Lemi 4(4.8) 0(0.0) Lemi,gf 57(67.9) 67(72.0) Lemi,gf Lgf 11(13.1) 7(7.5) Lemi,Lgf 3(3.6) 5(5.4) Lesmi,gf 1(1.2) 2(2.2) Lgf 4(4.8) 9(9.7) D[例(%)] χ2=15.373 0.004 D0.5 0(0.0) 1(1.1) D1.0 43(51.2) 25(25.9) D1.5 15(17.9) 17(18.3) D2.0 23(27.4) 46(49.5) D2.5 2(2.4) 1(1.1) D3.0 0(0.0) 2(2.2) D4.0 1(1.2) 1(1.1) Rf[例(%)] χ2 =12.404 0.001 Rf0 28(33.3) 16(17.2) Rf1 56(66.7) 69(74.2) Rf2 0(0.0) 8(8.6) 红色征[例(%)] χ2=4.396 0.036 阴性 30(35.7) 20(21.5) 阳性 54(64.3) 73(78.5) 马赛克样改变[例(%)] χ2=1.980 0.159 阴性 83(98.8) 87(93.5) 阳性 1(1.2) 6(6.5) 胃黏膜花斑样改变[例(%)] χ2=0.303 0.582 阴性 21(25.0) 20(21.5) 阳性 63(75.0) 73(78.5) 组织胶用量(mL) 1.5(0.5~2.0) 2.5(1.5~3.0) Z=-4.880 <0.001 聚桂醇用量(mL) 26(19~36) 26(20~40) Z=-1.348 0.178 治疗方式[例(%)] χ2=0.808 0.668 组织胶硬化治疗术 60(71.4) 64(68.8) 套扎治疗术 2(2.4) 1(1.1) 组织胶硬化治疗术+套扎 22(26.2) 28(30.1) 序贯治疗[例(%)] χ2=17.950 <0.001 是 50(59.5) 26(28.0) 否 34(40.5) 67(72.0) 一级预防[例(%)] χ2=25.439 <0.001 是 47(56.0) 18(19.4) 否 37(44.0) 75(80.6) 注:L,曲张静脉位置;Lei,食管下段静脉曲张;Lei,gf,食管下段静脉曲张延伸至胃底;Lei,gf Lgf,食管下段静脉曲张延伸至胃底,伴孤立性胃底静脉曲张;Lemi,食管中下段静脉曲张;Lemi,gf,食管中下段静脉曲张延伸至胃底;Lemi,gf Lgf,食管中下段静脉曲张延伸至胃底,伴孤立性胃底静脉曲张;Lemi,Lgf,食管中下段静脉曲张,伴孤立性胃底静脉曲张;Lesmi,gf,食管上中下段静脉曲张延伸至胃底;Lgf,孤立性胃底静脉曲张;D,曲张静脉最大直径;D0.5,直径0.5 cm;D1.0,直径1.0 cm;D1.5,直径1.5 cm;D2.0,直径2.0 cm;D2.5,直径2.5 cm;D3.0,直径3.0 cm;D4.0直径4.0 cm;Rf:危险因素;Rf0,无近期出血指征;Rf1,有近期出血的征象,需要择期进行内镜下治疗;Rf2,可见糜烂、血栓头、活动性出血,需要及时进行内镜下治疗。
表 5 影响EGVB患者再出血的二元Logistic回归多因素分析
Table 5. Multivariate analysis of binary Logistic regression influencing rebleeding in patients with EGVB
变量 β值 SE Wald χ2 OR P值 95%CI RBC -1.978 0.901 4.819 0.138 0.028 0.024~0.809 ChE 0.001 0.000 3 7.373 1.001 0.007 1.000~1.002 ALP -0.020 0.008 6.735 0.981 0.009 0.966~0.995 Alb -0.314 0.128 6.011 0.730 0.014 0.568~0.939 TT 0.567 0.222 6.499 1.763 0.011 1.140~2.725 门静脉主干内径 0.428 0.117 13.416 1.534 <0.001 1.220~1.929 序贯治疗 -2.303 0.713 10.418 0.100 0.001 0.025~0.405 一级预防 -2.368 0.737 10.313 0.094 0.001 0.022~0.397 注:RBC,红细胞;ChE,胆碱酯酶;ALP,碱性磷酸酶;Alb,白蛋白;TT,凝血酶时间;OR,比值比;CI,置信区间。
表 6 ROC曲线分析结果
Table 6. The analysis of Roc curve
指标 AUC P值 95%CI Logistic模型 0.928 <0.001 0.893~0.964 MELD评分 0.603 0.003 0.520~0.687 Child-Pugh分级 0.650 0.001 0.578~0.722 FIB-4指数 0.587 0.045 0.503~0.671 注:MELD,终末期肝病模型;Child-Pugh分级,蔡尔德-皮尤分级;FIB-4,肝纤维化4因子指数;AUC,曲线下面积;CI,置信区间。
-
[1] ALQAHTANI SA, JANG S. Pathophysiology and management of variceal bleeding[J]. Drugs, 2021, 81( 6): 647- 667. DOI: 10.1007/s40265-021-01493-2. [2] BAIGES A, HERNÁNDEZ-GEA V. Management of liver decompensation in advanced chronic liver disease: Ascites, hyponatremia, and gastroesophageal variceal bleeding[J]. Clin Drug Investig, 2022, 42( Suppl 1): 25- 31. DOI: 10.1007/s40261-022-01147-5. [3] LESMANA CRA, RAHARJO M, GANI RA. Managing liver cirrhotic complications: Overview of esophageal and gastric varices[J]. Clin Mol Hepatol, 2020, 26( 4): 444- 460. DOI: 10.3350/cmh.2020.0022. [4] Chinese Society of Hepatology, Chinese Society of Gastroenterology, and Chinese Society of Digestive Endoscopology of Chinese Medical Association. Guidelines on the management of esophagogastric variceal bleeding in cirrhotic portal hypertension[J]. J Clin Hepatol, 2023, 39( 3): 527- 538. DOI: 10.3969/j.issn.1001-5256.2023.03.008.中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会内镜学分会. 肝硬化门静脉高压食管胃静脉曲张出血的防治指南[J]. 临床肝胆病杂志, 2023, 39( 3): 527- 538. DOI: 10.3969/j.issn.1001-5256.2023.03.008. [5] de FRANCHIS R, BOSCH J, GARCIA-TSAO G, et al. Baveno VII- Renewing consensus in portal hypertension[J]. J Hepatol, 2022, 76( 4): 959- 974. DOI: 10.1016/j.jhep.2021.12.022. [6] Chinese Society of Hepatology, Chinese Society of Gastroenterology, and Chinese Society of Digestive Endoscopology of Chinese Medical Association. Guidelines for the diagnosis and treatment of esophageal and gastric variceal bleeding in cirrhotic portal hypertension[J]. J Clin Hepatol, 2016, 32( 2): 203- 219. 10.3969/j.issn.1001-5256.2016.02.002. DOI: 10.3969/j.issn.1001-5256.2016.02.002中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会内镜学分会. 肝硬化门静脉高压食管胃静脉曲张出血的防治指南[J]. 临床肝胆病杂志, 2016, 32( 2): 203- 219. DOI: 10.3969/j.issn.1001-5256.2016.02.002. [7] Esophageal and Gastric Varices Group of the Digestive Endoscopy Society of the Chinese Medical Association. Tentative guidelines for endoscopic diagnosis and treatment of varicosity and variceal bleeding in digestive tract(2009)[J]. China Contin Med Educ, 2010, 2( 6): 21- 26. DOI: 10.3969/j.issn.1674-9308.2010.06.003.中华医学会消化内镜学分会食管胃静脉曲张学组. 消化道静脉曲张及出血的内镜诊断和治疗规范试行方案(2009年)[J]. 中国继续医学教育, 2010, 2( 6): 21- 26. DOI: 10.3969/j.issn.1674-9308.2010.06.003. [8] KIM WR, MANNALITHARA A, HEIMBACH JK, et al. MELD 3.0: The model for end-stage liver disease updated for the modern era[J]. Gastroenterology, 2021, 161( 6): 1887- 1895.e4. DOI: 10.1053/j.gastro.2021.08.050. [9] XIE X, LU LG. Advances in antiviral treatments of HBV-induced liver cirrhosis[J]. J Pract Hepatol, 2018, 21( 1): 140- 144. DOI: 10.3969/j.issn.1672-5069.2018.01.041.谢晓, 陆伦根. 乙型肝炎肝硬化抗病毒治疗的进展[J]. 实用肝脏病杂志, 2018, 21( 1): 140- 144. DOI: 10.3969/j.issn.1672-5069.2018.01.041. [10] Chinese Society of Infectious Diseases, Chinese Medical Association; Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B(version 2019)[J]. J Clin Hepatol, 2019, 35( 12): 2648- 2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007.中华医学会感染病学分会, 中华医学会肝病学分会. 慢性乙型肝炎防治指南(2019年版)[J]. 临床肝胆病杂志, 2019, 35( 12): 2648- 2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007. [11] WU XQ, TANG DJ, YANG PY, et al. Analysis of risk factors of hepatocellular carcinoma in patients with hepatitis B liver cirrhosis after antiviral treatment[J]. J Mod Oncol, 2020, 28( 24): 4295- 4299. DOI: 10.3969/j.issn.1672-4992.2020.24.018.吴晓庆, 唐德军, 杨璞叶, 等. 乙肝肝硬化患者抗病毒治疗后肝癌发生的危险因素分析[J]. 现代肿瘤医学, 2020, 28( 24): 4295- 4299. DOI: 10.3969/j.issn.1672-4992.2020.24.018. [12] ZHU SQ, ZHAO XA, WANG S. Influencing factors of liver cirrhosis complicated with esophageal and gastric variceal bleeding and values of three models in predicting rebleeding[J]. J Clin Med Pract, 2021, 25( 16): 49- 53. DOI: 10.7619/jcmp.20211353.朱思奇, 赵祥安, 王甦. 肝硬化伴食管胃底静脉曲张出血的影响因素及3种模型对再出血的预测价值[J]. 实用临床医药杂志, 2021, 25( 16): 49- 53. DOI: 10.7619/jcmp.20211353. [13] HOU YX, YU H, ZHANG Q, et al. Machine learning-based model for predicting the esophagogastric variceal bleeding risk in liver cirrhosis patients[J]. Diagn Pathol, 2023, 18( 1): 29. DOI: 10.1186/s13000-023-01293-0. [14] WANG SM, WANG N, YU Z, et al. Diagnostic values of APRI, AAR, and FIB-4 predictive models in autoimmune cirrhosis combined with esophagogastric fundal varices[J]. J Jilin Univ(Med Ed), 2024, 50( 2): 523- 528. DOI: 10.13481/j.1671-587X.20240227.王素梅, 王楠, 于珍, 等. APRI、AAR和FIB-4等预测模型对自身免疫性肝硬化伴食管胃底静脉曲张的诊断价值[J]. 吉林大学学报(医学版), 2024, 50( 2): 523- 528. DOI: 10.13481/j.1671-587X.20240227. [15] ZHENG JF, ZHANG YN, LI P, et al. The endoscopic ultrasound probe findings in prediction of esophageal variceal recurrence after endoscopic variceal eradication therapies in cirrhotic patients: A cohort prospective study[J]. BMC Gastroenterol, 2019, 19( 1): 32. DOI: 10.1186/s12876-019-0943-y. [16] ALVI H, ZUBERI BF, RASHEED T, et al. Evaluation of endoscopic variceal band ligation sessions in obliteration of esophageal varices[J]. Pak J Med Sci, 2020, 36( 2): 37- 41. DOI: 10.12669/pjms.36.2.1144. [17] GAO YY, YUAN HX, HAN T, et al. Associations between endoscopic primary prophylaxis and rebleeding in liver cirrhosis patients with esophagogastric variceal bleeding[J]. Front Surg, 2022, 9: 925915. DOI: 10.3389/fsurg.2022.925915. [18] VILLANUEVA C, COLOMO A, BOSCH A, et al. Transfusion strategies for acute upper gastrointestinal bleeding[J]. N Engl J Med, 2013, 368( 1): 11- 21. DOI: 10.1056/NEJMoa1211801. [19] CHEN YC, HSIAO CT, LIN LC, et al. The association between red blood cell transfusion and outcomes in patients with upper gastrointestinal bleeding[J]. Clin Transl Gastroenterol, 2018, 9( 3): 138. DOI: 10.1038/s41424-018-0004-9. [20] TIAN T. Application value of total bilirubin, Albumin, total bile acid and cholinesterase in the diagnosis of esophageal varices with cirrhosis[J]. Syst Med, 2024, 9( 10): 34- 37. DOI: 10.19368/j.cnki.2096-1782.2024.10.034.田甜. 总胆红素、白蛋白、总胆汁酸、胆碱酯酶检测在诊断肝硬化合并食管胃底静脉曲张中的应用价值[J]. 系统医学, 2024, 9( 10): 34- 37. DOI: 10.19368/j.cnki.2096-1782.2024.10.034. [21] WANG Z, XIE YW, LU Q, et al. The impact of Albumin infusion on the risk of rebleeding and in-hospital mortality in cirrhotic patients admitted for acute gastrointestinal bleeding: A retrospective study of a single institute[J]. BMC Gastroenterol, 2020, 20( 1): 198. DOI: 10.1186/s12876-020-01337-5. [22] VILLA E, BIANCHINI M, BLASI A, et al. EASL Clinical Practice Guidelines on prevention and management of bleeding and thrombosis in patients with cirrhosis[J]. J Hepatol, 2022, 76( 5): 1151- 1184. DOI: 10.1016/j.jhep.2021.09.003. [23] NORTHUP PG, CALDWELL SH. Coagulation in liver disease: A guide for the clinician[J]. Clin Gastroenterol Hepatol, 2013, 11( 9): 1064- 1074. DOI: 10.1016/j.cgh.2013.02.026. [24] BABA Y, KAWANO S, KONO Y, et al. Clinical characteristics and risk factors for rebleeding in patients with obscure gastrointestinal bleeding[J]. Intern Med, 2020, 59( 11): 1345- 1350. DOI: 10.2169/internalmedicine.3628-19. [25] WU C, ZHANG XL, XING YM, et al. Risk factors of re-bleeding after endoscopic esophageal Varix ligation in patients with hepatitis B liver cirrhosis and esophagogastric varices bleeding[J]. J Pract Hepatol, 2023, 26( 4): 540- 543. DOI: 10.3969/j.issn.1672-5069.2023.04.022.吴冲, 张小丽, 邢益门, 等. 内镜下套扎治疗乙型肝炎肝硬化并发食管胃静脉曲张破裂出血患者1年内再出血调查及危险因素分析[J]. 实用肝脏病杂志, 2023, 26( 4): 540- 543. DOI: 10.3969/j.issn.1672-5069.2023.04.022. [26] GIANNINI EG. Liver enzyme alteration: A guide for clinicians[J]. Can Med Assoc J, 2005, 172( 3): 367- 379. DOI: 10.1503/cmaj.1040752. [27] LI N. Application of AST and CHE expression levels for diagnosis of patients with liver cirrhosis during biochemical testing[J]. Smart Healthc, 2024, 10( 30): 32- 34. DOI: 10.19335/j.cnki.2096-1219.2024.30.009.李楠. 生化检验中AST、CHE水平表达在肝硬化患者诊断中的应用[J]. 智慧健康, 2024, 10( 30): 32- 34. DOI: 10.19335/j.cnki.2096-1219.2024.30.009. [28] BAI X, LIU XY, DU WJ, et al. Risk factors for bleeding events in patients with cirrhosis-associate esophageal and gastric varices[J]. Acta Univ Med Anhui, 2024, 59( 1): 149- 153. DOI: 10.19405/j.cnki.issn1000-1492.2024.01.024.白雪, 刘晓艳, 杜文军, 等. 肝硬化合并食管胃底静脉曲张患者发生破裂出血的危险因素分析[J]. 安徽医科大学学报, 2024, 59( 1): 149- 153. DOI: 10.19405/j.cnki.issn1000-1492.2024.01.024. [29] KOTHARI HG, GUPTA SJ, GAIKWAD NR, et al. Role of non-invasive markers in prediction of esophageal varices and variceal bleeding in patients of alcoholic liver cirrhosis from central India[J]. Turk J Gastroenterol, 2019, 30( 12): 1036- 1043. DOI: 10.5152/tjg.2019.18334. [30] GU D, TONG C, ZHAO XA, et al. Evaluation of PC/SD, FIB-4 index, CTP score, MELD score and MELD-Na score in the prediction of rebleeding after ligation of esophageal varices with cirrhosis in 1 year[J]. Chin J Gastroenterol Hepatol, 2023, 32( 3): 289- 294. DOI: 10.3969/j.issn.1006-5709.2023.03.010.顾达, 童聪, 赵祥安, 等. PC/SD、FIB-4指数、CTP评分、MELD评分、MELD-Na评分在预测肝硬化食管静脉曲张出血套扎术后1年内再出血的价值评估[J]. 胃肠病学和肝病学杂志, 2023, 32( 3): 289- 294. DOI: 10.3969/j.issn.1006-5709.2023.03.010. -



 PDF下载 ( 2141 KB)
PDF下载 ( 2141 KB)

 下载:
下载: