细菌性肝脓肿并发脓毒症的危险因素及列线图构建
DOI: 10.12449/JCH250621
Risk factors for pyogenic liver abscess comorbid with sepsis and construction of a nomogram prediction model
-
摘要:
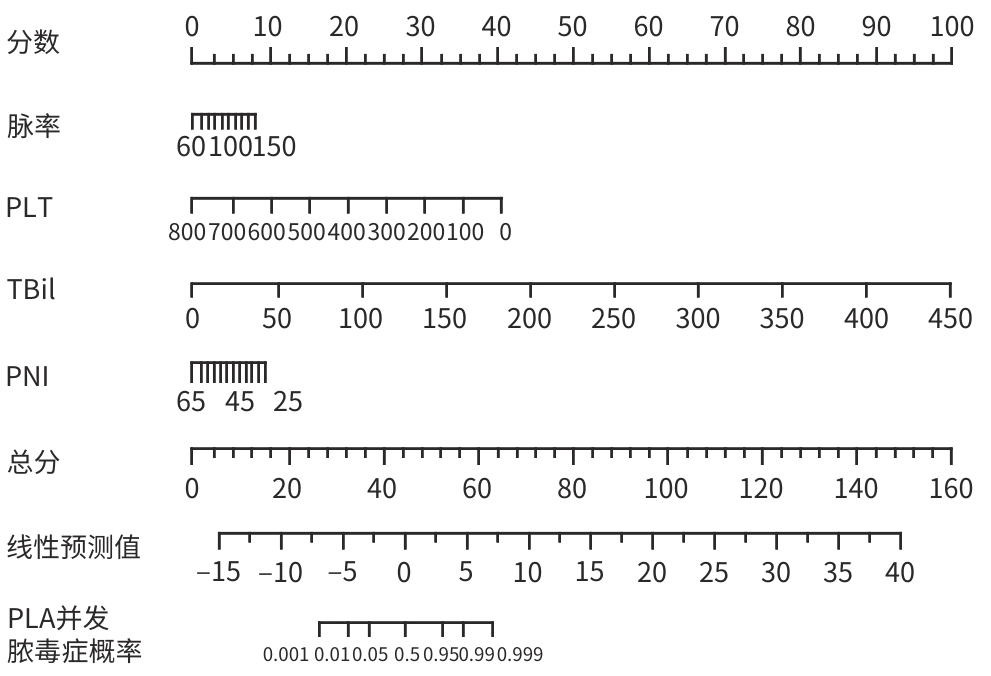
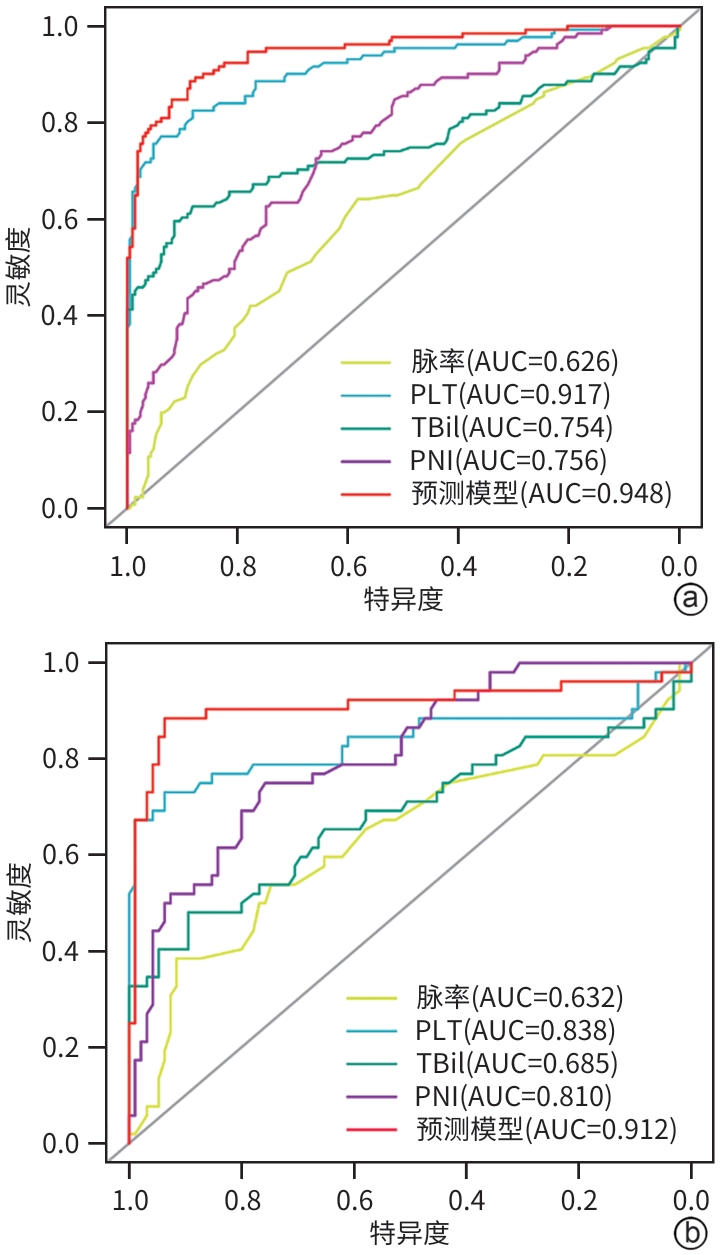
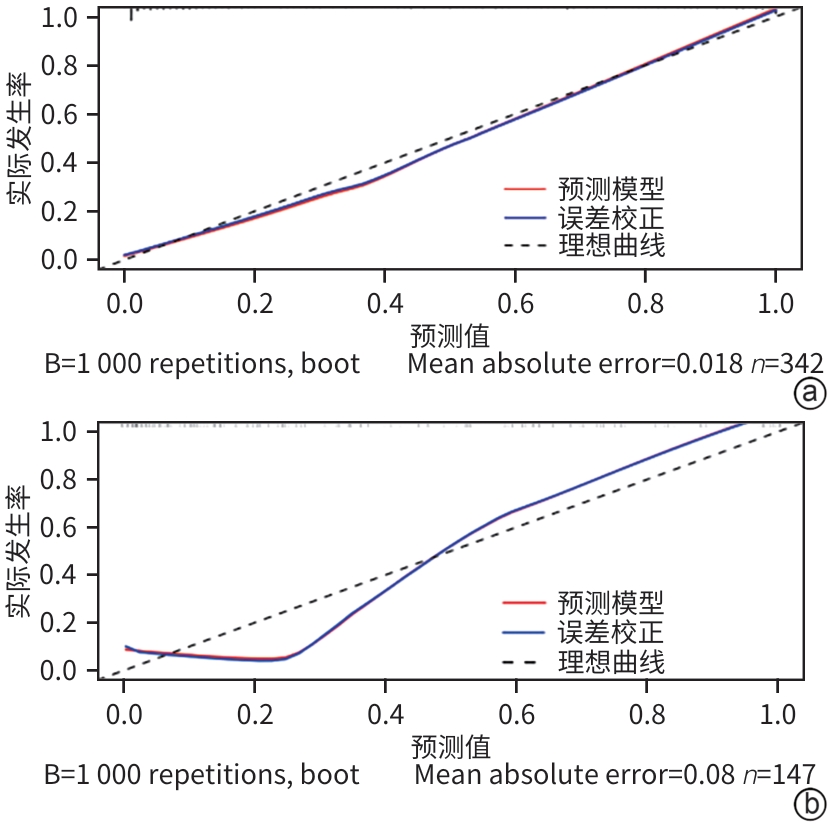
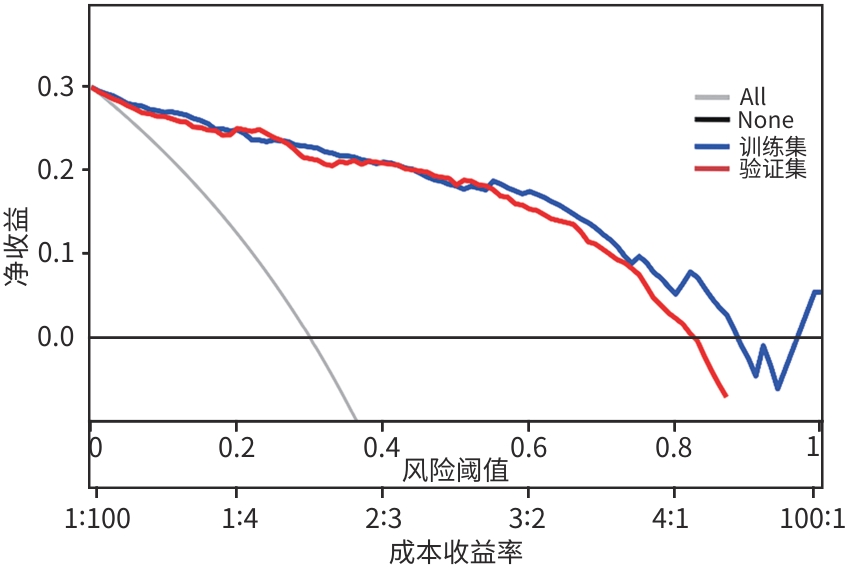
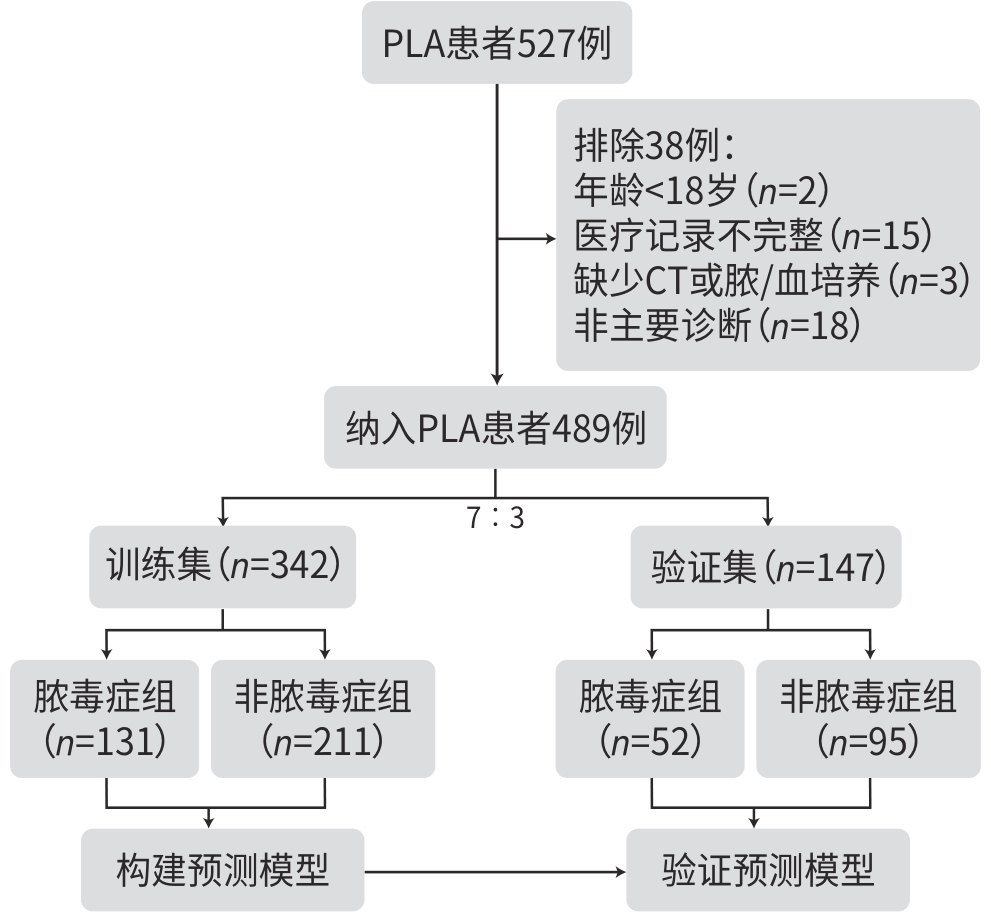
目的 通过分析细菌性肝脓肿(PLA)并发脓毒症的临床特征,探讨PLA并发脓毒症的危险因素,并构建预测模型。 方法 回顾性分析2019年1月—2023年12月于徐州医科大学附属医院住院诊断为PLA的489例患者,根据是否并发脓毒症,分为脓毒症组(n=306)和非脓毒症组(n=183)。收集患者一般资料、实验室检查指标及结局指标。进一步将患者按7∶3的比例随机分为训练集342例和验证集147例,训练集用于筛选变量和构建模型,验证集用于测试模型性能。采用LASSO回归进行变量筛选,并进一步行多因素Logistic回归分析,建立预测模型,绘制列线图。使用校准图、受试者操作特征曲线(ROC曲线)和决策曲线分析对模型进行评估,并进行内部验证。对于符合正态分布的计量资料2组间比较采用成组t检验;非正态分布的计量资料2组间比较采用Mann-Whitney U检验。分类变量采用χ2检验分析组间差异。 结果 脓毒症组和非脓毒症组的脉率、平均动脉压、症状持续时间、合并肝硬化、合并恶性肿瘤、白细胞计数、中性粒细胞计数、淋巴细胞计数、血小板计数(PLT)、活化部分凝血酶原时间、纤维蛋白原、CRP、AST、ALT、Alb、TBil、肌酐、钾、预后营养指数(PNI)差异均有统计学意义(P值均<0.05)。在训练集中,通过LASSO回归分析,筛选出脉率、PLT、TBil、PNI 4个预测因子,进一步多因素Logistic回归分析显示,脉率(OR=1.033,95%CI:1.006~1.061,P=0.018)、PLT(OR=0.981,95%CI:0.975~0.987,P<0.001)、TBil(OR=1.086,95%CI:1.053~1.125,P<0.001)和PNI(OR=0.935,95%CI:0.882~0.988,P=0.019)是PLA患者发生脓毒症风险的独立影响因素,据此构建的模型表现出良好的预测能力,在训练集中模型的ROC曲线下面积为0.948(95%CI:0.923~0.973),在验证集中模型的ROC曲线下面积为0.912(95%CI:0.848~0.976)。决策曲线分析结果显示, 在阈值概率0.3~0.9范围内模型具有较好的净获益。 结论 采用脉率、PLT、TBil、PNI构建的预测模型及列线图,能较好预测PLA发生脓毒症的风险,具有临床价值。 Abstract:Objective To investigate the risk factors for pyogenic liver abscess (PLA) comorbid with sepsis by analyzing clinical features, and to construct a predictive model. Methods A retrospective analysis was performed for 489 patients who were hospitalized and diagnosed with PLA in The Affiliated Hospital of Xuzhou Medical University from January 2019 to December 2023, and according to the presence or absence of sepsis, they were divided into sepsis group with 306 patients and non-sepsis group with 183 patients. Related data were collected, including general information, laboratory markers, and outcome measures. The patients were further divided into a training set of 342 patients and a validation set of 147 patients at a ratio of 7∶3, and the training set was used for screening of variables and construction of a predictive model, while the validation set was used to test the performance of the model. An LASSO regression analysis was used for the screening of variables, and a multivariate Logistic regression analysis was used to construct the predictive model and plot a nomogram. The calibration curve, the receiver operating characteristic (ROC) curve, and the decision curve analysis were used for the validation of the model, and internal validation was performed for assessment. The independent-samples t test was used for comparison of normally distributed continuous data between two groups, and the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups; the chi-square test was used for comparison of categorical variables between groups. Results There were significant differences between the sepsis group and the non-sepsis group in pulse rate, mean arterial pressure, duration pf symptoms, comorbidity of liver cirrhosis or malignant tumor, leukocyte count, neutrophil count, lymphocyte count, platelet count (PLT), activated partial thromboplastin time, fibrinogen, C-reactive protein, aspartate aminotransferase, alanine aminotransferase, albumin, total bilirubin (TBil), creatinine, potassium, and prognostic nutritional index (PNI) (all P<0.05). In the training set, the LASSO regression analysis identified four predictive factors of pulse rate, PLT, TBil and PNI, and the multivariate Logistic regression analysis showed that pulse rate (odds ratio [OR]=1.033, 95% confidence interval [CI]: 1.006 — 1.061, P=0.018), PLT (OR=0.981, 95%CI: 0.975 — 0.987, P<0.001), TBil (OR=1.086, 95%CI: 1.053 — 1.125, P<0.001), and PNI (OR=0.935, 95%CI: 0.882 — 0.988, P=0.019) were independent influencing factors for the risk of sepsis in patients with PLA. The model constructed based on these factors showed a good predictive ability, with an area under the ROC curve of 0.948 (95%CI: 0.923 — 0.973) in the training set and 0.912 (95%CI: 0.848 — 0.976) in the validation set. The decision curve analysis showed that the model has a good net benefit within the range of 0.3 — 0.9 for threshold probability. Conclusion The nomogram prediction model constructed based on pulse rate, PLT, TBil, and PNI has a certain clinical value and can well predict the risk of sepsis in patients with PLA. -
Key words:
- Liver Abscess /
- Sepsis /
- Risk Factors /
- Nomograms
-
表 1 PLA患者的一般资料
Table 1. General information on PLA patients
变量 总计(n=489) 非脓毒症组(n=306) 脓毒症组(n=183) 统计值 P值 男性[例(%)] 320(65.44) 200(65.36) 120(65.57) χ2=0.00 0.962 年龄(岁) 60.00(52.00~69.00) 59.00(51.25~69.00) 61.00(53.50~69.00) Z=-1.43 0.153 BMI(kg/m2) 24.22(21.88~26.12) 24.22(22.03~26.28) 24.22(21.71~25.94) Z=-0.56 0.576 脉率(次/min) 86(78~98) 82(76~92) 91(80~105) Z=-4.74 <0.001 MAP(mmHg) 89.77±12.64 90.73±11.83 88.18±13.77 t=2.08 0.038 症状持续时间(d) 7(4~15) 10(6~15) 5(3~10) Z=-5.89 <0.001 临床表现[例(%)] 发热 405(82.82) 248(81.05) 157(85.79) χ2=1.81 0.178 腹痛 189(38.65) 119(38.89) 70(38.25) χ2=0.02 0.889 胃肠道症状 132(26.99) 77(25.16) 55(30.05) χ2=1.39 0.238 合并症[例(%)] 糖尿病 180(36.81) 109(35.62) 71(38.80) χ2=0.50 0.481 高血压 129(26.38) 75(24.51) 54(29.51) χ2=1.47 0.225 胆道疾病 55(11.25) 33(10.78) 22(12.02) χ2=0.18 0.675 恶性肿瘤 66(13.50) 34(11.11) 32(17.49) χ2=3.99 0.046 肝硬化 12(2.45) 3(0.98) 9(4.92) χ2=5.86 0.015 PLA感染途径[例(%)] χ2=19.22 <0.001 胆源性 137(28.02) 78(25.49) 59(32.24) 其他 51(10.43) 20(6.54) 31(16.94) 隐源性 301(61.55) 208(67.97) 93(50.82) 治疗方式[例(%)] χ2=1.51 0.471 单用抗生素 188(38.45) 114(37.25) 74(40.44) 抗生素+经皮穿刺引流 272(55.62) 176(57.52) 96(52.46) 抗生素+手术 29(5.93) 16(5.23) 13(7.10) 表 2 PLA患者的实验室资料、影像学表现及临床结局
Table 2. Laboratory data, imaging manifestations, and clinical outcomes in patients with PLA
变量 总计(n=489) 非脓毒症组(n=306) 脓毒症组(n=183) 统计值 P值 实验室结果 WBC(×109/L) 10.20(7.80~14.30) 9.90(7.20~13.67) 10.90(8.55~15.00) Z=-2.35 0.019 NEUT(×109/L) 8.69(5.80~12.29) 7.99(5.36~11.35) 9.48(6.92~13.23) Z=-3.56 <0.001 LYM(×109/L) 1.0(0.6~1.4) 1.2(0.9~1.6) 0.7(0.5~1.1) Z=-9.16 <0.001 PLT(×109/L) 203.00(102.00~296.00) 261.50(193.25~348.00) 85.00(47.50~128.00) Z=-14.61 <0.001 CRP(mg/L) 136.20(74.60~200.00) 116.05(65.35~184.30) 155.60(95.00~225.95) Z=-4.68 <0.001 APTT(s) 28.90(26.50~31.80) 28.25(26.20~31.00) 30.10(27.75~33.30) Z=-5.14 <0.001 Fib(g/L) 5.48(4.42~6.96) 5.75(4.61~7.19) 5.06(4.05~6.48) Z=-3.66 <0.001 AST(U/L) 36.0(22.0~72.0) 28.0(20.0~44.0) 63.0(33.5~131.0) Z=-8.77 <0.001 ALT(U/L) 47.0(26.0~91.0) 38.0(23.0~67.0) 71.0(38.0~138.5) Z=-6.56 <0.001 Alb(g/L) 31.90±6.43 33.87±5.70 28.59±6.23 t=9.58 <0.001 TBil(μmol/L) 13.00(8.50~23.10) 11.30(8.00~16.00) 24.40(10.80~43.25) Z=-8.67 <0.001 Cr(μmol/L) 57.0(47.0~72.0) 55.0(46.0~65.0) 62.0(50.0~89.5) Z=-5.10 <0.001 K(mmol/L) 3.82±0.58 3.95±0.56 3.61±0.55 t=6.54 <0.001 PNI 37.35±8.06 40.24±7.35 32.53±6.82 t=11.54 <0.001 影像学特征[例(%)] 单发 193(39.47) 120(39.22) 73(39.89) χ2=0.02 0.883 右侧 336(68.71) 210(68.63) 126(68.85) χ2=0.00 0.959 环形强化 98(20.04) 66(21.57) 32(17.49) χ2=1.19 0.275 临床结局[例(%)] 死亡 19(3.89) 1(0.33) 18(9.84) χ2=27.73 <0.001 侵袭综合征 16(3.27) 5(1.63) 11(6.01) χ2=6.93 0.008 急性肾衰竭 11(2.25) 0(0.00) 11(6.01) χ2=16.18 <0.001 急性肝衰竭 5(1.02) 1(0.33) 4(2.19) χ2=2.29 0.130 急性呼吸衰竭 28(5.73) 0(0.00) 28(15.30) χ2=49.66 <0.001 脓毒性休克 24(4.91) 1(0.33) 23(12.57) χ2=36.77 <0.001 表 3 PLA患者发生脓毒症风险的多因素Logistic回归分析
Table 3. Multifactorial Logistic regression analysis of the risk of sepsis in patients with PLA
变量 β值 SE Z值 OR(95%CI) P值 常数 -1.135 2.241 -0.510 0.321(0.003~24.856) 0.613 脉率 0.032 0.014 2.370 1.033(1.006~1.061) 0.018 PLT -0.019 0.003 -7.310 0.981(0.975~0.987) <0.001 TBil 0.082 0.017 4.870 1.086(1.053~1.125) <0.001 PNI -0.067 0.029 -2.350 0.935(0.882~0.988) 0.019 -
[1] KHIM G, EM S, MO S, et al. Liver abscess: Diagnostic and management issues found in the low resource setting[J]. Br Med Bull, 2019, 132( 1): 45- 52. DOI: 10.1093/bmb/ldz032. [2] Emergency Medicine Branch of the Chinese Medical Association. Emergency expert consensus on diagnosis and treatment of bacterial liver abscess[J]. Chin J Emerg Med, 2022, 31( 3): 273- 280. DOI: 10.3760/cma.j.issn.1671-0282.2022.03.003.中华医学会急诊医学分会. 细菌性肝脓肿诊治急诊专家共识[J]. 中华急诊医学杂志, 2022, 31( 3): 273- 280. DOI: 10.3760/cma.j.issn.1671-0282.2022.03.003. [3] ZHANG J, GAO Y, DU ZQ, et al. Clinical features and prognosis of gas-forming and non-gas-forming pyogenic liver abscess: A comparative study[J]. Surg Infect(Larchmt), 2021, 22( 4): 427- 433. DOI: 10.1089/sur.2020.245. [4] SEYMOUR CW, LIU VX, IWASHYNA TJ, et al. Assessment of clinical criteria for sepsis: For the third international consensus definitions for sepsis and septic shock(sepsis-3)[J]. JAMA, 2016, 315( 8): 762- 774. DOI: 10.1001/jama.2016.0288. [5] EVANS L, RHODES A, ALHAZZANI W, et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021[J]. Crit Care Med, 2021, 49( 11): e1063- e1143. DOI: 10.1097/ccm.0000000000005337. [6] VILLANUEVA DM, TAUNK P, KRISHNAN P, et al. Emerging multiorgan Klebsiella pneumoniae invasive syndrome leading to septic shock: A case report and review of the literature[J]. Cureus, 2022, 14( 7): e26647. DOI: 10.7759/cureus.26647. [7] HELMS J, CATOIRE P, ABENSUR VUILLAUME L, et al. Oxygen therapy in acute hypoxemic respiratory failure: Guidelines from the SRLF-SFMU consensus conference[J]. Ann Intensive Care, 2024, 14( 1): 140. DOI: 10.1186/s13613-024-01367-2. [8] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [9] KELLUM JA, ROMAGNANI P, ASHUNTANTANG G, et al. Acute kidney injury[J]. Nat Rev Dis Primers, 2021, 7( 1): 52. DOI: 10.1038/s41572-021-00284-z. [10] CHO H, LEE ES, LEE YS, et al. Predictors of septic shock in initially stable patients with pyogenic liver abscess[J]. Scand J Gastroenterol, 2017, 52( 5): 589- 594. DOI: 10.1080/00365521.2017.1288757. [11] HE MY, WANG CM, ZHAI WL, et al. Study the influence factors of treatment prognosis in septic shock patients[J]. Clin J Med Offic, 2023, 51( 6): 570- 573, 578. DOI: 10.16680/j.1671-3826.2023.06.06.贺明轶, 王春梅, 翟文亮, 等. 脓毒症休克患者预后影响因素研究[J]. 临床军医杂志, 2023, 51( 6): 570- 573, 578. DOI: 10.16680/j.1671-3826.2023.06.06. [12] HU XD, BA XT, ZHU P. Risk factors and prognosis analysis of gastrointestinal bleeding secondary to sepsis[J]. J Clin Exp Med, 2023, 22( 19): 2032- 2035. DOI: 10.3969/j.issn.1671-4695.2023.19.005.胡向党, 巴晓彤, 朱萍. 脓毒症继发消化道出血危险因素及预后分析[J]. 临床和实验医学杂志, 2023, 22( 19): 2032- 2035. DOI: 10.3969/j.issn.1671-4695.2023.19.005. [13] LI ZB, LI QC, WU QP, et al. Analysis of risk factors for sepsis caused by liver abscess and establishment and verification of prediction model based on PNI and SII[J]. J Hainan Med Univ, 2024, 30( 12): 930- 938. DOI: 10.13210/j.cnki.jhmu.20240307.002.李泽标, 李秋呈, 吴秋萍, 等. 肝脓肿致脓毒症的危险因素分析及基于PNI、SII预测模型的建立与验证[J]. 海南医学院学报, 2024, 30( 12): 930- 938. DOI: 10.13210/j.cnki.jhmu.20240307.002. [14] LI J, WANG Y, LUO JH, et al. Development and validation of a nomogram for predicting sepsis in patients with pyogenic liver abscess[J]. Sci Rep, 2023, 13( 1): 10849. DOI: 10.1038/s41598-023-37907-2. [15] LIU F, YAO J, LIU CY, et al. Construction and validation of machine learning models for sepsis prediction in patients with acute pancreatitis[J]. BMC Surg, 2023, 23( 1): 267. DOI: 10.1186/s12893-023-02151-y. [16] COX D. Sepsis-it is all about the platelets[J]. Front Immunol, 2023, 14: 1210219. DOI: 10.3389/fimmu.2023.1210219. [17] LI Y, ZOU ZP, ZHANG YL, et al. Dynamics in perioperative neutrophil-to-lymphocyte*platelet ratio as a predictor of early acute kidney injury following cardiovascular surgery[J]. Ren Fail, 2021, 43( 1): 1012- 1019. DOI: 10.1080/0886022X.2021.1937220. [18] MEYER J, LEJMI E, FONTANA P, et al. A focus on the role of platelets in liver regeneration: Do platelet-endothelial cell interactions initiate the regenerative process?[J]. J Hepatol, 2015, 63( 5): 1263- 1271. DOI: 10.1016/j.jhep.2015.07.002. [19] GRECO E, LUPIA E, BOSCO O, et al. Platelets and multi-organ failure in sepsis[J]. Int J Mol Sci, 2017, 18( 10): 2200. DOI: 10.3390/ijms18102200. [20] CZERWONKO ME, HUESPE P, BERTONE S, et al. Pyogenic liver abscess: Current status and predictive factors for recurrence and mortality of first episodes[J]. HPB(Oxford), 2016, 18( 12): 1023- 1030. DOI: 10.1016/j.hpb.2016.09.001. [21] ZHANG SY, CHEN YX. Progress in diagnosis and treatment of pyogenic liver abscess[J]. J Clin Hepatol, 2018, 34( 7): 1577- 1580. DOI: 10.3969/j.issn.1001-5256.2018.07.046.章顺轶, 陈岳祥. 细菌性肝脓肿诊治进展[J]. 临床肝胆病杂志, 2018, 34( 7): 1577- 1580. DOI: 10.3969/j.issn.1001-5256.2018.07.046. [22] XIE TH, XIN Q, CHEN R, et al. Clinical value of prognostic nutritional index and neutrophil-to-lymphocyte ratio in prediction of the development of sepsis-induced kidney injury[J]. Dis Markers, 2022, 2022: 1449758. DOI: 10.1155/2022/1449758. [23] CHEN L, BAI P, KONG XY, et al. Prognostic nutritional index(PNI) in patients with breast cancer treated with neoadjuvant chemotherapy as a useful prognostic indicator[J]. Front Cell Dev Biol, 2021, 9: 656741. DOI: 10.3389/fcell.2021.656741. [24] ZHANG JL, CHEN Y, ZOU L, et al. Prognostic nutritional index as a risk factor for diabetic kidney disease and mortality in patients with type 2 diabetes mellitus[J]. Acta Diabetol, 2023, 60( 2): 235- 245. DOI: 10.1007/s00592-022-01985-x. [25] GIRARDOT T, RIMMELÉ T, VENET F, et al. Apoptosis-induced lymphopenia in sepsis and other severe injuries[J]. Apoptosis, 2017, 22( 2): 295- 305. DOI: 10.1007/s10495-016-1325-3. [26] XU J, ZHOU XH, ZHENG C. The geriatric nutritional risk index independently predicts adverse outcomes in patients with pyogenic liver abscess[J]. BMC Geriatr, 2019, 19( 1): 14. DOI: 10.1186/s12877-019-1030-5. [27] DING R, XIE W, LIU LG, et al. Clinical features of Klebsiella pneumoniae liver abscess and influencing factors for prognosis[J]. J Clin Hepatol, 2022, 38( 7): 1584- 1589. DOI: 10.3969/j.issn.1001-5256.2022.07.023.丁蕊, 谢雯, 刘丽改, 等. 肺炎克雷伯菌肝脓肿的临床特征及预后影响因素分析[J]. 临床肝胆病杂志, 2022, 38( 7): 1584- 1589. DOI: 10.3969/j.issn.1001-5256.2022.07.023. -



 PDF下载 ( 2192 KB)
PDF下载 ( 2192 KB)

 下载:
下载: