磁共振成像胆道评分和肝肌比值对肝占位患者术前肝储备功能的评估价值
DOI: 10.12449/JCH250920
Application value of preoperative assessment of liver reserve function based on magnetic resonance cholangiopancreatography-related parameters and liver-to-muscle ratio in patients with hepatic space-occupying lesion
-
摘要:
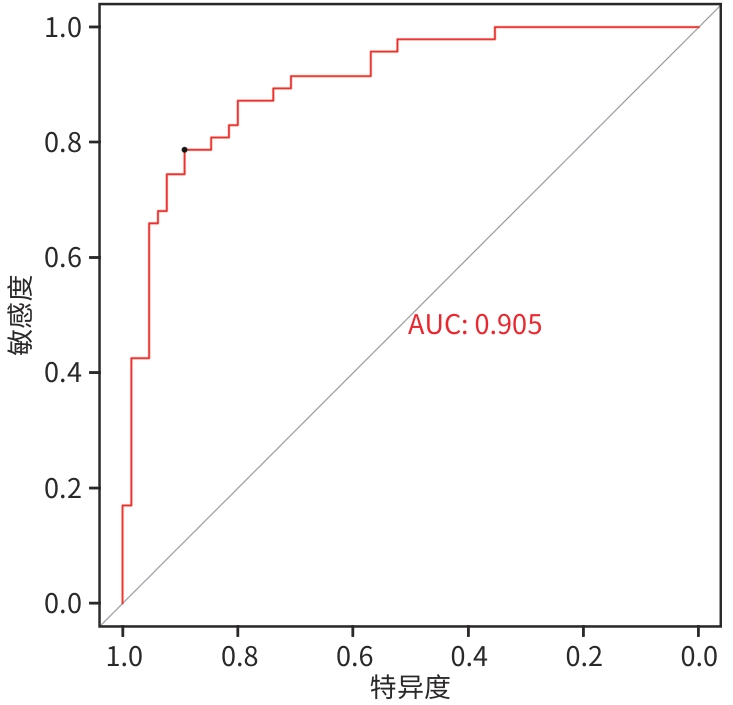
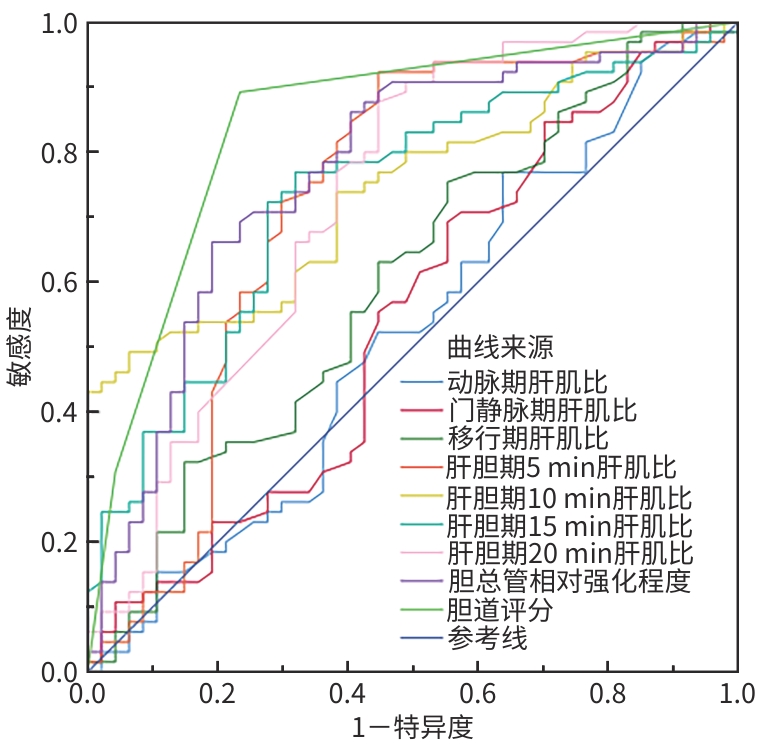
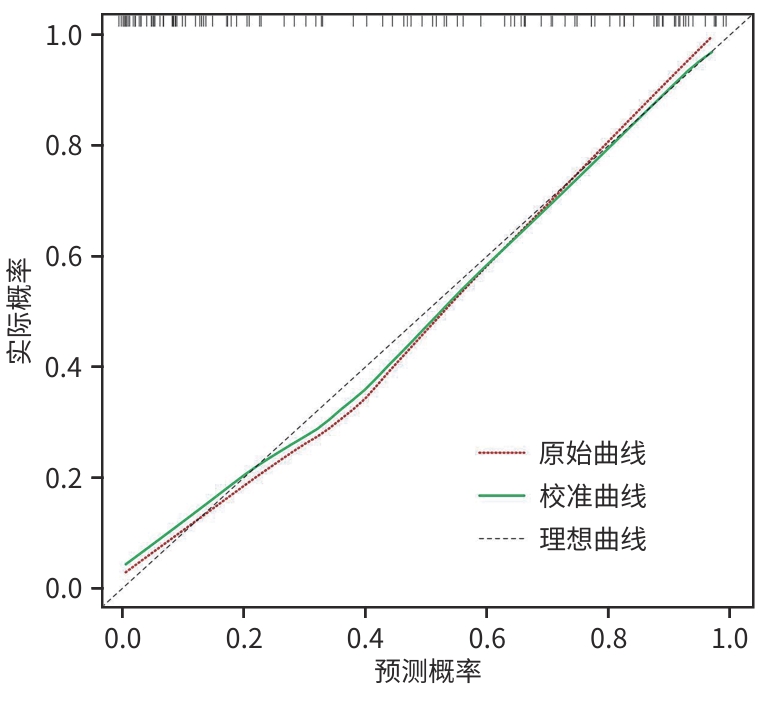
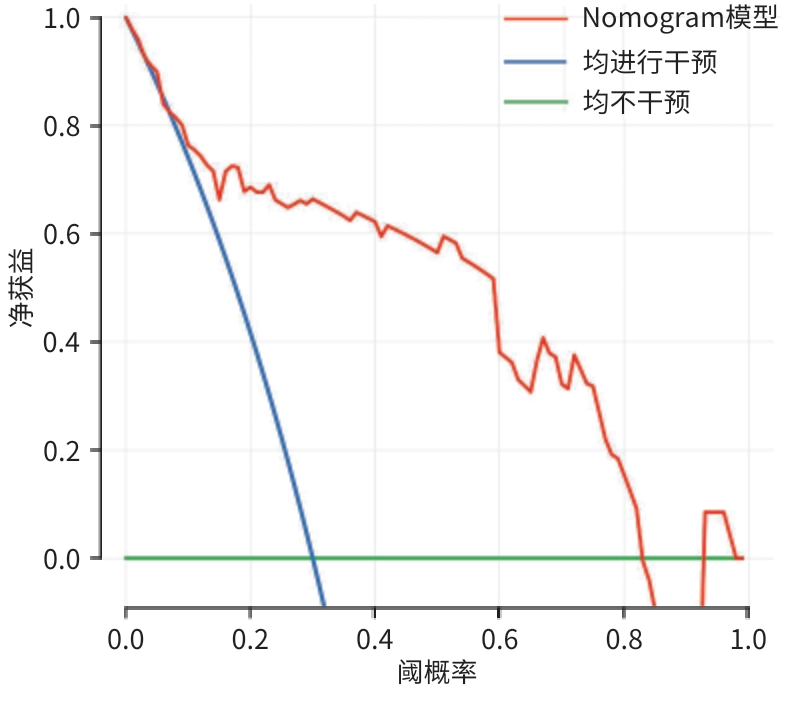
目的 本研究通过构建基于磁共振胆道相关参数和肝肌比的Nomogram预测模型,探讨该预测模型在肝占位患者术前肝储备功能评估中的应用价值。 方法 收集2022年4月—2024年4月在广西医科大学附属武鸣医院住院并拟行手术的112例肝占位患者的临床资料和钆塞酸二钠增强MRI的影像资料。根据肝损伤程度,将患者分为肝功能代偿良好组(Child-Pugh A级65例)、肝功能失代偿组(Child-Pugh B级42例,C级5例)。测量两组患者不同增强扫描时期的肝肌比、胆总管相对强化程度及胆道评分,并运用单因素和多因素Logistic回归分析筛选独立的预测因素,进而构建Nomogram模型。同时绘制受试者操作特征曲线(ROC曲线)、校正曲线、决策曲线,以评估模型的区分度、准确性和临床应用价值。计量资料符合正态分布的数据两组间比较采用成组t检验;符合偏态分布的数据两组间比较采用Mann-Whitney U检验。计数资料两组间比较采用χ2检验。 结果 两组间肝胆期5 min肝肌比(Z=-3.99)、肝胆期10 min肝肌比(Z=-4.39)、肝胆期15 min肝肌比(Z=-4.23)、肝胆期20 min肝肌比(Z=-5.40)、胆总管相对强化程度(Z=-4.85)及胆道评分(t=7.99)比较差异均有统计学意义(P值均<0.001)。多因素Logistic回归分析显示,肝胆期10 min肝肌比(OR=0.63,95%CI:0.44~0.90)、肝胆期20 min肝肌比(OR=0.38,95%CI:0.17~0.82)及胆道评分(OR=0.17,95%CI:0.07~0.39)是术前诊断肝功能失代偿的独立影响因素(P值均<0.05)。基于肝胆期10 min肝肌比、肝胆期20 min肝肌比及胆道评分建立的Nomogram模型术前诊断肝功能失代偿的ROC曲线下面积为0.905(95%CI:0.849~0.960),敏感度为78.7%,特异度为89.2%。 结论 基于肝胆期10 min肝肌比、肝胆期20 min肝肌比及胆道评分构建的列线图模型,在术前能有效评估拟接受手术治疗的肝占位患者的肝储备功能状态。 Abstract:Objective To establish a nomogram predictive model based on magnetic resonance cholangiopancreatography-related parameters and liver-to-muscle ratio, and to investigate the application value of this model in preoperative assessment of liver reserve function in patients with hepatic space-occupying lesion. Methods Clinical data and Gd-EOB-DTPA MRI imaging data were collected from 112 patients with hepatic space-occupying lesion who were hospitalized and scheduled for surgery in Wuming Hospital of Guangxi Medical University from April 2022 to April 2024. According to the degree of liver injury, the patients were divided into Child-Pugh class A group (65 patients with compensated liver function) and Child-Pugh class B+C group (47 patients with decompensated liver function, including 42 patients with Child-Pugh class B liver function and 5 patients with Child-Pugh class C liver function). The two groups of patients were measured in terms of liver-to-muscle ratio, relative signal intensity of the common bile duct, and bile duct score in different phases of contrast-enhanced CT scan, and univariate and multivariate Logistic regression analyses were used to identify independent predictive factors and establish a nomogram model. In addition, the receiver operating characteristic (ROC) curve, the calibration curve, and the decision curve were plotted to assess the discriminatory ability, accuracy, and clinical application value of the model. The independent-samples t test was used for comparison of normally distributed continuous data between two groups, and the Mann-Whitney U test was used for comparison of data with skewed distribution between two groups; the chi-square test was used for comparison of categorical data between two groups. Results There were significant differences between the two groups in liver-to-muscle ratio at 5 minutes (Z=-3.99, P<0.001), 10 minutes (Z=-4.39, P<0.001), 15 minutes (Z=-4.23, P<0.001), and 20 minutes (Z=-5.40, P<0.001) during the hepatobiliary phase, the relative enhancement degree of the common bile duct (Z=-4.85, P<0.001), and bile duct score (t=7.99, P<0.001). The multivariate Logistic regression analysis showed that liver-to-muscle ratio at 10 minutes during the hepatobiliary phase (odds ratio [OR]=0.63, 95% confidence interval [CI]: 0.44 — 0.90, P<0.05), liver-to-muscle ratio at 20 minutes during the hepatobiliary phase (OR=0.38, 95%CI: 0.17 — 0.82, P<0.05), and bile duct score (OR=0.17, 95%CI: 0.07 — 0.39, P<0.05) were independent influencing factors for the preoperative diagnosis of liver function decompensation. The nomogram model established based on liver-to-muscle ratio at 10 minutes during the hepatobiliary phase, liver-to-muscle ratio at 20 minutes during the hepatobiliary phase, and bile duct score had an area under the ROC curve of 0.905 (95%CI: 0.849 — 0.960), with a sensitivity of 78.7% with a specificity of 89.2%. Conclusion The nomogram model established based on the liver-to-muscle ratio at 10 and 20 minutes during the hepatobiliary phase and bile duct score can effectively assess the status of liver reserve function in patients with hepatic space-occupying lesion before surgery. -
Key words:
- Liver Neoplasms /
- Magnetic Resonance Imaging /
- Nomograms
-
表 1 肝功能代偿良好组与肝功能失代偿组一般资料比较
Table 1. Comparison of general data between the well-compensated and decompensated groups
项目 合计(n=112) 肝功能代偿
良好组(n=65)肝功能失代偿组
(n=47)统计值 P值 年龄(岁) 56.58±11.51 55.95±13.02 57.45±9.08 t=-0.72 0.476 动脉期肝肌比 1.62(1.45~1.85) 1.63(1.46~1.81) 1.61(1.44~1.87) Z=-0.40 0.693 门静脉期肝肌比 2.10(1.95~2.35) 2.12(1.96~2.34) 2.06(1.86~2.35) Z=-0.79 0.431 移行期肝肌比 2.15(1.93~2.36) 2.19(2.01~2.40) 2.09(1.87~2.28) Z=-1.83 0.068 肝胆期5 min肝肌比 2.33(2.03~2.61) 2.48(2.21~2.62) 2.03(1.88~2.38) Z=-3.99 <0.001 肝胆期10 min肝肌比 3.23(2.56~5.67) 4.40(2.91~7.04) 2.70(2.26~3.71) Z=-4.39 <0.001 肝胆期15 min肝肌比 3.13(2.45~4.93) 3.65(2.90~6.00) 2.60(2.10~3.41) Z=-4.23 <0.001 肝胆期20 min肝肌比 2.69(2.16~3.29) 2.92(2.63~3.63) 2.14(1.83~2.66) Z=-5.40 <0.001 胆总管相对强化程度 3.69(2.62~5.92) 4.60(3.42~8.29) 2.67(2.21~3.65) Z=-4.85 <0.001 性别[例(%)] χ2=1.58 0.209 男 89(79.46) 49(75.38) 40(85.11) 女 23(20.54) 16(24.62) 7(14.89) 胆道评分(分) 2.76±0.08 3.18±0.66 2.17±0.67 t=7.99 <0.001 表 2 单因素Logistic回归分析
Table 2. Univariate logistic regression analyses
因素 β值 SE Wald值 P值 OR(95%CI) 动脉期肝肌比 0.07 0.53 0.02 0.891 1.08(0.38~3.03) 门静脉期肝肌比 -0.46 0.54 0.74 0.390 0.63(0.22~1.80) 移行期肝肌比 -0.84 0.56 2.23 0.136 0.43(0.14~1.30) 肝胆期5 min肝肌比 -1.24 0.47 6.90 0.009 0.29(0.12~0.73) 肝胆期10 min肝肌比 -0.59 0.15 16.38 <0.001 0.55(0.42~0.74) 肝胆期15 min肝肌比 -0.45 0.13 11.91 <0.001 0.64(0.49~0.82) 肝胆期20 min肝肌比 -1.27 0.36 12.25 <0.001 0.28(0.14~0.57) 胆总管相对强化程度 -0.25 0.08 9.35 0.002 0.78(0.67~0.91) 胆道评分 -2.22 0.41 28.79 <0.001 0.11(0.05~0.25) 表 3 多因素Logistic 回归分析
Table 3. Multivariate logistic regression analyses
因素 β值 SE Z值 P值 OR(95%CI) 肝胆期10 min肝肌比 -0.46 0.18 -2.50 0.012 0.63(0.44~0.90) 肝胆期20 min肝肌比 -0.98 0.40 -2.46 0.014 0.38(0.17~0.82) 胆道评分 -1.78 0.43 -4.19 <0.001 0.17(0.07~0.39) 表 4 MRI指标及Nomogram模型区分肝功能代偿良好与肝功能失代偿的诊断效能
Table 4. MRI indicators and the Nomogram model distinguish the diagnostic performance of well-compensated liver function from decompensated hepatic function
项目 AUC P值 95%CI 敏感度 特异度 截断值 Z值 P值1) 动脉期肝肌比 0.522 0.691 0.411~0.633 0.769 0.362 1.455 5.979 <0.001 门静脉期肝肌比 0.544 0.430 0.433~0.655 0.846 0.298 1.905 5.894 <0.001 移行期肝肌比 0.601 0.068 0.494~0.709 0.754 0.447 2.000 5.185 <0.001 肝胆期5 min肝肌比 0.722 <0.001 0.617~0.827 0.923 0.553 2.055 3.521 <0.001 肝胆期10 min肝肌比 0.743 <0.001 0.654~0.833 0.462 0.957 4.985 3.903 <0.001 肝胆期15 min肝肌比 0.735 <0.001 0.641~0.829 0.769 0.681 2.865 3.570 <0.001 肝胆期20 min肝肌比 0.730 <0.001 0.631~0.828 0.877 0.533 2.475 3.864 <0.001 胆总管相对强化程度 0.770 <0.001 0.678~0.861 0.662 0.809 3.880 3.097 0.002 胆道评分 0.846 <0.001 0.769~0.923 0.892 0.766 2.500 2.626 0.009 Nomogram模型 0.905 <0.001 0.849~0.960 0.787 0.892 0.545 注:1)与Nomogram模型AUC比较。
-
[1] WANG YX, PAN KF, LI WQ. Interpretation on the report of global cancer statistics 2022[J/CD]. J Multidiscip Cancer Manag(Electronic Edition), 2024, 10( 3): 1- 16. DOI: 10.12151/JMCM.2024.03-01.王裕新, 潘凯枫, 李文庆. 2022全球癌症统计报告解读[J/CD]. 肿瘤综合治疗电子杂志, 2024, 10( 3): 1- 16. DOI: 10.12151/JMCM.2024.03-01. [2] SØREIDE JA, DESHPANDE R. Post hepatectomy liver failure(PHLF)-Recent advances in prevention and clinical management[J]. Eur J Surg Oncol, 2021, 47( 2): 216- 224. DOI: 10.1016/j.ejso.2020.09.001. DOI: 10.12151/JMCM.2024.03-01. [3] WU T, CHEN L. New advances in the precision diagnosis and treatment of liver cancer[J]. J Clin Hepatol, 2022, 38( 3): 497- 498. DOI: 10.3969/j.issn.1001-5256.2022.03.001.吴彤, 陈磊. 肝癌精准诊疗新进展[J]. 临床肝胆病杂志, 2022, 38( 3): 497- 498. DOI: 10.3969/j.issn.1001-5256.2022.03.001. [4] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2024version)[J]. J Clin Hepatol, 2024, 40( 12): 2371- 2387. DOI: 10.12449/JCH241206.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2024年版)[J]. 临床肝胆病杂志, 2024, 40( 12): 2371- 2387. DOI: 10.12449/JCH241206. [5] DONG SQ, MA QZ, WU CN, et al. Imaging quality of biliary tract and detecting diseases with hepatobiliary phase Gd-EOB-DTPA contrast-enhanced MR cholangiography based on 3D-VIBE and 3D-FLASH sequences[J]. Chin J Med Imag Technol, 2023, 39( 6): 866- 871. DOI: 10.13929/j.issn.1003-3289.2023.06.015.董思情, 马巧稚, 吴春楠, 等. 3D-VIBE与3D-FLASH序列肝胆特异期Gd-EOB-DTPA增强MR胆道成像显示胆道系统图像质量及检出病变[J]. 中国医学影像技术, 2023, 39( 6): 866- 871. DOI: 10.13929/j.issn.1003-3289.2023.06.015. [6] WANG Q, BRISMAR TB, GILG S, et al. Multimodal perioperative assessment of liver function and volume in patients undergoing hepatectomy for colorectal liver metastasis: A comparison of the indocyanine green retention test, 99mTc mebrofenin hepatobiliary scintigraphy and gadoxetic acid enhanced MRI[J]. Br J Radiol, 2022, 95( 1139): 20220370. DOI: 10.1259/bjr.20220370. [7] SHAO J. Research of gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid enhanced magnetic resonance imaging in evaluating liver function[D]. Taiyuan: Shanxi Med Univ, 2021. DOI: 10.27288/d.cnki.gsxyu.2021.000980.邵佳. 应用钆塞酸二钠增强磁共振成像评估肝功能的研究[D]. 太原: 山西医科大学, 2021. DOI: 10.27288/d.cnki.gsxyu.2021.000980. [8] HAN D, LIU JY, JIN EH, et al. Liver assessment using Gd-EOB-DTPA-enhanced magnetic resonance imaging in primary biliary cholangitis patients[J]. Jpn J Radiol, 2019, 37( 5): 412- 419. DOI: 10.1007/s11604-019-00822-6. [9] LI LJ, JIA QL, LIU ZF, et al. Study on the relationship between Gd-EOB-DTPA enhanced MRI cholangiography and different grades of liver cirrhosis[J]. J Imag Res Med Appl, 2020, 4( 8): 70- 71.李亮杰, 贾啟龙, 刘志飞, 等. Gd-EOB-DTPA增强MRI胆道成像与不同级别肝硬化关系的研究[J]. 影像研究与医学应用, 2020, 4( 8): 70- 71. [10] LIU D, HUANG JY, HU CH. Effect of different liver function on contrast-enhanced MR cholangiography with Gd-EOB-DTPA[J]. J Med Imag, 2019, 29( 1): 70- 73, 94.刘冬, 黄瑾瑜, 胡春洪. Gd-EOB-DTPA增强MRI胆道成像与不同级别肝硬化关系的研究[J]. 医学影像学杂志, 2019, 29( 1): 70- 73, 94. [11] RIMINI M, ROVESTI G, CASADEI-GARDINI A, et al. Child Pugh and ALBI grade: past, present or future?[J]. Ann Transl Med, 2020, 8( 17): 1044. DOI: 10.21037/atm-20-3709. [12] MORANDI A, RISALITI M, MONTORI M, et al. Predicting post-hepatectomy liver failure in HCC patients: A review of liver function assessment based on laboratory tests scores[J]. Medicina(Kaunas), 2023, 59( 6): 1099. DOI: 10.3390/medicina59061099. [13] LIN WH, LI K. Recent advances in preoperative assessment of hepatic functional reserve for hepatectomy[J]. Chin J Surg, 2021, 59( 5): 392- 396. DOI: 10.3760/cma.j.cn112139-20200506-00362.林伟鸿, 李凯. 肝切除术前肝脏储备功能评估方式的新进展[J]. 中华外科杂志, 2021, 59( 5): 392- 396. DOI: 10.3760/cma.j.cn112139-20200506-00362. [14] HE Q, LIU K, WANG CH, et al. Interpretation on the key points of guideline for the diagnose and treatment of primary liver cancer(2022 edition)[J]. Med J West China, 2023, 35( 4): 474- 479. DOI: 10.3969/j.issn.1672-3511.2023.04.002.贺庆, 刘坤, 王超红, 等.《原发性肝癌诊疗指南(2022年版)》解读[J]. 西部医学, 2023, 35( 4): 474- 479. DOI: 10.3969/j.issn.1672-3511.2023.04.002. [15] JIANG Y, QIU WJ, ZHOU ZP. The application of Gd-EOB-DTPA-enhanced MRI T1 mapping and its research progresses in hepatic diseases[J]. Int J Med Radiol, 2019, 42( 02): 208- 211. DOI: 10.19300/j.2019.Z6410.蒋宇, 邱维加, 周智鹏. Gd-EOB-DTPA增强MRI T1 mapping技术在肝脏疾病的应用进展[J]. 国际医学放射学杂志, 2019, 42( 02): 208- 211. DOI: 10.19300/j.2019.Z6410. [16] WEN X, FENG X, KANG Y, et al. Application progress of Gd-EOB-DTPA-enhanced MRI T1 mapping in hepatic diffuse diseases[J]. Curr Med Imaging, 2022, 18( 12): 1276- 1281. DOI: 10.2174/1573405617666211130153450. [17] CAPARROZ C, FORNER A, RIMOLA J, et al. Portal hypertension may influence the registration of hypointensity of small hepatocellular carcinoma in the hepatobiliary phase in gadoxetic acid MR[J]. Radiol Oncol, 2022, 56( 3): 292- 302. DOI: 10.2478/raon-2022-0024. [18] TSUJITA Y, SOFUE K, KOMATSU S, et al. Prediction of post-hepatectomy liver failure using gadoxetic acid-enhanced magnetic resonance imaging for hepatocellular carcinoma with portal vein invasion[J]. Eur J Radiol, 2020, 130: 109189. DOI: 10.1016/j.ejrad.2020.109189. [19] BEER L, MANDORFER M, BASTATI N, et al. Inter- and intra-reader agreement for gadoxetic acid-enhanced MRI parameter readings in patients with chronic liver diseases[J]. Eur Radiol, 2019, 29( 12): 6600- 6610. DOI: 10.1007/s00330-019-06182-z. [20] WANG YJ, ZHANG L, NING J, et al. Preoperative remnant liver function evaluation using a routine clinical dynamic Gd-EOB-DTPA-enhanced MRI protocol in patients with hepatocellular carcinoma[J]. Ann Surg Oncol, 2021, 28( 7): 3672- 3682. DOI: 10.1245/s10434-020-09361-1. [21] BASTATI N, BEER L, BA-SSALAMAH A, et al. Gadoxetic acid-enhanced MRI-derived functional liver imaging score(FLIS) and spleen diameter predict outcomes in ACLD[J]. J Hepatol, 2022, 77( 4): 1005- 1013. DOI: 10.1016/j.jhep.2022.04.032. [22] HU JH, WANG XX, HUANG JC, et al. Clinical value of Gd-EOB-DTPA enhanced MRI for preoperative evaluation of hepatic function preservation in patients with liver tumors[J]. Chin Imag J Integr Tradit West Med, 2022, 20( 3): 233- 238. DOI: 10.3969/j.issn.1672-0512.2022.03.009.胡景卉, 王笑笑, 黄京城, 等. Gd-EOB-DTPA增强MRI对肝肿瘤术前肝储备功能评估的临床价值[J]. 中国中西医结合影像学杂志, 2022, 20( 3): 233- 238. DOI: 10.3969/j.issn.1672-0512.2022.03.009. [23] ZHU Z, CAO YL, SUN G, et al. Summary of classification methods of hepatic insufficiency[J]. China Pharm, 2012, 15( 3): 418- 421. DOI: 10.3969/j.issn.1008-049X.2012.03.053.朱珠, 曹运莉, 孙钢, 等. 肝功能不全分级方法概述[J]. 中国药师, 2012, 15( 3): 418- 421. DOI: 10.3969/j.issn.1008-049X.2012.03.053. [24] ARAKI K, HARIMOTO N, KUBO N, et al. Functional remnant liver volumetry using Gd-EOB-DTPA-enhanced magnetic resonance imaging(MRI) predicts post-hepatectomy liver failure in resection of more than one segment[J]. HPB(Oxford), 2020, 22( 2): 318- 327. DOI: 10.1016/j.hpb.2019.08.002. [25] HAMM B, STAKS T, MÜHLER A, et al. Phase I clinical evaluation of Gd-EOB-DTPA as a hepatobiliary MR contrast agent: Safety, pharmacokinetics, and MR imaging[J]. Radiology, 1995, 195( 3): 785- 792. DOI: 10.1148/radiology.195.3.7754011. [26] REIMER P, SCHNEIDER G, SCHIMA W. Hepatobiliary contrast agents for contrast-enhanced MRI of the liver: Properties, clinical development and applications[J]. Eur Radiol, 2004, 14( 4): 559- 578. DOI: 10.1007/s00330-004-2236-1. [27] PASTOR CM, VILGRAIN V. Steatosis alters the activity of hepatocyte membrane transporters in obese rats[J]. Cells, 2021, 10( 10): 2733. DOI: 10.3390/cells10102733. [28] ZHOU XJ, LONG LL, MO ZQ, et al. OATP1B3 expression in hepatocellular carcinoma correlates with intralesional Gd-EOB-DTPA uptake and signal intensity on Gd-EOB-DTPA-enhanced MRI[J]. Cancer Manag Res, 2021, 13: 1169- 1177. DOI: 10.2147/CMAR.S292197. [29] KIRIMKER EO, KIRAC AT, CELIK SU, et al. Comparison of anatomic and non-anatomic liver resection for hepatocellular carcinoma: A retrospective cohort study[J]. Medicina(Kaunas), 2022, 58( 9): 1305. DOI: 10.3390/medicina58091305. [30] YAN LN, CHEN XL, LI ZH, et al. Perioperative management of primary liver cancer[J]. World J Gastroenterol, 2007, 13( 13): 1970- 1974. DOI: 10.3748/wjg.v13.i13.1970. -



 PDF下载 ( 2327 KB)
PDF下载 ( 2327 KB)


 下载:
下载: