求同存异,兼容并济——从国内外慢加急性肝衰竭定义的演变历程统一共识
DOI: 10.12449/JCH241108
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:徐曼曼负责撰写论文;陈煜负责拟定写作思路,指导论文撰写并修改论文。
Unified consensus and evolution of the definition of acute-on-chronic liver failure: Seeking common ground while reserving differences
-
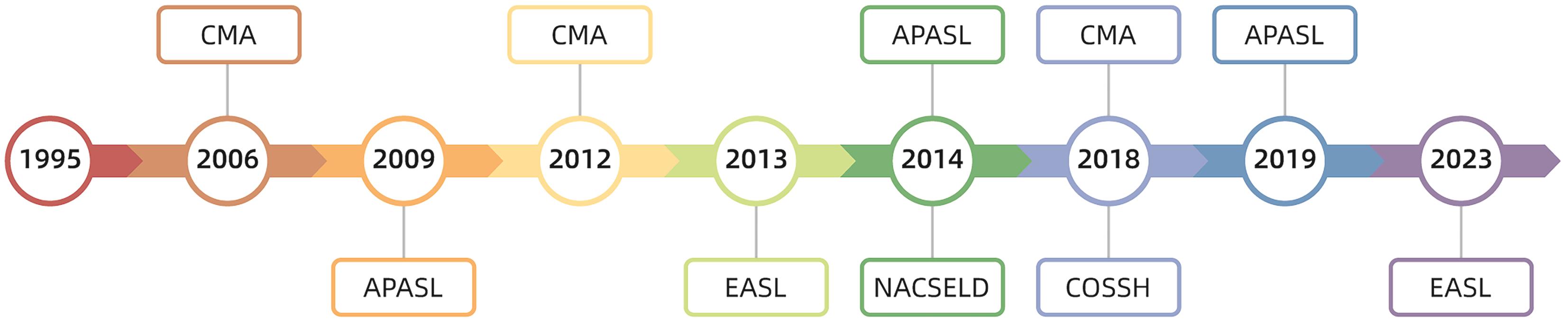
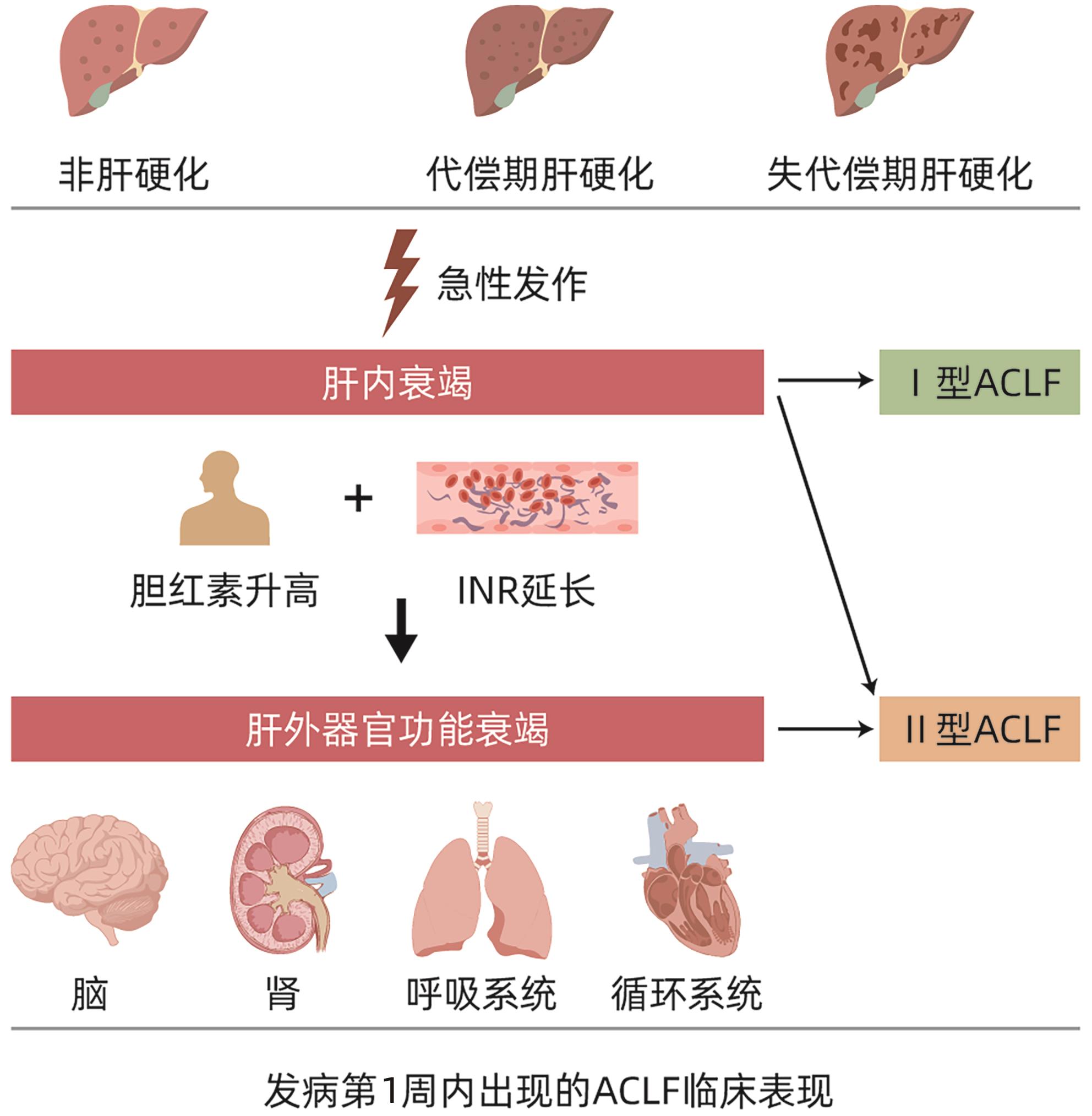
摘要: 在慢加急性肝衰竭(ACLF)这一概念被提出的近30年来,随着对其发病机制、诊断标准、治疗措施等各个方面研究的不断深入,来自全球范围内的相关诊疗共识指南也在不断更新,但ACLF的定义始终未得到统一,定义的不同必然会阻碍诸多治疗手段、预后评分、诊疗意见的推广应用。近年来,肝病学专家们不断提出了统一ACLF定义的方式方法,求同存异,取长补短,最终力求使ACLF的定义趋于一致。Abstract: The concept of acute-on-chronic liver failure (ACLF) has been introduced for nearly 30 years, and with extensive research on its pathogenesis, diagnostic criteria, and treatment strategies, related consensus statements and guidelines have been constantly updated in China and globally; however, there is still a lack of a unified definition of ACLF, and such differences in definition may inevitably hinder the application and implementation of various treatment methods, prognostic scoring systems, and clinical recommendations. In recent years, hepatology experts have continuously proposed methods to unify the definition of ACLF, seeking common ground while reserving differences and drawing on the strengths of various definitions, in order to achieve a more unified definition of ACLF.
-
Key words:
- Acute-on-Chronic Liver Failure /
- Definition /
- Evolution
-
-
[1] OHNISHI H, SUGIHARA J, MORIWAKI H, et al. Acute-on-chronic liver failure[J]. Ryoikibetsu Shokogun Shirizu, 1995( 7): 217- 219. [2] SARIN SK, KUMAR A, ALMEIDA JA, et al. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific association for the study of the liver(APASL)[J]. Hepatol Int, 2009, 3( 1): 269- 282. DOI: 10.1007/s12072-008-9106-x. [3] SARIN SK, KEDARISETTY CK, ABBAS Z, et al. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific Association for the Study of the Liver(APASL) 2014[J]. Hepatol Int, 2014, 8( 4): 453- 471. DOI: 10.1007/s12072-014-9580-2. [4] SARIN SK, CHOUDHURY A, SHARMA MK, et al. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific association for the study of the liver(APASL): An update[J]. Hepatol Int, 2019, 13( 4): 353- 390. DOI: 10.1007/s12072-019-09946-3. [5] JALAN R, SALIBA F, PAVESI M, et al. Development and validation of a prognostic score to predict mortality in patients with acute-on-chronic liver failure[J]. J Hepatol, 2014, 61( 5): 1038- 1047. DOI: 10.1016/j.jhep.2014.06.012. [6] BAJAJ JS, O’LEARY JG, REDDY KR, et al. Survival in infection-related acute-on-chronic liver failure is defined by extrahepatic organ failures[J]. Hepatology, 2014, 60( 1): 250- 256. DOI: 10.1002/hep.27077. [7] WU TZ, LI J, SHAO L, et al. Development of diagnostic criteria and a prognostic score for hepatitis B virus-related acute-on-chronic liver failure[J]. Gut, 2018, 67( 12): 2181- 2191. DOI: 10.1136/gutjnl-2017-314641. [8] KIMMANN M, TREBICKA J. Acute-on-chronic liver failure: Current interventional treatment options and future challenges[J]. J Pers Med, 2023, 13( 7): 1052. DOI: 10.3390/jpm13071052. [9] LI YH, XU Y, WU HM, et al. Umbilical cord-derived mesenchymal stem cell transplantation in hepatitis B virus related acute-on-chronic liver failure treated with plasma exchange and entecavir: A 24-month prospective study[J]. Stem Cell Rev Rep, 2016, 12( 6): 645- 653. DOI: 10.1007/s12015-016-9683-3. [10] WANG HM, YAO WQ, WANG YY, et al. Meta-analysis on last ten years of clinical injection of bone marrow-derived and umbilical cord MSC to reverse cirrhosis or rescue patients with acute-on-chronic liver failure[J]. Stem Cell Res Ther, 2023, 14( 1): 267. DOI: 10.1186/s13287-023-03494-2. [11] SALIBA F, BAÑARES R, LARSEN FS, et al. Artificial liver support in patients with liver failure: A modified DELPHI consensus of international experts[J]. Intensive Care Med, 2022, 48( 10): 1352- 1367. DOI: 10.1007/s00134-022-06802-1. [12] LARSEN FS. Artificial liver support in acute and acute-on-chronic liver failure[J]. Curr Opin Crit Care, 2019, 25( 2): 187- 191. DOI: 10.1097/MCC.0000000000000584. [13] SAHA BK, MAHTAB M AL, AKBAR SMF, et al. Therapeutic implications of granulocyte colony stimulating factor in patients with acute-on-chronic liver failure: Increased survival and containment of liver damage[J]. Hepatol Int, 2017, 11( 6): 540- 546. DOI: 10.1007/s12072-017-9814-1. [14] ENGELMANN C, HERBER A, FRANKE A, et al. Granulocyte-colony stimulating factor(G-CSF) to treat acute-on-chronic liver failure: A multicenter randomized trial(GRAFT study)[J]. J Hepatol, 2021, 75( 6): 1346- 1354. DOI: 10.1016/j.jhep.2021.07.033. [15] PATEL A, WALLING A, KANWAL F, et al. Rates, patterns, and predictors of specialty palliative care consultation among patients with acute-on-chronic liver failure[J]. JHEP Rep, 2023, 6( 2): 100976. DOI: 10.1016/j.jhepr.2023.100976. [16] PERRICONE G, ARTZNER T, de MARTIN E, et al. Intensive care management of acute-on-chronic liver failure[J]. Intensive Care Med, 2023, 49( 8): 903- 921. DOI: 10.1007/s00134-023-07149-x. [17] HE WP, HU JH, ZHAO J, et al. Comparison of four prognostic models and a new Logistic regression model to predict short-term prognosis of acute-on-chronic hepatitis B liver failure[J]. Chin Med J(Engl), 2012, 125( 13): 2272- 2278. [18] JALAN R, YURDAYDIN C, BAJAJ JS, et al. Toward an improved definition of acute-on-chronic liver failure[J]. Gastroenterology, 2014, 147( 1): 4- 10. DOI: 10.1053/j.gastro.2014.05.005. [19] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [20] BAJAJ JS, O’LEARY JG, LAI JC, et al. Acute-on-chronic liver failure clinical guidelines[J]. Am J Gastroenterol, 2022, 117( 2): 225- 252. DOI: 10.14309/ajg.0000000000001595. [21] XU M, CHEN Y. New perspectives in the definition and classification of acute-on-chronic liver failure[J]. Chin Med J(Engl), 2024. DOI: 10.1097/CM9.0000000000003289.[ Online ahead of print]. [22] DONG JL, CHEN Y. Recognition of the clinical classification of acute-on-chronic liver failure: Redefinition from a new perspective of onset manifestations and dynamic outcomes[J]. J Clin Hepatol, 2023, 39( 10): 2277- 2280. DOI: 10.3969/j.issn.1001-5256.2023.10.002.董金玲, 陈煜. 慢加急性肝衰竭临床分型的再认识: 从起病表现和动态转归的新视角重新定义[J]. 临床肝胆病杂志, 2023, 39( 10): 2277- 2280. DOI: 10.3969/j.issn.1001-5256.2023.10.002. [23] XU MM, CHEN Y, ARTRU F. Acute decompensation of cirrhosis versus acute-on-chronic liver failure: What are the clinical implications?[J]. United European Gastroenterol J, 2024, 12( 2): 194- 202. DOI: 10.1002/ueg2.12538. [24] WU Y, DONG JL, XU MM, et al. Acute-on-chronic liver failure: Features and prognosis of a new clinical classification system based on onset manifestations[J]. J Clin Hepatol, 2023, 39( 10): 2375- 2382. DOI: 10.3969/j.issn.1001-5256.2023.10.015.武羽, 董金玲, 徐曼曼, 等. 慢加急性肝衰竭: 基于起病表现的新型临床分型特征及预后分析[J]. 临床肝胆病杂志, 2023, 39( 10): 2375- 2382. DOI: 10.3969/j.issn.1001-5256.2023.10.015. [25] KARVELLAS CJ, BAJAJ JS, KAMATH PS, et al. AASLD Practice Guidance on Acute-on-chronic liver failure and the management of critically ill patients with cirrhosis[J]. Hepatology, 2024, 79( 6): 1463- 1502. DOI: 10.1097/HEP.0000000000000671. [26] KULKARNI AV, SARIN SK. Acute-on-chronic liver failure-steps towards harmonization of the definition![J]. J Hepatol, 2024, 81( 2): 360- 366. DOI: 10.1016/j.jhep.2024.03.036. 期刊类型引用(13)
1. 温芳芳,张龙,王娟. 预后营养指数、血清白蛋白对肝切除术病人术后感染风险的预测价值及护理指导意义. 全科护理. 2025(02): 236-239 .  百度学术
百度学术2. 魏红艳,王远珍,常丽仙,木唤,刘春云,刘立. 原发性肝癌合并腹水患者发生SBP的风险预测分析. 昆明医科大学学报. 2024(03): 133-140 .  百度学术
百度学术3. 魏红艳,王远珍,常丽仙,木唤,刘春云,刘立. 原发性肝癌患者并发自发性腹膜炎临床诊断模型的构建和应用. 现代肿瘤医学. 2024(19): 3718-3725 .  百度学术
百度学术4. 朱明强,杨大帅,熊祥云,裴俊鹏,彭阳,丁佑铭. 肝癌肝切除术后感染风险预测模型的建立与评价. 临床肝胆病杂志. 2023(01): 110-117 .  本站查看
本站查看5. 罗清兰,邓宇伟,曾涛. 原发性肝癌术前中性粒细胞/淋巴细胞比值、血小板/淋巴细胞比值和甲胎蛋白对预后的评估分析. 当代医学. 2022(19): 18-21 .  百度学术
百度学术6. 付先锋,晏燕. 肝动脉介入栓塞治疗的肝癌患者预后与血清胆碱酯酶、钠水平的关系分析. 检验医学与临床. 2022(24): 3417-3420 .  百度学术
百度学术7. 曾桥. 腹腔镜手术治疗肝癌的分析. 当代医学. 2021(04): 96-98 .  百度学术
百度学术8. 黄旦华. 多项肿瘤标志物联合检测在肝癌中的诊断效能. 医疗装备. 2021(11): 52-53 .  百度学术
百度学术9. 袁维,孙克伟,陈斌,朱文芳,银思涵. 56例中晚期原发性肝癌死亡患者的临床分析. 中西医结合肝病杂志. 2021(08): 707-711 .  百度学术
百度学术10. 马冰,白黎,赵艳,海丹丹,李花花. 原发性肝癌TACE术后发生感染性并发症的影响因素研究. 实用癌症杂志. 2021(12): 2033-2035 .  百度学术
百度学术11. 王益卓,刘唯佳,卢兵,黄其密,唐德奉. 原发性肝癌合并肺部感染58例临床特征分析. 中华肺部疾病杂志(电子版). 2020(01): 83-84 .  百度学术
百度学术12. 刘娟. 以坚强概念为基础的心理干预对原发性肝癌合并抑郁病人症状改善、心理状态及生命质量的影响. 全科护理. 2020(28): 3834-3837 .  百度学术
百度学术13. 叶颖剑,刘波,陈伟,李琼霞. 血清AFP阴性的肝细胞癌患者预后及分期系统分析. 临床肝胆病杂志. 2019(03): 535-541 .  本站查看
本站查看其他类型引用(4)
-




 PDF下载 ( 1061 KB)
PDF下载 ( 1061 KB)

 下载:
下载:

 百度学术
百度学术

