非酒精性脂肪性肝病与抑郁症关系的系统评价及Meta分析
DOI: 10.12449/JCH250914
Association between non-alcoholic fatty liver disease and depression: A systematic review and Meta-analysis
-
摘要:
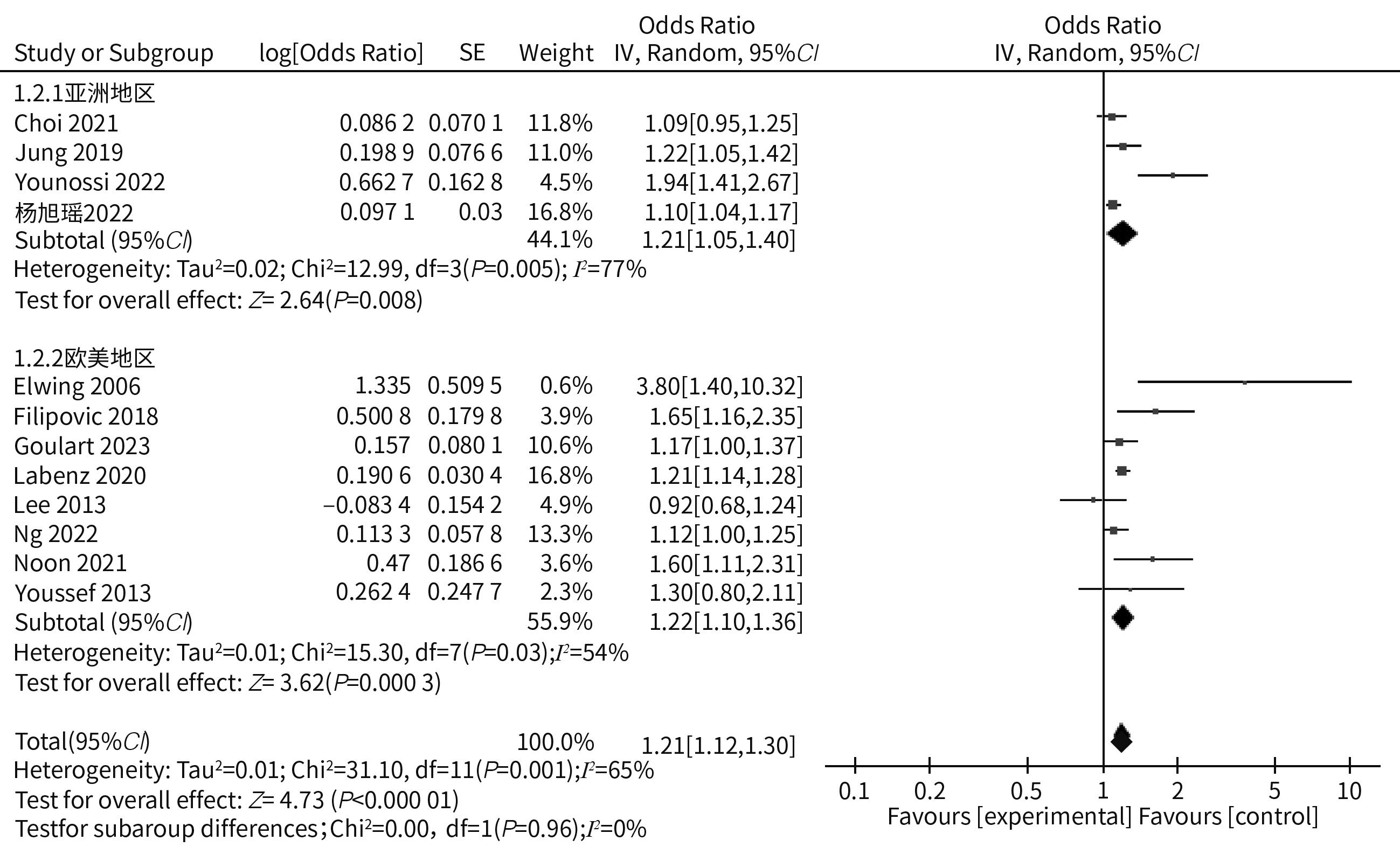
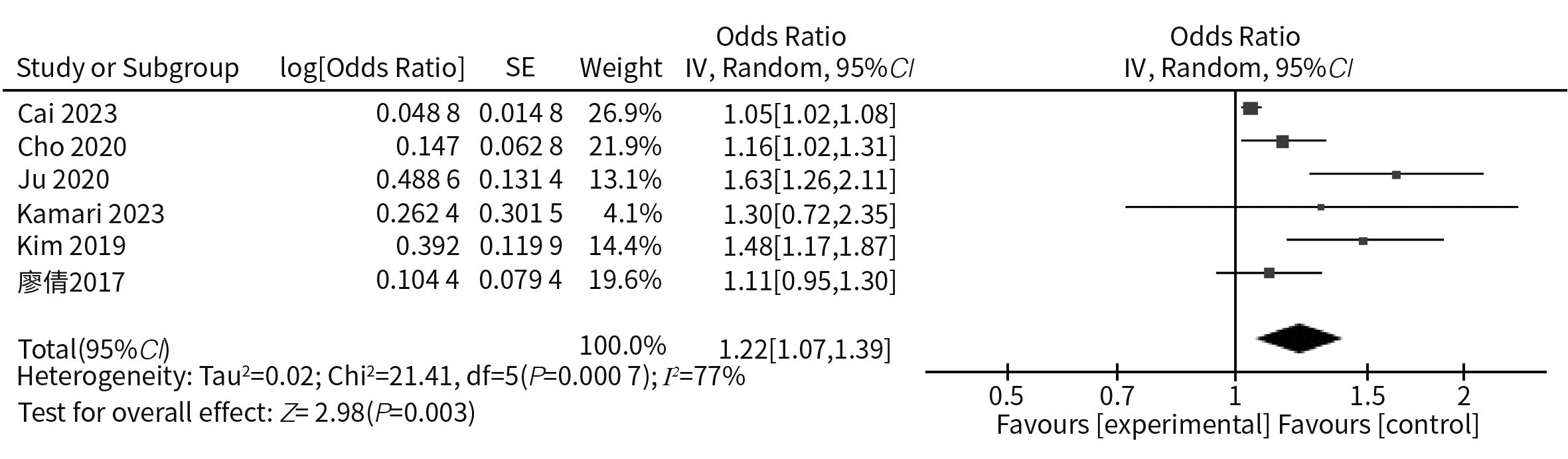
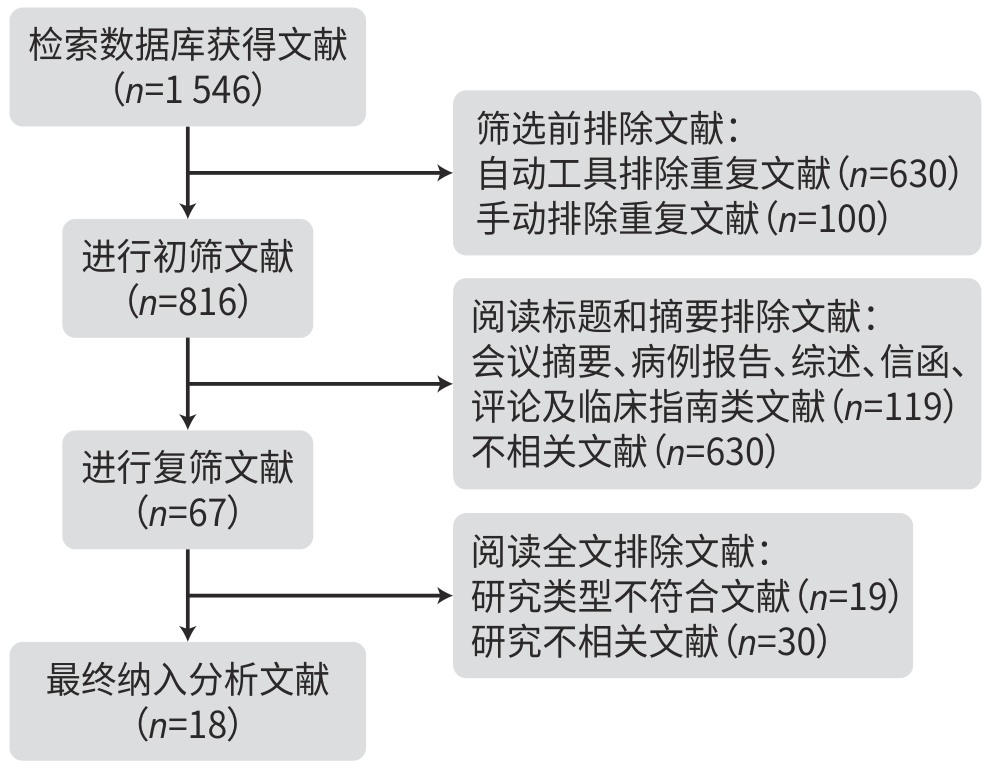
目的 系统评价非酒精性脂肪性肝病(NAFLD)与抑郁症的关联性,为临床协同管理提供依据。 方法 本研究根据PRISMA指南完成,PROSPERO注册号:CRD42023482013。检索PubMed、Embase、Cochrane Library、Web of Science、中国知网、万方、维普、CBM数据库建库至2024年11月1日公开发表的NAFLD和抑郁症二者相关性的研究文献,根据纳入和排除标准筛选文献并提取数据。采用RevMan 5.3进行Meta分析。 结果 共纳入18项研究,涉及396 793例参与者。12项研究探讨NAFLD对抑郁症的影响,共涉及224 269例参与者,其中包含75 574例NAFLD患者。Meta分析显示,NAFLD显著增加抑郁症发生风险(OR=1.21,95%CI: 1.12~1.30,P<0.001)。6项研究分析抑郁症对NAFLD的影响,共涉及172 524例参与者,其中包含29 368例抑郁症患者。Meta分析显示,抑郁症导致NAFLD风险显著增加(OR=1.13,95%CI: 1.05~1.22,P=0.001)。 结论 NAFLD与抑郁症存在显著的双向关联。在初诊和随访时,建议对NAFLD患者行抑郁症筛查并加强心理健康监测;对抑郁症患者需重视代谢功能评估并实施运动干预。 Abstract:Objective To systematically review the association between non-alcoholic fatty liver disease (NAFLD) and depression, and to provide a basis for synergistic management in clinical practice. Methods This study was conducted according to the PRISMA guidelines, with the PROSPERO registration number of CRD42023482013. PubMed, Embase, the Cochrane Library, Web of Science, CNKI, Wanfang Data, VIP, and CBM were searched for articles on the association between NAFLD and depression published up to November 1, 2024. The articles were screened according to the inclusion and exclusion criteria, and related data were extracted. RevMan 5.3 was used to perform the Meta-analysis. Results A total of 18 studies were included, involving 396 793 participants. Among these studies, 12 discussed the influence of NAFLD on depression, involving 224 269 participants, among whom there were 75 574 patients with NAFLD. The Meta-analysis showed that NAFLD was significantly associated with the risk of depression (odds ratio [OR]=1.21, 95% confidence interval [CI]: 1.12 — 1.30, P<0.001). Six studies examined the influence of depression on NAFLD, involving 172 524 participants, among whom there were 29 368 patients with depression. The meta-analysis showed that depression caused a significant increase in the risk of NAFLD (OR=1.13, 95%CI: 1.05 — 1.22, P=0.001). Conclusion There is a significant bidirectional association between NAFLD and depression. It is recommended to perform the screening for depression and enhance mental health monitoring in patients with NAFLD, and metabolic function assessment and exercise intervention should be performed for patients with depression. -
Key words:
- Non-Alcoholic Fatty Liver Disease /
- Depressive Disorder /
- Meta-Analysis
-
表 1 纳入研究的基本特征
Table 1. Basic features of the included study
作者及发表年份 国家或
地区总样本量
(例)研究对象
数量(例)研究对象
年龄(岁)研究类型 OR/RR/HR
(95%CI)调整的变量 NOS评分
(分)NAFLD对抑郁症的影响 Choi,2021[22] 韩国 25 333 7 846 NAFLD 48.4±10.1 回顾性研究 1.09(0.95~1.26) 年龄、性别、糖尿病、 血压、吸烟 7 Elwing,2006[23] 美国 72 36 NASH 51.4±2.0 前瞻性研究 3.8(1.40~10.20) 年龄 7 Filipovic,2018[24] 塞尔维亚 283 40 NAFLD 47.88±6.07 前瞻性研究 1.65(1.16~2.36) BMI、高血压、代谢综合征 8 Goulart,2023[25] 巴西 7 241 2 223 NAFLD 49.0 前瞻性研究 1.17(1.00~1.38) 年龄、性别 7 Jung,2019[26] 韩国 112 797 31 635 NAFLD 前瞻性研究 1.32(1.17~1.48) 年龄、性别、家庭月收入、婚姻状况、工作、平均饮酒量、吸烟、
收缩压、TC、HDL-C、糖尿病、体力活动、BMI、HOMA-IR7 Labenz,2020[27] 德国 39 742 19 871 NAFLD 58.5±14.2 回顾性研究 1.21(1.14~1.26) 糖尿病、心血管疾病、哮喘、慢性阻塞性肺病、癌症 6 Lee,2013[28] 美国 10 231 497 NAFLD 49.62±0.72 回顾性研究 0.92(0.68~1.24) 性别、家庭收入、吸烟、BMI、血脂异常、心脏病、慢性肝病、药
物使用史6 Ng,2022[29] 美国 21 414 6 726 NAFLD 52.16 回顾性研究 1.12(1.00~1.26) 年龄、性别、种族、糖尿病、超重 7 Noon,2021[30] 美国 160 160 NAFLD 15±1.8 前瞻性研究 1.60(1.11~2.52) BMI、ALT、AST、GGT 9 Younossi,
2022[31]18个国家
或地区1)5 691 5 691 NAFLD 51 回顾性研究 1.94(1.41~2.67) 年龄、性别、肥胖、焦虑、2型糖尿病、高脂血症、高血压、心肌
梗死、中风、充血性心力衰竭6 Youssef,2013[32] 美国 567 567 NAFLD 49±1.0 回顾性研究 1.30(0.80~2.11) 年龄、性别、种族、BMI、糖尿病、高血压 7 杨旭瑶,2022[33] 中国 738 282 NAFLD 41.17±11.57 回顾性研究 1.10(1.03~1.16) 性别、BMI、TC、TG 6 抑郁症对NAFLD的影响 Cai,2023[34] 美国 3 263 3 263抑郁症 48.0 回顾性研究 1.05(1.02~1.08) 年龄、性别、种族/民族、教育水平、家庭贫困收入比、婚姻状
况、体力活动、过度饮酒、吸烟、BMI、乙型/丙型肝炎、糖尿病、
高血压、心血管疾病6 Cho,2021[35] 韩国 142 005 16 961抑郁症 34.8 回顾性研究 1.07(1.03~1.11) 年龄、性别、教育水平、BMI、吸烟、体力活动、总能量摄入、糖
尿病、高血压、心血管疾病、收缩压、血糖、TC、TG、HDL-C、
HOMA-IR、Hs-CRP8 Kamari,2023[36] 印度 7 114 7 114抑郁症 45.78±7.80 回顾性研究 1.30(0.72~2.35) 年龄、婚姻状况、居住地、饮酒情况 6 Kim,2019[37] 美国 10 484 1 162抑郁症 49.5±0.6 回顾性研究 1.48(1.17~1.87) 年龄、性别、种族/民族、教育水平、婚姻状况、经济状况、吸烟、
高血压、体力活动、TC、糖尿病、腰围、BMI7 Lee,2021[38] 韩国 4 688 422抑郁症 50.1 回顾性分析 1.63(1.26~2.10) 年龄、性别、婚姻状况、个人收入、吸烟、糖尿病、高血压、心血
管疾病7 廖倩,2017[39] 中国 4 970 446抑郁症 46 前瞻性研究 1.11(0.95~1.31) 年龄、性别、教育水平、现在或既往吸烟和饮酒、打鼾、收缩
压、舒张压、睡眠持续时间、糖尿病、BMI、步行时间、血脂6 注:HDL-C,高密度脂蛋白胆固醇;HOMA-IR,稳态模型的胰岛素抵抗指数;Hs-CRP,超敏C反应蛋白。1)包括中国内地、中国香港、中国台湾、澳大利亚、古巴、埃及、希腊、印度、意大利、日本、沙特阿拉伯、马来西亚、墨西哥、巴基斯坦、俄罗斯、西班牙、土耳其和美国。
-
[1] ANSTEE QM, DARLAY R, COCKELL S, et al. Genome-wide association study of non-alcoholic fatty liver and steatohepatitis in a histologically characterised cohort[J]. J Hepatol, 2020, 73( 3): 505- 515. DOI: 10.1016/j.jhep.2020.04.003. [2] ESTES C, ANSTEE QM, ARIAS-LOSTE MT, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016-2030[J]. J Hepatol, 2018, 69( 4): 896- 904. DOI: 10.1016/j.jhep.2018.05.036. [3] LI F, LI MW, WANG YS. Therapeutic paradigms and potential therapies for nonalcoholic steatohepatitis[J]. J Clin Hepatol, 2024, 40( 10): 2082- 2086. DOI: 10.12449/JCH241025.李凤, 李茂微, 王雨杉. 非酒精性脂肪肝病的治疗模式和潜在疗法[J]. 临床肝胆病杂志, 2024, 40( 10): 2082- 2086. DOI: 10.12449/JCH241025. [4] BATTLE DE. Diagnostic and statistical manual of mental disorders(DSM)[J]. Codas, 2013, 25( 2): 191- 192. DOI: 10.1590/s2317-17822-013000200017. [5] ZHANG Y, JIA XC, YANG YL, et al. Change in the global burden of depression from 1990-2019 and its prediction for 2030[J]. J Psychiatr Res, 2024, 178: 16- 22. DOI: 10.1016/j.jpsychires.2024.07.054. [6] BERGFELD IO, MANTIONE M, FIGEE M, et al. Treatment-resistant depression and suicidality[J]. J Affect Disord, 2018, 235: 362- 367. DOI: 10.1016/j.jad.2018.04.016. [7] PARK SJ, ROH S, HWANG J, et al. Association between depression and metabolic syndrome in Korean women: Results from the Korean national health and nutrition examination survey(2007-2013)[J]. J Affect Disord, 2016, 205: 393- 399. DOI: 10.1016/j.jad.2016.08.022. [8] WANG L, GUO JH, LU JP. Risk factor compositions of nonalcoholic fatty liver disease change with body mass index in males and females[J]. Oncotarget, 2016, 7( 24): 35632- 35642. DOI: 10.18632/oncotarget.9691. [9] CHEN ZB, HUANG LY, WANG BY, et al. Research advances in the association between metabolic associated fatty liver and type 2 diabetes mellitus and the mechanism of comorbidity[J]. J Clin Hepatol, 2023, 39( 10): 2454- 2459. DOI: 10. 3969/j.issn.1001-5256.2023.10.025.陈兆斌, 黄丽媛, 王炳元, 等. 代谢相关脂肪性肝病与2型糖尿病的关系及共病机制研究进展[J]. 临床肝胆病杂志, 2023, 39( 10): 2454- 2459. DOI: 10. 3969/j.issn.1001-5256.2023.10.025. [10] GOLDBACHER EM, BROMBERGER J, MATTHEWS KA. Lifetime history of major depression predicts the development of the metabolic syndrome in middle-aged women[J]. Psychosom Med, 2009, 71( 3): 266- 272. DOI: 10.1097/PSY.0b013e318197a4d5. [11] KINDER LS, CARNETHON MR, PALANIAPPAN LP, et al. Depression and the metabolic syndrome in young adults: Findings from the Third National Health and Nutrition Examination Survey[J]. Psychosom Med, 2004, 66( 3): 316- 322. DOI: 10.1097/01.psy.0000124755.91880.f4. [12] RORIZ-CRUZ M, ROSSET I, WADA T, et al. Stroke-independent association between metabolic syndrome and functional dependence, depression, and low quality of life in elderly community-dwelling Brazilian people[J]. J Am Geriatr Soc, 2007, 55( 3): 374- 382. DOI: 10.1111/j.1532-5415.2007.01068.x. [13] GARVEY WT, MECHANICK JI, BRETT EM, et al. American association of clinical endocrinologists and American college of endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity[J]. Endocr Pract, 2016, 22( Suppl 3): 1- 203. DOI: 10.4158/EP1-61365.GL. [14] SINGH MK, LESLIE SM, PACKER MM, et al. Brain and behavioral correlates of insulin resistance in youth with depression and obesity[J]. Horm Behav, 2019, 108: 73- 83. DOI: 10.1016/j.yhbeh.2018.03.009. [15] WATSON K, NASCA C, AASLY L, et al. Insulin resistance, an unmasked culprit in depressive disorders: Promises for interventions[J]. Neuropharmacology, 2018, 136( Pt B): 327- 334. DOI: 10.1016/j.neuropharm.2017.11.038. [16] LYRA E SILVA NM, LAM MP, SOARES CN, et al. Insulin resistance as a shared pathogenic mechanism between depression and type 2 diabetes[J]. Front Psychiatry, 2019, 10: 57. DOI: 10.3389/fpsyt.2019.00057. [17] PAGE MJ, MCKENZIE JE, BOSSUYT PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews[J]. BMJ, 2021, 372: n71. DOI: 10.1136/bmj.n71. [18] STANG A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses[J]. Eur J Epidemiol, 2010, 25( 9): 603- 605. DOI: 10.1007/s10654-010-9491-z. [19] MAURICE J, MANOUSOU P. Non-alcoholic fatty liver disease[J]. Clin Med, 2018, 18( 3): 245- 250. DOI: 10.7861/clinmedicine.18-3-245. [20] FRIEDRICH MJ. Depression is the leading cause of disability around the world[J]. JAMA, 2017, 317( 15): 1517. DOI: 10.1001/jama.2017.3826. [21] VIERA AJ. Odds ratios and risk ratios: What’s the difference and why does it matter?[J]. South Med J, 2008, 101( 7): 730- 734. DOI: 10.1097/SMJ.0b013e31817a7ee4. [22] CHOI JM, CHUNG GE, KANG SJ, et al. Association between anxiety and depression and nonalcoholic fatty liver disease[J]. Front Med(Lausanne), 2021, 7: 585618. DOI: 10.3389/fmed.2020.585618. [23] ELWING JE, LUSTMAN PJ, WANG HL, et al. Depression, anxiety, and nonalcoholic steatohepatitis[J]. Psychosom Med, 2006, 68( 4): 563- 569. DOI: 10.1097/01.psy.0000221276.17823.df. [24] FILIPOVIĆ B, MARKOVIĆ O, ĐURIĆ V, et al. Cognitive changes and brain volume reduction in patients with nonalcoholic fatty liver disease[J]. Can J Gastroenterol Hepatol, 2018, 2018: 9638797. DOI: 10.1155/2018/9638797. [25] GOULART AC, BIANCHI LLT, BISMARCHI D, et al. Sex differences in the relationship between hepatic steatosis, mood and anxiety disorders[J]. J Psychosom Res, 2023, 168: 111216. DOI: 10.1016/j.jpsychores.2023.111216. [26] JUNG JY, PARK SK, OH CM, et al. Non-alcoholic fatty liver disease and its association with depression in Korean general population[J]. J Korean Med Sci, 2019, 34( 30): e199. DOI: 10.3346/jkms.2019.34.e199. [27] LABENZ C, HUBER Y, MICHEL M, et al. Nonalcoholic fatty liver disease increases the risk of anxiety and depression[J]. Hepatol Commun, 2020, 4( 9): 1293- 1301. DOI: 10.1002/hep4.1541. [28] LEE K, OTGONSUREN M, YOUNOSZAI Z, et al. Association of chronic liver disease with depression: A population-based study[J]. Psychosomatics, 2013, 54( 1): 52- 59. DOI: 10.1016/j.psym.2012.09.005. [29] NG CH, XIAO JL, CHEW NWS, et al. Depression in non-alcoholic fatty liver disease is associated with an increased risk of complications and mortality[J]. Front Med(Lausanne), 2022, 9: 985803. DOI: 10.3389/fmed.2022.985803. [30] NOON SL, D’ANNIBALE DA, SCHWIMMER MH, et al. Incidence of depression and anxiety in a cohort of adolescents with nonalcoholic fatty liver disease[J]. J Pediatr Gastroenterol Nutr, 2021, 72( 4): 579- 583. DOI: 10.1097/MPG.0000000000003024. [31] YOUNOSSI ZM, YILMAZ Y, YU ML, et al. Clinical and patient-reported outcomes from patients with nonalcoholic fatty liver disease across the world: Data from the global non-alcoholic steatohepatitis(NASH)/non-alcoholic fatty liver disease(NAFLD) registry[J]. Clin Gastroenterol Hepatol, 2022, 20( 10): 2296- 2306.e6. DOI: 10.1016/j.cgh.2021.11.004. [32] YOUSSEF NA, ABDELMALEK MF, BINKS M, et al. Associations of depression, anxiety and antidepressants with histological severity of nonalcoholic fatty liver disease[J]. Liver Int, 2013, 33( 7): 1062- 1070. DOI: 10.1111/liv.12165. [33] YANG XY, CHANG J, YU D, et al. The correlation between depression and non-alcoholic fatty liver disease[J]. J Int Psychiatry, 2022, 49( 5): 840- 845. DOI: 10.13479/j.cnki.jip.2022.05.018.杨旭瑶, 常江, 余荻, 等. 抑郁症与非酒精性脂肪性肝病的相关性分析[J]. 国际精神病学杂志, 2022, 49( 5): 840- 845. DOI: 10.13479/j.cnki.jip.2022.05.018. [34] CAI HW, ZHANG R, ZHAO CH, et al. Associations of depression score with metabolic dysfunction-associated fatty liver disease and liver fibrosis[J]. J Affect Disord, 2023, 334: 332- 336. DOI: 10.1016/j.jad.2023.04.093. [35] CHO IY, CHANG Y, SUNG E, et al. Depression and increased risk of non-alcoholic fatty liver disease in individuals with obesity[J]. Epidemiol Psychiatr Sci, 2021, 30: e23. DOI: 10.1017/S204579602000116X. [36] KAMARI N, FATEH HL, DARBANDI M, et al. Fatty liver index relationship with biomarkers and lifestyle: Result from RaNCD cohort study[J]. BMC Gastroenterol, 2023, 23( 1): 172. DOI: 10.1186/s12876-023-02785-5. [37] KIM D, YOO ER, LI AA, et al. Depression is associated with non-alcoholic fatty liver disease among adults in the United States[J]. Aliment Pharmacol Ther, 2019, 50( 5): 590- 598. DOI: 10.1111/apt.15395. [38] LEE JW, PARK SH. Association between depression and nonalcoholic fatty liver disease: Contributions of insulin resistance and inflammation[J]. J Affect Disord, 2021, 278: 259- 263. DOI: 10.1016/j.jad.2020.09.073. [39] LIAO Q, ZHENG Y, LIU XF, et al. Correlation of non-alcoholic fatty liver disease and depression in an elderly Chinese population[J]. J Third Mil Med Univ, 2017, 39( 19): 1954- 1959. DOI: 10.16016/j.1000-5404.2017-04136.廖倩, 郑怡, 刘羞菲, 等. 中老年人群非酒精性脂肪肝与抑郁症的相关性研究[J]. 第三军医大学学报, 2017, 39( 19): 1954- 1959. DOI: 10.16016/j.1000-5404.201704136. [40] KAČAVENDA-BABOVIĆ D, ĐURIĆ P, BABOVIĆ R, et al. Depression, anxiety and quality of life in patients with chronic hepatitis c virus infection in Vojvodina[J]. Acta Clin Croat, 2021, 60( 4): 579- 589. DOI: 10.20471/acc.2021.60.04.03. [41] LI SD, LI SL, DUAN F, et al. Depression and NAFLD risk: A meta-analysis and Mendelian randomization study[J]. J Affect Disord, 2024, 352: 379- 385. DOI: 10.1016/j.jad.2024.02.074. [42] LIANG YJ, ZOU LL, TIAN YL, et al. Dietary and metabolic risk of neuropsychiatric disorders: Insights from animal models[J]. Br J Nutr, 2021, 126( 12): 1771- 1787. DOI: 10.1017/S0007114521000659. [43] LUPPINO FS, DE WIT LM, BOUVY PF, et al. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies[J]. Arch Gen Psychiatry, 2010, 67( 3): 220- 229. DOI: 10.1001/archgenpsychiatry.2010.2. [44] LI W, LIU JY, CAI JJ, et al. NAFLD as a continuous driver in the whole spectrum of vascular disease[J]. J Mol Cell Cardiol, 2022, 163: 118- 132. DOI: 10.1016/j.yjmcc.2021.10.007. [45] CHAN KL, CATHOMAS F, RUSSO SJ. Central and peripheral inflammation link metabolic syndrome and major depressive disorder[J]. Physiology(Bethesda), 2019, 34( 2): 123- 133. DOI: 10.1152/physiol.00047.2018. [46] MARRIE RA, WALLD R, BOLTON JM, et al. Psychiatric comorbidity increases mortality in immune-mediated inflammatory diseases[J]. Gen Hosp Psychiatry, 2018, 53: 65- 72. DOI: 10.1016/j.genhosppsych.2018.06.001. [47] van der FELTZ-CORNELIS CM, VAN OS J, KNAPPE S, et al. Towards Horizon 2020: Challenges and advances for clinical mental health research-outcome of an expert survey[J]. Neuropsychiatr Dis Treat, 2014, 10: 1057- 1068. DOI: 10.2147/NDT.S59958. [48] SOTO-ANGONA Ó, ANMELLA G, VALDÉS-FLORIDO MJ, et al. Non-alcoholic fatty liver disease(NAFLD) as a neglected metabolic companion of psychiatric disorders: Common pathways and future approaches[J]. BMC Med, 2020, 18( 1): 261. DOI: 10.1186/s12916-020-01713-8. [49] GHANEI GHESHLAGH R, PARIZAD N, SAYEHMIRI K. The relationship between depression and metabolic syndrome: Systematic review and meta-analysis study[J]. Iran Red Crescent Med J, 2016, 18( 6): e26523. DOI: 10.5812/ircmj.26523. [50] KONTTINEN H, SILVENTOINEN K, SARLIO-LÄHTEENKORVA S, et al. Emotional eating and physical activity self-efficacy as pathways in the association between depressive symptoms and adiposity indicators[J]. Am J Clin Nutr, 2010, 92( 5): 1031- 1039. DOI: 10.3945/ajcn.2010.29732. [51] DAYABANDARA M, HANWELLA R, RATNATUNGA S, et al. Antipsychotic-associated weight gain: Management strategies and impact on treatment adherence[J]. Neuropsychiatr Dis Treat, 2017, 13: 2231- 2241. DOI: 10.2147/NDT.S113099. [52] GRACIOUS BL, BHATT R, POTTER C. Nonalcoholic fatty liver disease and fibrosis in youth taking psychotropic medications: Literature review, case reports, and management[J]. J Child Adolesc Psychopharmacol, 2015, 25( 8): 602- 610. DOI: 10.1089/cap.2015.0007. [53] MOUZAKI M, YODOSHI T, ARCE-CLACHAR AC, et al. Psychotropic medications are associated with increased liver disease severity in pediatric nonalcoholic fatty liver disease[J]. J Pediatr Gastroenterol Nutr, 2019, 69( 3): 339- 343. DOI: 10.1097/MPG.0000000000002401. [54] CARRIER P, DEBETTE-GRATIEN M, GIRARD M, et al. Liver illness and psychiatric patients[J]. Hepat Mon, 2016, 16( 12): e41564. DOI: 10.5812/hepatmon.41564. [55] MILLER AH, RAISON CL. The role of inflammation in depression: From evolutionary imperative to modern treatment target[J]. Nat Rev Immunol, 2016, 16( 1): 22- 34. DOI: 10.1038/nri.2015.5. -



 PDF下载 ( 1414 KB)
PDF下载 ( 1414 KB)

 下载:
下载: