栀子大黄汤在酒精性肝病小鼠模型中的保护作用
DOI: 10.3969/j.issn.1001-5256.2023.12.019
伦理学声明:本研究方案于2023年2月9日经由上海南方模式生物研究中心伦理委员会审批,批号:2023-0003,符合实验室动物管理与使用准则。
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:侯逸文负责课题设计,资料分析,撰写论文;张荣杰、纪龙珊、李茜参与收集数据,修改论文;高月求、李曼负责拟定写作思路,指导撰写文章并最后定稿。
Protective effect of Zhizi Dahuang decoction in a mouse model of alcoholic liver disease
-
摘要:
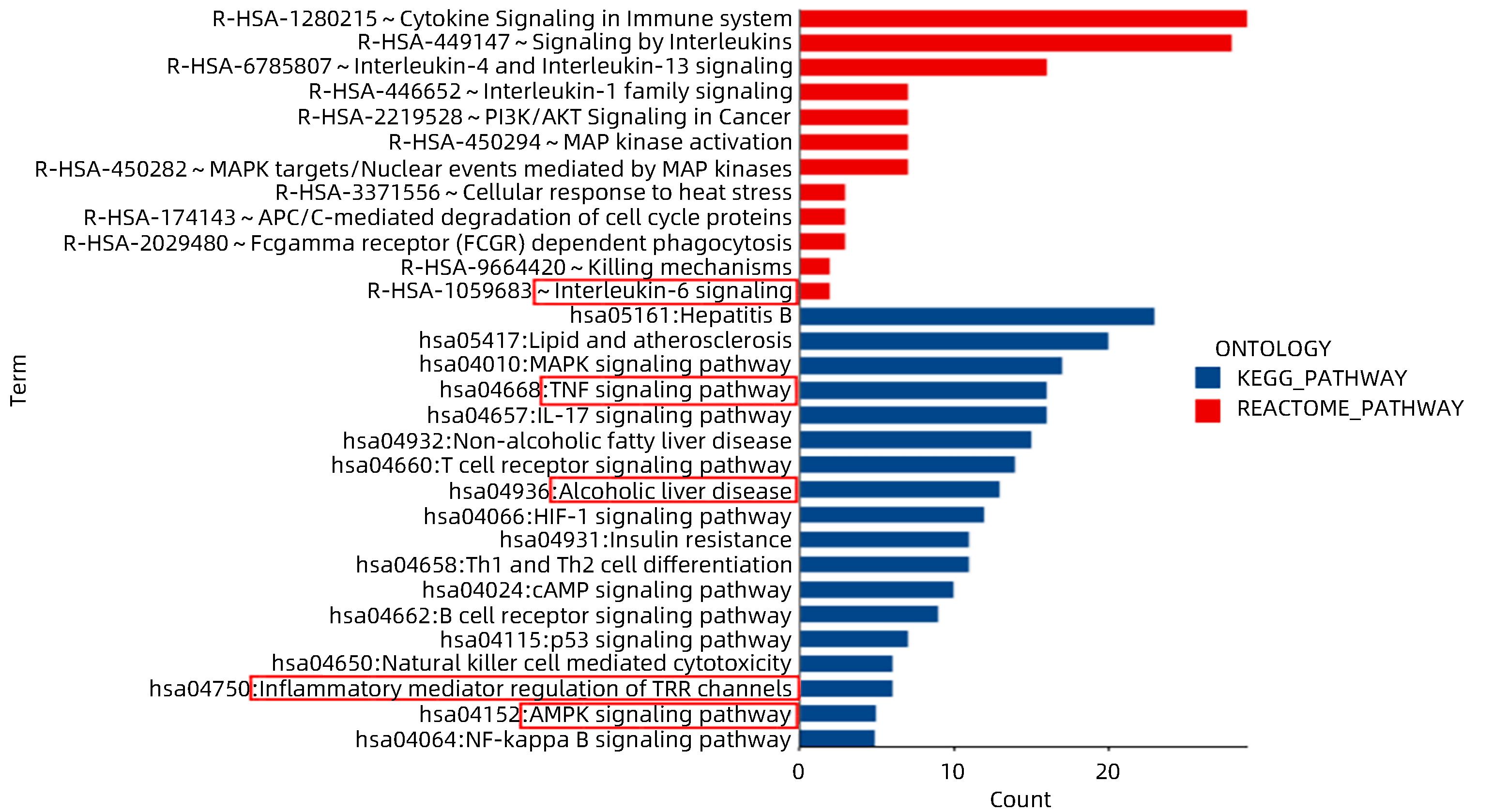
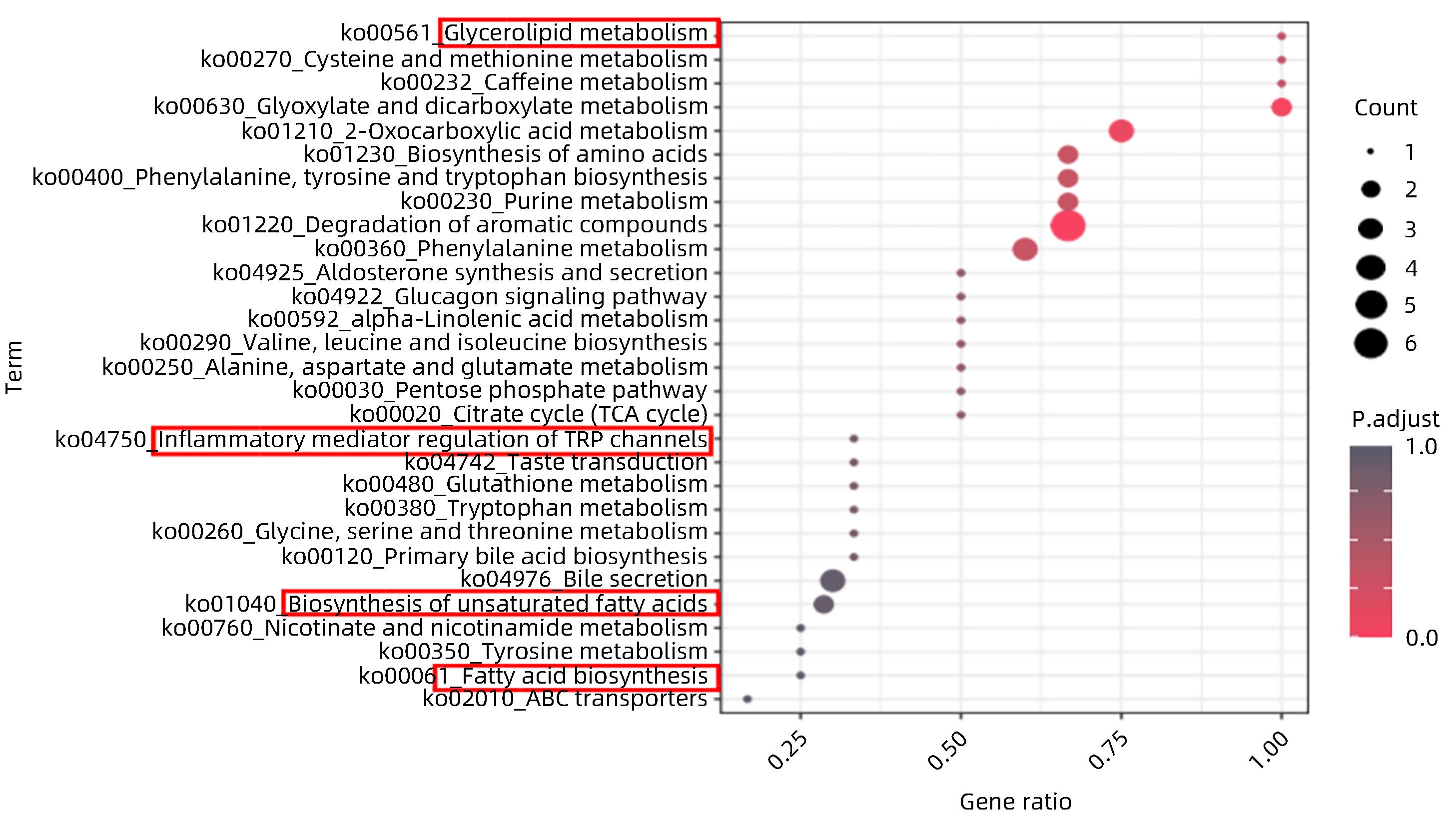
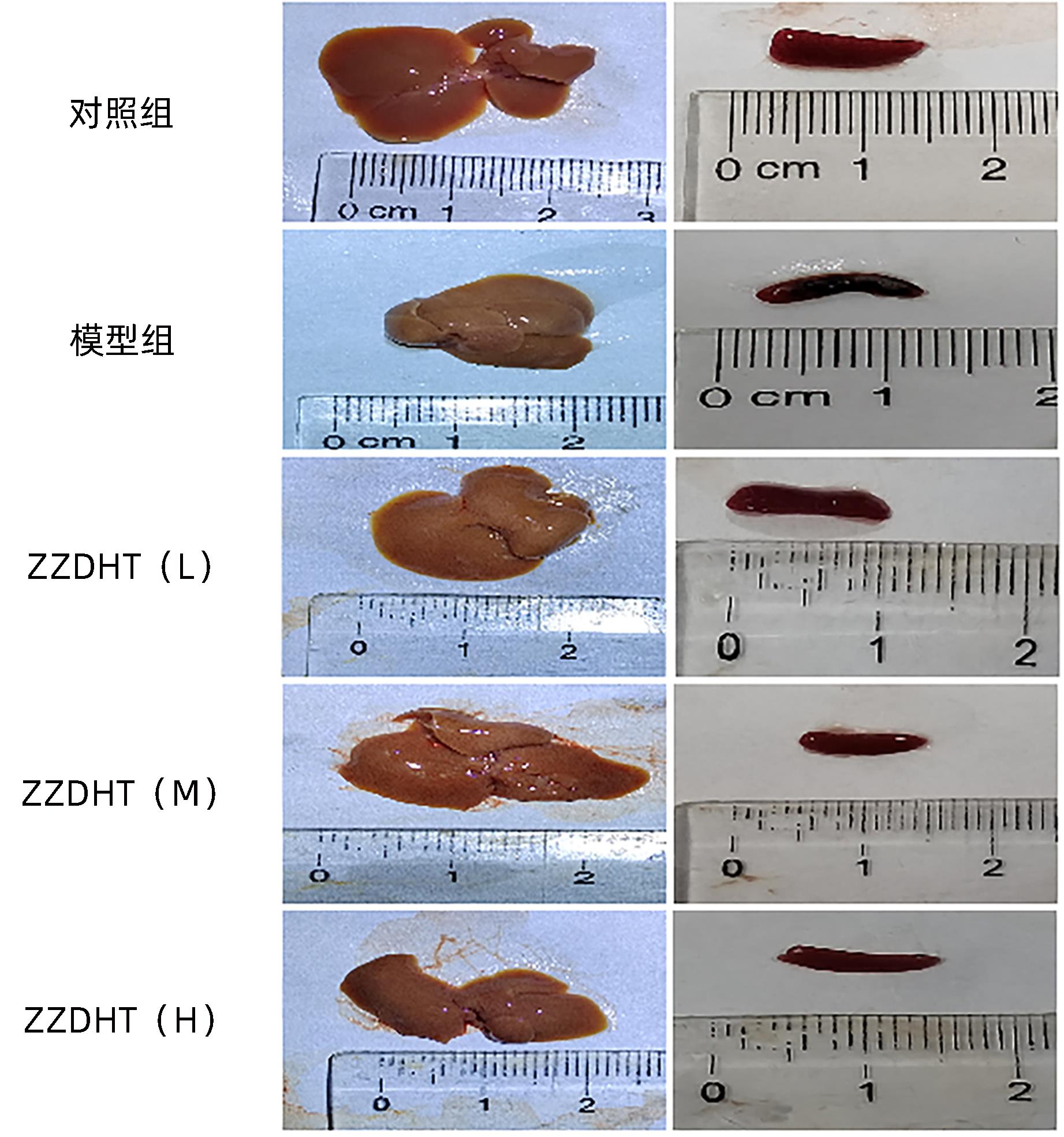
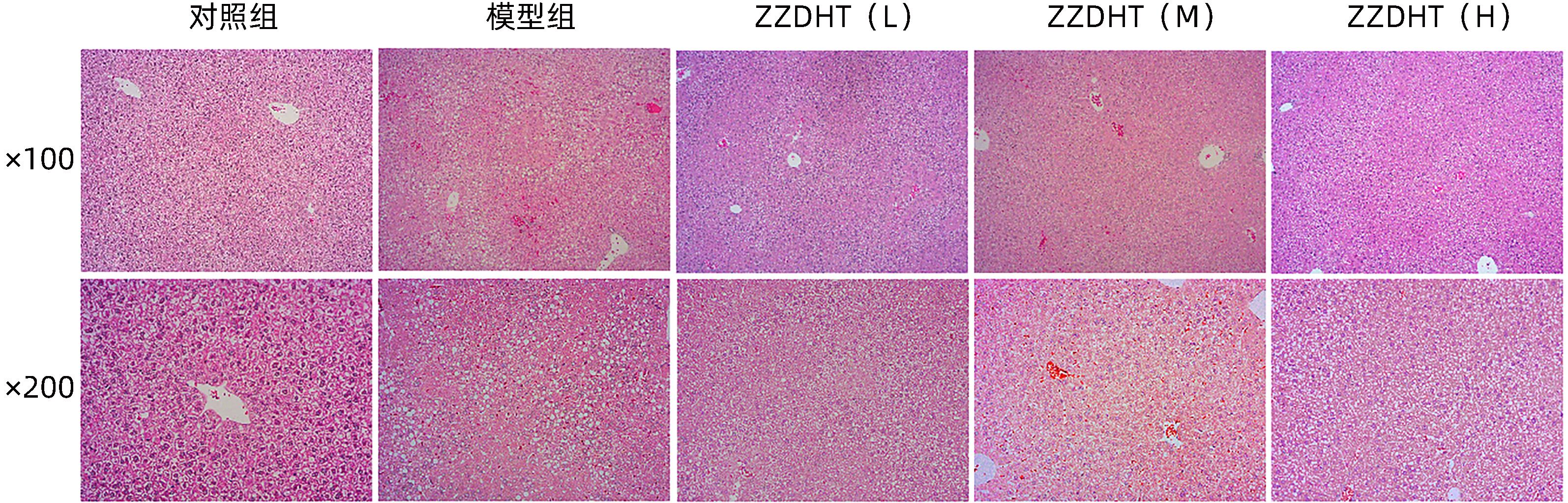
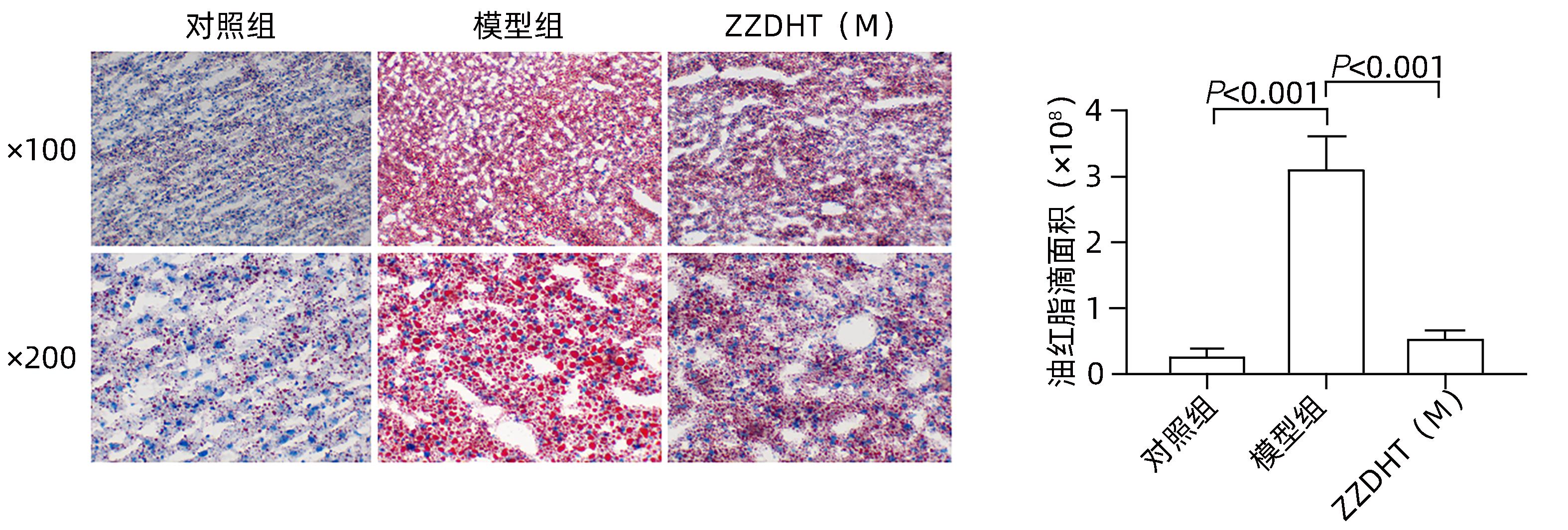
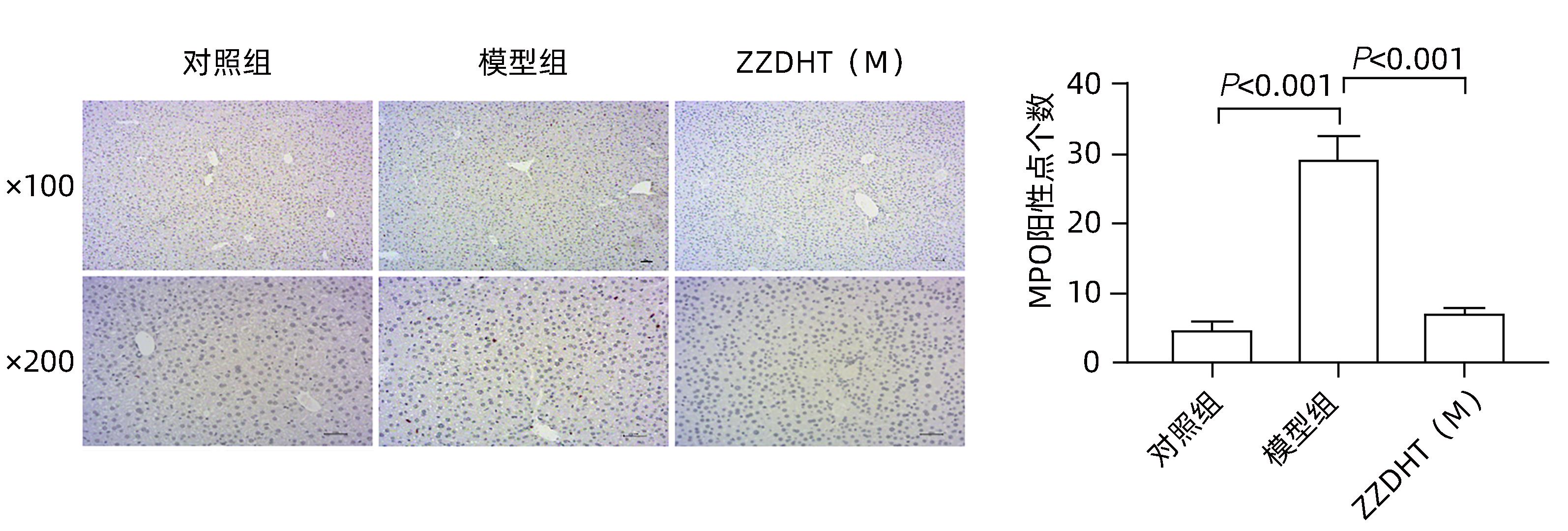
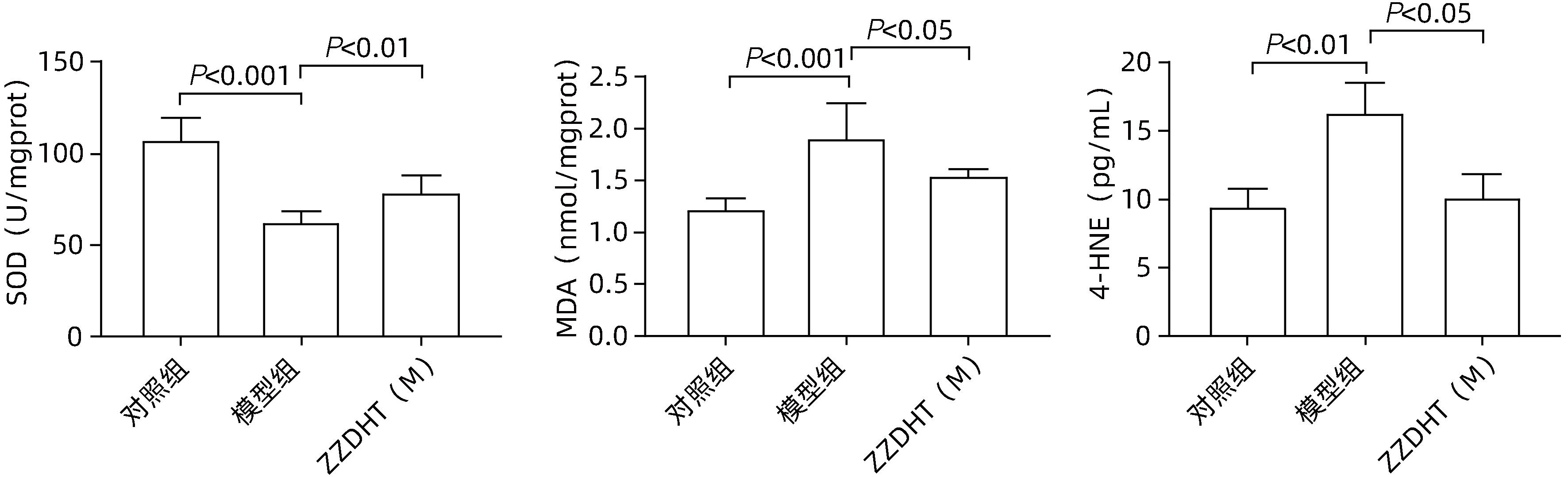
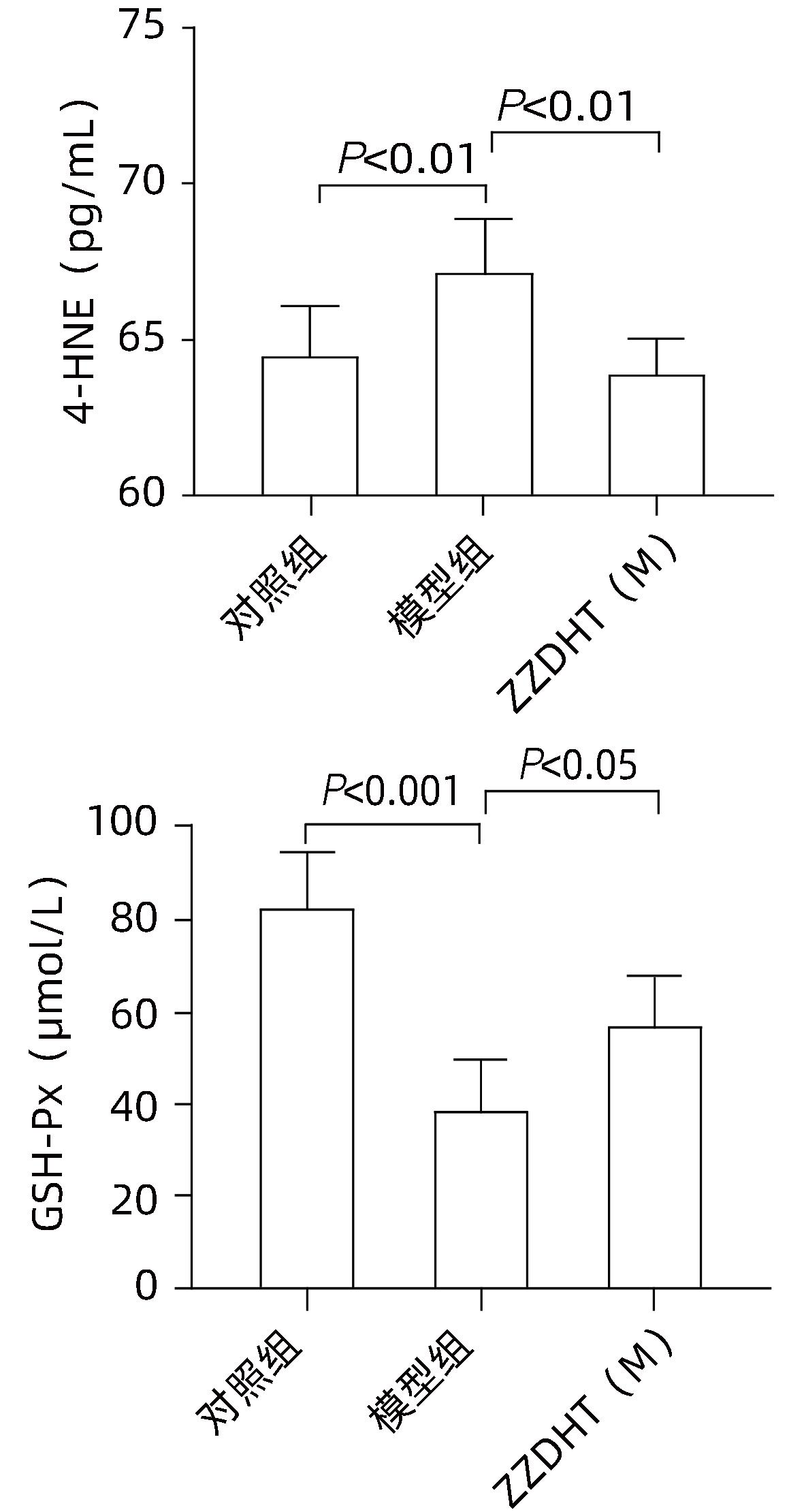
目的 阐明栀子大黄汤(ZZDHT)通过改善肝脏中性粒细胞的氧化应激治疗酒精性肝病(ALD)的作用。 方法 (1)运用网络药理学方法筛选ZZDHT的化学成分及其对应的作用靶点,分析其治疗ALD的潜在靶点和相关功能通路。(2)使用非靶代谢组学技术检测ZZDHT在小鼠血清和肝脏中代谢物变化情况,配制两倍中剂量浓度的ZZDHT予以灌胃,分别于灌胃后6个时间点(10 min、30 min、1 h、2 h、4 h、6 h)取小鼠血清和肝组织,混合进行后续质谱分析(用药组,18只)。对照组(18只)予以等量生理盐水灌胃。使用超高液相色谱技术,快速分离和鉴定ZZDHT在血清和肝组织中的代谢物,对ZZDHT有效成分进行验证。(3)8周龄C57BL/6J雄性小鼠随机均分为对照组、模型组、ZZDHT低剂量[ZZDHT(L)]组、ZZDHT中剂量[ZZDHT(M)]组、ZZDHT高剂量[ZZDHT(H)]组(每组10只),除对照组外,其余各组建立ALD小鼠模型(NIAAA模型小鼠),用药组在造模的同时分别进行ZZDHT低、中、高剂量的灌胃,对照组和模型组使用等量生理盐水灌胃。检测血清ALT、AST和TG的表达水平;PCR测得肝脏相关炎性、氧化应激和中性粒细胞指标基因表达水平;ELISA法测定血清中炎症和氧化应激相关指标;SOD、GSH-Px、MDA检测肝脏氧化应激水平;通过HE染色、MPO染色以及油红染色观察小鼠肝组织损伤、中性粒细胞浸润及脂质沉积情况。计量资料多组间比较采用单因素方差分析,进一步两两比较采用LSD-t检验。 结果 (1)通过筛选共得到ZZDHT的53个有效活性成分,227个靶点基因,ALD的靶点基因共8 685个,两者共同的靶点基因222个。核心通路包括interleukin-6 signaling、TNF signaling pathway等。(2)非靶代谢分析得出ZZDHT在小鼠肝脏中代谢物有225个,在血清中代谢物有227个,共同代谢物有126个。分析得到肝脏代谢物核心通路有glycerolipid metabolism、inflammatory mediator regulation of TRP channels等,血清代谢物核心通路有AMPK signaling pathway、Oxidative phosphorylation等,均与氧化应激和炎症相关通路有关。(3)与模型组相比,ZZDHT(L)、ZZDHT(M)、ZZDHT(H)组小鼠血清ALT、AST和TG水平均明显降低(P值均<0.05),ZZDHT(M)组小鼠肝组织Ly6g、Ncf1、Ncf2、IL-6、TNF-α、IL-1β、MDA、4-HNE、Gp91、P22水平均明显降低(P值均<0.05),SOD水平明显升高(P<0.05),ZZDHT(M)组小鼠血清4-HNE水平明显降低、GSH-Px水平明显升高(P值均<0.05)。ZZDHT(M)组小鼠肝脏中脂肪沉积和中性粒细胞浸润均明显改善(P值均<0.05)。 结论 ZZDHT可显著改善NIAAA模型小鼠的氧化应激和炎症反应。 Abstract:Objective To investigate the effect of Zhizi Dahuang decoction (ZZDHT) in the treatment of alcoholic liver disease (ALD) by improving oxidative stress in hepatic neutrophils. Methods Network pharmacology was used to obtain the chemical components of ZZDHT and their corresponding action targets and analyze the potential targets and functional pathways of ZZDHT in the treatment of ALD. The non-target metabolomics technology was used to observe the changes in the metabolites of ZZDHT in mouse serum and liver. The mice were given ZZDHT at a dose twice as much as the middle dose concentration by gavage, and serum and liver samples were collected at six time points after gavage (10 minutes, 30 minutes, 1 hour, 2 hours, 4 hours, and 6 hours) and were then mixed for mass spectrometry (administration group with 18 mice), while the 18 mice in the control group were given an equal volume of normal saline by gavage. Ultra-performance liquid chromatography was used for rapid isolation and identification of the metabolites of ZZDHT in serum and liver tissue, and the effective constituents of ZZDHT were validated. Male C57BL/6J mice, aged 8 weeks, were randomly and equally divided into control group, model group, and low-, middle-, and high-dose ZZDHT groups, with 10 mice in each group. All mice except those in the control group were used to establish a mouse model of ALD (NIAAA model mice), and at the same time, the mice in the administration groups were given low-, middle-, and high-dose ZZDHT by gavage, while those in the control group and the model group were given an equal volume of normal saline by gavage. The serum levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), and triglyceride (TG) were measured; PCR was used to measure the gene expression levels of related inflammation, oxidative stress, and neutrophil indicators in the liver; ELISA was used to measure the levels of related inflammation and oxidative stress indicators in serum; superoxide dismutase (SOD), glutathione peroxidase (GSH-Px), and malondialdehyde (MDA) were measured to observe the level of oxidative stress in the liver; HE staining, myeloperoxidase staining, and oil red staining were used to observe liver injury, neutrophil infiltration, and lipid deposition. A one-way analysis of variance was used for comparison of continuous data between multiple groups, and the least significant difference t-test was used for further comparison between two groups. Results A total of 53 active components and 227 target genes were obtained for ZZDHT, and there were 8685 target genes of ALD, resulting in 222 common target genes between these two groups of genes. Core pathways included the interleukin-6 signaling pathway and the TNF signaling pathway. The non-targeted metabolic analysis of ZZDHT obtained 225 metabolites in mouse liver and 227 metabolites in serum, among which there were 126 common metabolites. The core pathways of liver metabolites included glycerolipid metabolism and inflammatory mediator regulation of TRP channels, and the core pathways of serum metabolites included the AMPK signaling pathway and oxidative phosphorylation, all of which were associated with oxidative stress- and inflammation-related pathways. Compared with the model group, the low-, middle-, and high-dose ZZDHT groups had significant reductions in the serum levels of ALT, AST, and TG (all P<0.05), and the middle-dose ZZDHT group had significant reductions in the levels of Ly6g, Ncf1, Ncf2, IL-6, TNF-α, IL-1β, MDA, 4-HNE, Gp91, and P22 in the liver (all P<0.05), a significant increase in the level of SOD (P<0.05), a significant reduction in the serum level of 4-HNE (P<0.05), and a significant increase in the level of GSH-Px (P<0.05). There were significant improvements in fat deposition and neutrophil infiltration in the liver of mice in the middle-dose ZZDHT group (both P<0.05). Conclusion ZZDHT significantly reduces oxidative stress and inflammatory response in NIAAA model mice. -
Key words:
- Liver Diseases, Alcoholic /
- Zhizi Dahuang Decoction /
- Oxidative Stress /
- Models, Animal
-
-
[1] SEITZ HK, BATALLER R, CORTEZ-PINTO H, et al. Alcoholic liver disease[J]. Nat Rev Dis Primers, 2018, 4( 1): 16. DOI: 10.1038/s41572-018-0014-7. [2] SINGAL AK, BATALLER R, AHN J, et al. ACG clinical guideline: Alcoholic liver disease[J]. Am J Gastroenterol, 2018, 113( 2): 175- 194. DOI: 10.1038/ajg.2017.469. [3] OTERO SANCHEZ L, KARAKIKE E, NJIMI H, et al. Clinical course and risk factors for infection in severe forms of alcohol-associated liver disease[J]. Hepatology, 2021, 74( 5): 2714- 2724. DOI: 10.1002/hep.31984. [4] ASRANI SK, MELLINGER J, ARAB JP, et al. Reducing the global burden of alcohol-associated liver disease: A blueprint for action[J]. Hepatology, 2021, 73( 5): 2039- 2050. DOI: 10.1002/hep.31583. [5] ZHAO KL. Understanding alcoholic liver disease[J]. Hepatologist, 2019, 3: 45. DOI: 10.3969/j.issn.2095-5160.2019.03.012.赵康路. 认识酒精肝[J]. 肝博士, 2019,( 3): 45. DOI: 10.3969/j.issn.2095-5160.2019.03.012. [6] AVILA MA, DUFOUR JF, GERBES AL, et al. Recent advances in alcohol-related liver disease(ALD): Summary of a Gut round table meeting[J]. Gut, 2020, 69( 4): 764- 780. DOI: 10.1136/gutjnl-2019-319720. [7] WU Y, LI YR, YANG JZ, et al. Research advances in the pathogenesis of alcoholic liver disease[J]. J Clin Hepatol, 2020, 36( 12): 2822- 2825. DOI: 10.3969/j.issn.1001-5256.2020.12.038.吴亚, 李艳茹, 杨寄镯, 等. 酒精性肝病发病机制研究现状[J]. 临床肝胆病杂志, 2020, 36( 12): 2822- 2825. DOI: 10.3969/j.issn.1001-5256.2020.12.038. [8] GUSTOT T, FERNANDEZ J, SZABO G, et al. Sepsis in alcohol-related liver disease[J]. J Hepatol, 2017, 67( 5): 1031- 1050. DOI: 10.1016/j.jhep.2017.06.013. [9] QIU P, LI X, KONG D, ZENG SJ, ZU YW, WANG Y, PAN SH New progress in the study of the pathogenesis of alcoholic liver disease[J] Chinese Pharmacological Bulletin, 2014, 02: 160- 163.邱萍, 李相, 孔德松, 曾善静, 祖亚威, 王允, 潘苏华. 酒精性肝病发病机制研究的新进展[J]. 中国药理学通报, 2014, 02: 160- 163. [10] LUO PP, ZHENG M, ZHANG R, et al. S-Allylmercaptocysteine improves alcoholic liver disease partly through a direct modulation of insulin receptor signaling[J]. Acta Pharm Sin B, 2021, 11( 3): 668- 679. DOI: 10.1016/j.apsb.2020.11.006. [11] LI M, HE Y, ZHOU Z, et al. microRNA-223 ameliorates alcoholic liver injury by inhibiting the IL-6-p47phox-oxidative stress pathway in neutrophils[J]. Gut, 2017, 66( 4): 705- 715. DOI: 10.1136/gutjnl-2016-311861. [12] LIANG XX, YUAN L. Research progress on protective mechanism of traditional Chinese medicine treatment on alcoholic liver injury[J/CD]. Mod Med Heath Res Electron J, 2021, 5( 8): 135- 138.梁晓晓, 袁林. 中药治疗对酒精性肝损伤的保护机制研究进展[J/CD]. 现代医学与健康研究电子杂志, 2021, 5( 8): 135- 138. [13] ZHANG JR. Discussion on the Syndrome and Treatment of Jaundice in“Synopsis of the Golden Chamber”//[C]. Zhongjing Theory Branch of the Chinese Society of Traditional Chinese Medicine. Proceedings of the 22nd National Zhongjing Theory Academic Annual Conference. 2014: 5.张建荣.《金匮要略》黄疸病证治探讨//[C]. 中华中医药学会仲景学说分会. 全国第二十二次仲景学说学术年会论文集. 2014: 5. [14] NIE JJ, WANG X, TANG YP. The progress of alcoholic liver disease treated with combined therapy of traditional Chinese and western medicine[J]. Henan Tradit Chin Med, 2016, 36( 4): 738- 740. DOI: 10.16367/j.issn.1003-5028.2016.04.0316.聂晶晶, 王骁, 唐艳萍. 酒精性肝病的中西医结合治疗进展[J]. 河南中医, 2016, 36( 4): 738- 740. DOI: 10.16367/j.issn.1003-5028.2016.04.0316. [15] OUYANG HT. Literature research on the origin and development of Zhongjing’s alcoholic jaundice treatment based on syndrome differentiation before Qing Dynasty[D]. Beijing: Beijing University of Chinese Medicine, 2005.欧阳绘天. 仲景酒疸辨证论治源流与发展的清以前文献研究[D]. 北京: 北京中医药大学, 2005. [16] YANG ZF, LI XY, ZHOU BZ, et al. Protective effect of Zhi Zi Da Huang Tang on rats with alcoholic fatty liver[J]. J Jilin Univ Med Ed, 2017, 43( 3): 555- 560, 669. DOI: 10.13481/j.1671-587x.20170318.杨战锋, 李晓勇, 周百中, 等. 栀子大黄汤对酒精性脂肪肝大鼠的保护作用[J]. 吉林大学学报(医学版), 2017, 43( 3): 555- 560, 669. DOI: 10.13481/j.1671-587x.20170318. [17] BERTOLA A, MATHEWS S, KI SH, et al. Mouse model of chronic and binge ethanol feeding(the NIAAA model)[J]. Nat Protoc, 2013, 8( 3): 627- 637. DOI: 10.1038/nprot.2013.032. [18] GAO B, CHANG BX, XU MJ. Mouse model of chronic plus binge ethanol feeding(NIAAA model or Gao-binge model)[J]. Infect Dis Inf, 2013, 26( 5): 307- 311.高斌, 常彬霞, 徐明江. 慢性酒精喂养加急性酒精灌胃的酒精性肝病小鼠模型(NIAAA模型或Gao-Binge模型)[J]. 传染病信息, 2013, 26( 5): 307- 311. [19] YI XK, DU YC, QIAN BL, et al. Protective effect of tanshinone Ⅰ in a mouse model of hepatic ischemia-reperfusion injury[J]. J Clin Hepatol, 2021, 37( 1): 105- 109. DOI: 10.3969/j.issn.1001-5256.2021.01.021.易小康, 杜毅超, 钱保林, 等. 丹参酮Ⅰ在肝缺血再灌注损伤小鼠模型中的保护作用[J]. 临床肝胆病杂志, 2021, 37( 1): 105- 109. DOI: 10.3969/j.issn.1001-5256.2021.01.021. [20] DENG DY, XIA YF, ZHAO L. Effect of the TCM hot compress therapy on the gastrointestinal function recovery and serum inflammatory factors in patients undergoing colorectal surgery[J]. J Changchun Univ Chin Med, 2021, 37( 6): 1329- 1332. DOI: 10.13463/j.cnki.cczyy.2021.06.040.邓大一, 夏玉峰, 赵林. 木香大黄散热奄包对结直肠手术患者胃肠功能的恢复效果及血清炎性因子的影响[J]. 长春中医药大学学报, 2021, 37( 6): 1329- 1332. DOI: 10.13463/j.cnki.cczyy.2021.06.040. [21] XIAO TP, WANG MF, AI BC. Medication of four-side syndrome of damp-heat jaundice in synopsis of the golden chamber from Shennong herbal classic[J]. Guangming J Chin Med, 2022, 37( 9): 1540- 1542. DOI: 10.3969/j.issn.1003-8914.2022.09.012.肖肽平, 王曼菲, 艾碧琛. 从《神农本草经》看《金匮要略》湿热黄疸四方证之用药[J]. 光明中医, 2022, 37( 9): 1540- 1542. DOI: 10.3969/j.issn.1003-8914.2022.09.012. [22] CHU JY, YAN R, WANG S, et al. Sinapic acid reduces oxidative stress and pyroptosis via inhibition of BRD4 in alcoholic liver disease[J]. Front Pharmacol, 2021, 12: 668708. DOI: 10.3389/fphar.2021.668708. [23] LI HM, HUANG QA, TANG F, et al. Altered NCF2, NOX2 mRNA expression levels in peripheral blood mononuclear cells of pulmonary tuberculosis patients[J]. Int J Gen Med, 2021, 14: 9203- 9209. DOI: 10.2147/ijgm.s339194. [24] YU HH, YANG YH, CHIANG BL. Chronic granulomatous disease: A comprehensive review[J]. Clin Rev Allergy Immunol, 2021, 61( 2): 101- 113. DOI: 10.1007/s12016-020-08800-x. [25] KIM HG, HUANG MH, XIN Y, et al. The epigenetic regulator SIRT6 protects the liver from alcohol-induced tissue injury by reducing oxidative stress in mice[J]. J Hepatol, 2019, 71( 5): 960- 969. DOI: 10.1016/j.jhep.2019.06.019. [26] CENI E, MELLO T, GALLI A. Pathogenesis of alcoholic liver disease: Role of oxidative metabolism[J]. World J Gastroenterol, 2014, 20( 47): 17756- 17772. DOI: 10.3748/wjg.v20.i47.17756. [27] SUN J, FU JQ, LI L, et al. Nrf2 in alcoholic liver disease[J]. Toxicol Appl Pharmacol, 2018, 357: 62- 69. DOI: 10.1016/j.taap.2018.08.019. [28] GUTHRIE LA, MCPHAIL LC, HENSON PM, et al. Priming of neutrophils for enhanced release of oxygen metabolites by bacterial lipopolysaccharide. Evidence for increased activity of the superoxide-producing enzyme[J]. J Exp Med, 1984, 160( 6): 1656- 1671. DOI: 10.1084/jem.160.6.1656. [29] YING WH. NAD+/NADH and NADP+/NADPH in cellular functions and cell death: Regulation and biological consequences[J]. Antioxid Redox Signal, 2008, 10( 2): 179- 206. DOI: 10.1089/ars.2007.1672. [30] LIU TT, LIU JK, LI SL, et al. Advances in the mechanism of action of silent information regulator 1 in alcoholic liver disease and related pharma-ceutical studies[J]. J Clin Hepatol, 2022, 38( 12): 2841- 2845. DOI: 10.3969/j.issn.1001-5256.2022.12.030.刘甜恬, 刘江凯, 李素领, 等. 沉默调节蛋白1在酒精性肝病中的作用机制及相关药物研究进展[J]. 临床肝胆病杂志, 2022, 38( 12): 2841- 2845. DOI: 10.3969/j.issn.1001-5256.2022.12.030. [31] LI Q, TAN JX, HE Y, et al. Atractylenolide III ameliorates non-alcoholic fatty liver disease by activating hepatic adiponectin receptor 1-mediated AMPK pathway[J]. Int J Biol Sci, 2022, 18( 4): 1594- 1611. DOI: 10.7150/ijbs.68873. [32] HYUN J, HAN J, LEE CB, et al. Pathophysiological aspects of alcohol metabolism in the liver[J]. Int J Mol Sci, 2021, 22( 11): 5717. DOI: 10.3390/ijms22115717. [33] QUAN H, JIANG YY. Role of interleukin-1β in the pathogenesis of alcoholic liver disease[J]. J Clin Hepatol, 2021, 37( 5): 1226- 1228. DOI: 10.3969/j.issn.1001-5256.2021.05.053.全卉, 江宇泳. IL-1β在酒精性肝病发病机制中的作用[J]. 临床肝胆病杂志, 2021, 37( 5): 1226- 1228. DOI: 10.3969/j.issn.1001-5256.2021.05.053. -
 栀子大黄汤在酒精性肝病小鼠模型中的保护作用.pdf
栀子大黄汤在酒精性肝病小鼠模型中的保护作用.pdf

-



 PDF下载 ( 3331 KB)
PDF下载 ( 3331 KB)


 下载:
下载: