高代谢风险慢性乙型肝炎患者发生肝硬化的影响因素分析及预测模型构建
DOI: 10.12449/JCH250616
Risk factors for liver cirrhosis in chronic hepatitis B patients with high metabolic risks and establishment of a predictive model
-
摘要:
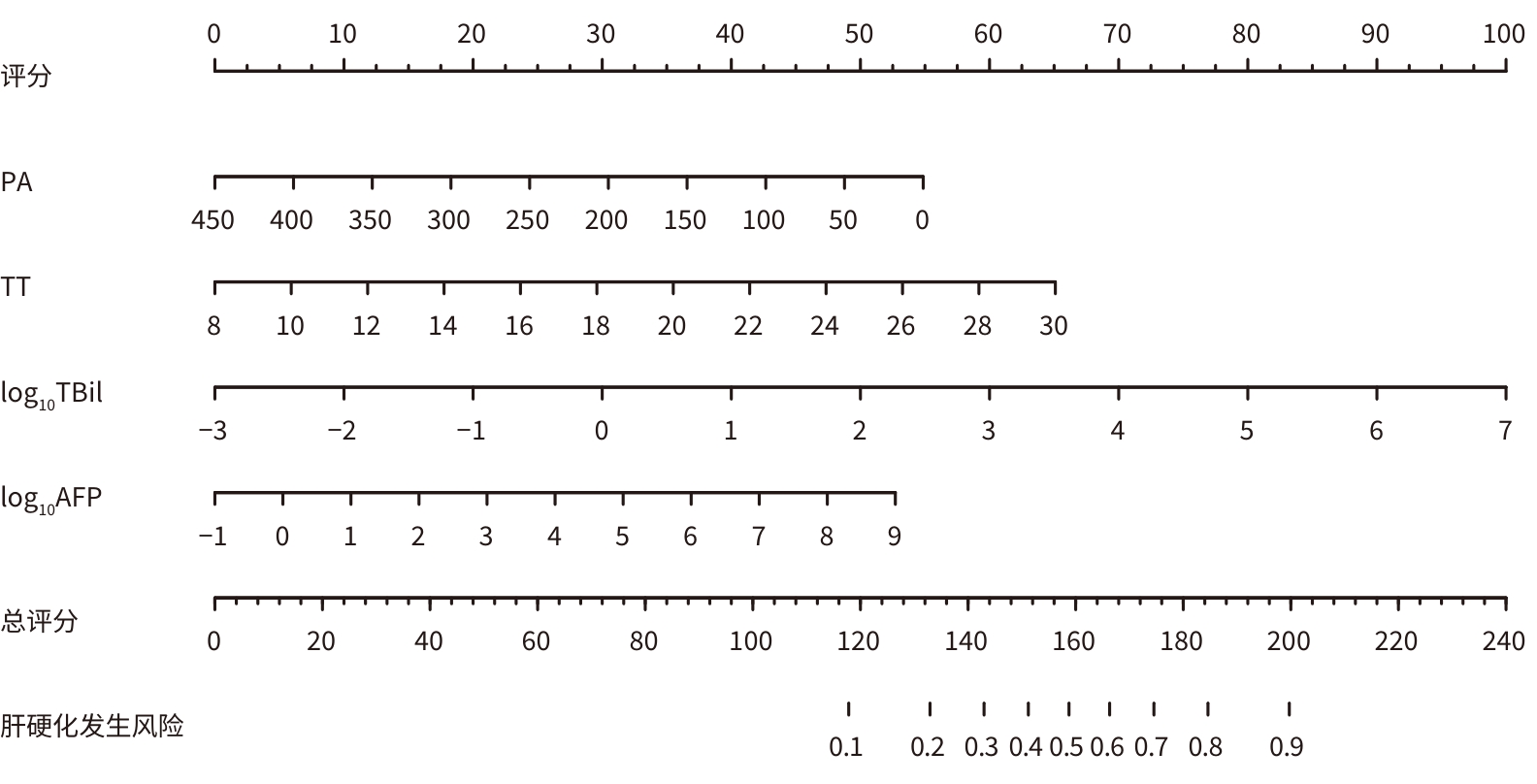
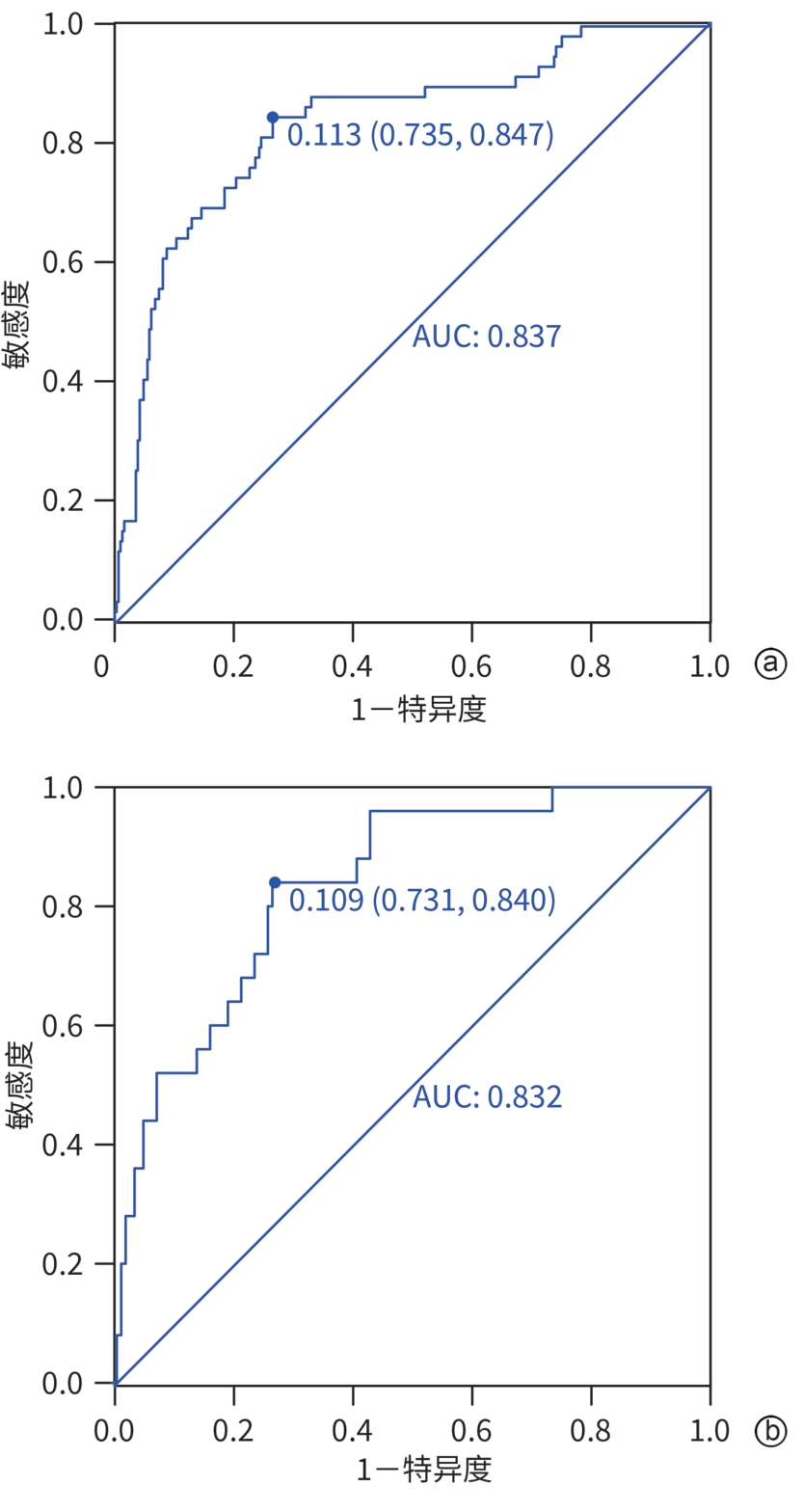
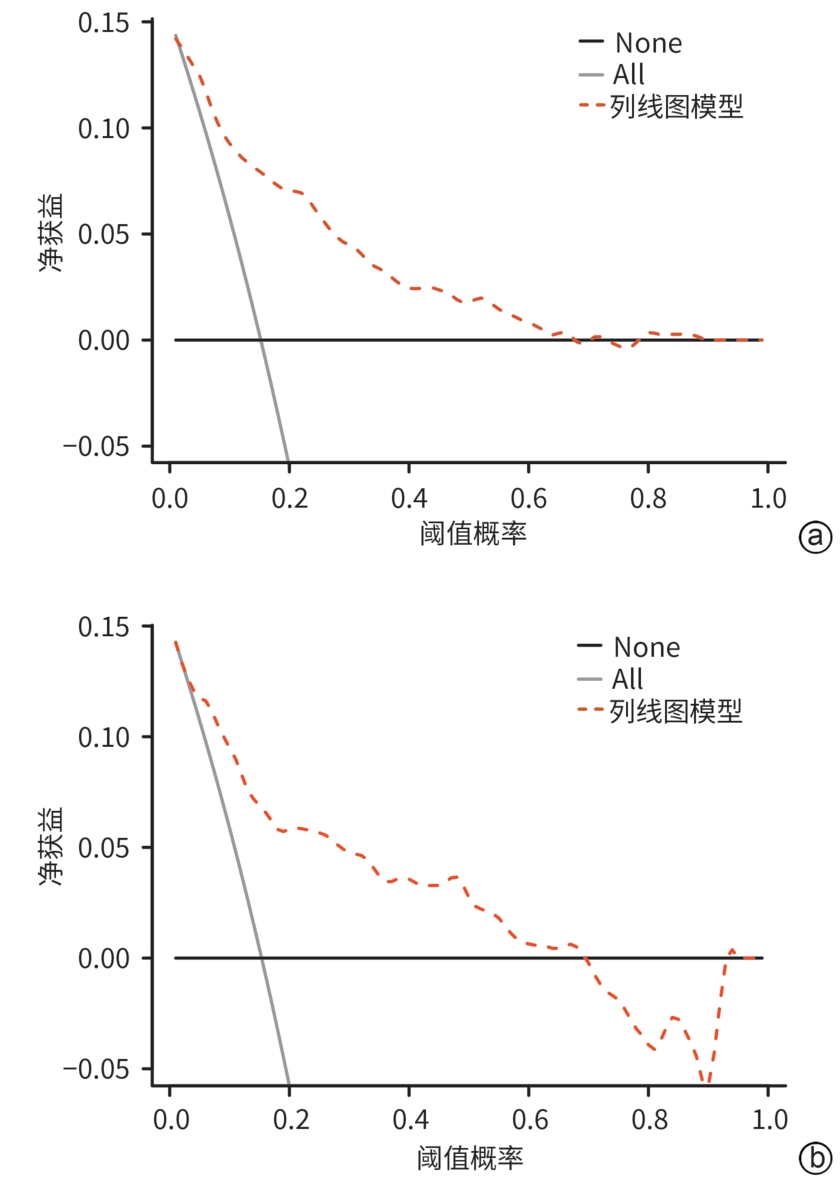
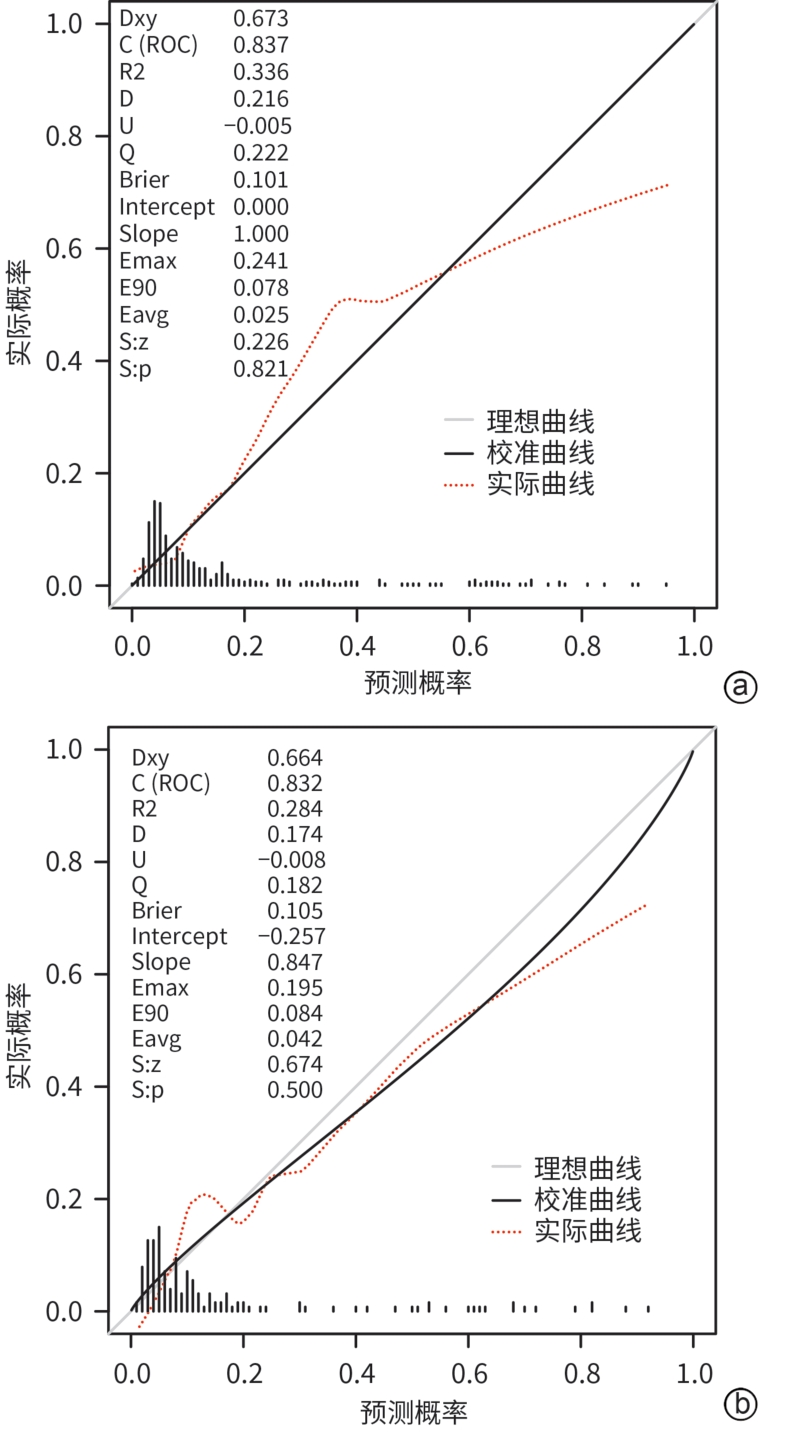
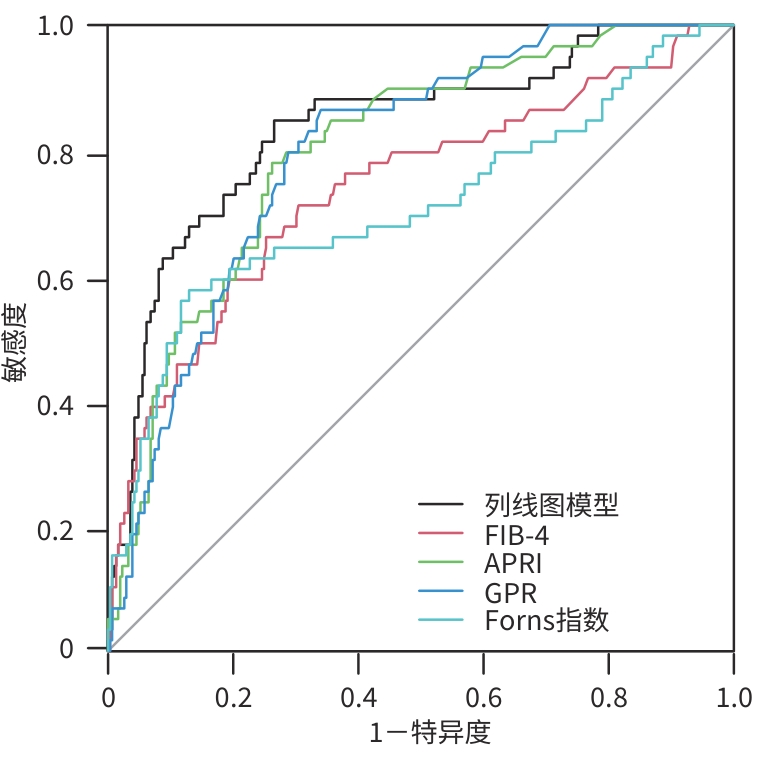
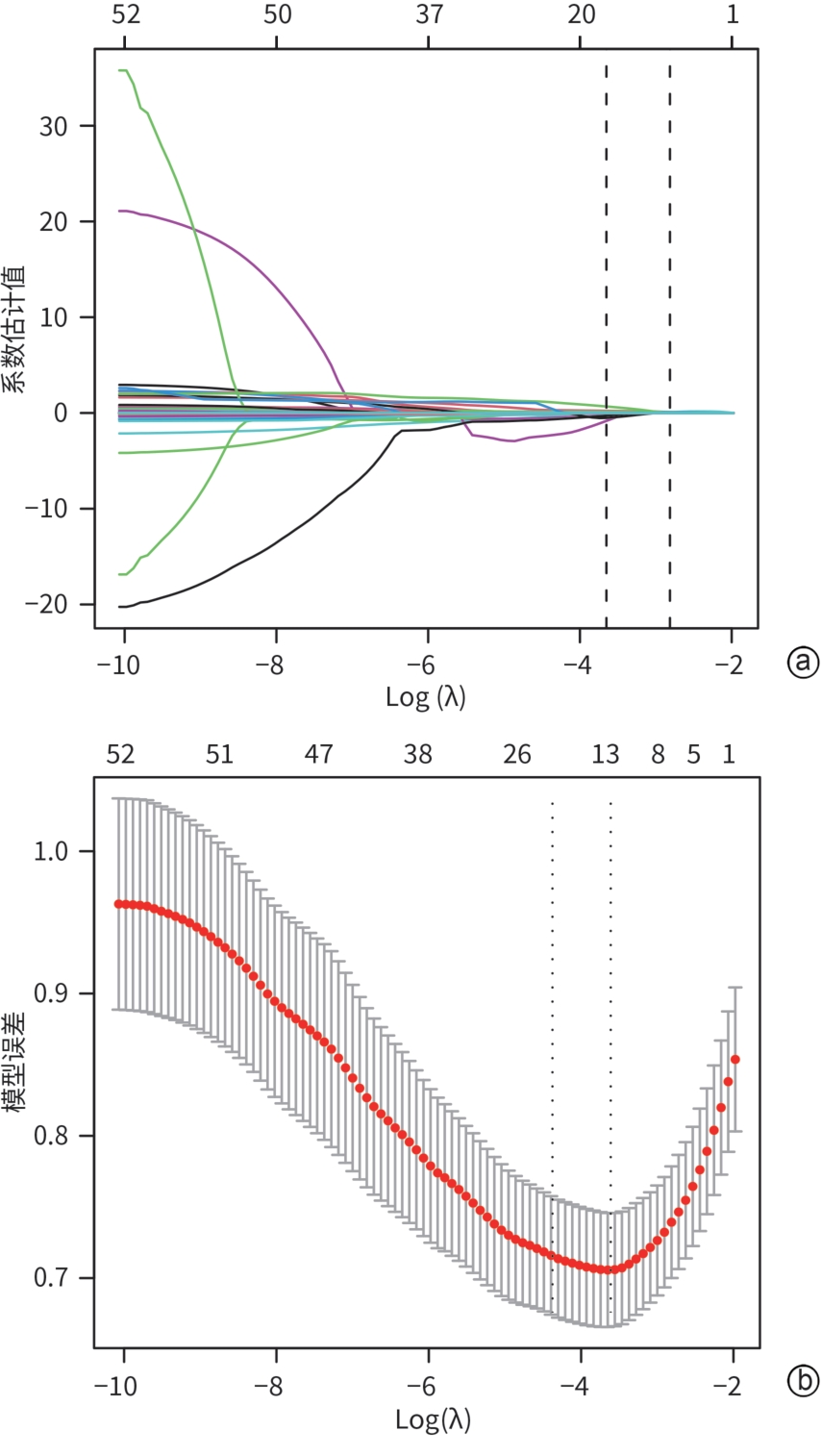
目的 探讨高代谢风险慢性乙型肝炎(CHB)患者发生肝硬化的主要危险因素,并构建无创预测模型,评估其与FIB-4、APRI、GPR及Forns指数模型的诊断效能差异。 方法 选取2017年9月1日—2022年10月31日于广西医科大学第二附属医院诊治的527例高代谢风险CHB患者,并按照7∶3比例随机分为建模组(n=368)和验证组(n=159)。在建模组中通过LASSO回归、多因素Logistic回归分析筛选出独立影响因素,并建立列线图模型,采用受试者操作特征曲线(ROC曲线)、校准曲线和决策曲线在建模组和验证组中对列线图预测模型进行验证以判断其区分度、校准度和临床实用性。通过Delong检验比较列线图预测模型与其他模型ROC曲线下面积(AUC)的差异。 结果 多因素Logistic回归分析显示,前白蛋白(OR=0.993,95%CI:0.988~0.999,P=0.019)、凝血酶时间(OR=1.182,95%CI:1.006~1.385,P=0.047)、log10TBil(OR=1.710,95%CI:1.239~2.419,P=0.001)、log10AFP(OR=1.327,95%CI:1.052~1.683,P=0.018)是高代谢风险CHB患者发生肝硬化的独立影响因素。依据多因素分析结果,构建风险预测模型列线图,其AUC为0.837(95%CI:0.788~0.888),特异度为73.5%,敏感度为84.7%,诊断效能高于FIB-4(0.739)、APRI(0.802)、GPR(0.800)、Forns指数(0.709)(Z值分别为2.815、2.271、1.989、2.722,P值分别为0.005、0.017、0.045、0.006)。 结论 基于前白蛋白、凝血酶时间、log10TBil、log10AFP建立的列线图模型具有一定的临床应用价值。 Abstract:Objective To investigate the main risk factors for liver cirrhosis in chronic hepatitis B (CHB) patients with high metabolic risk, to establish a noninvasive predictive model, and to compare the diagnostic efficiency of this model and other models including fibrosis-4 (FIB-4), aspartate aminotransferase-to-platelet ratio index (APRI), gamma-glutamyl transpeptidase-to-platelet ratio (GPR), and Forns index. Methods A total of 527 CHB patients with high metabolic risks who were admitted to The Second Affiliated Hospital of Guangxi Medical University from September 1, 2017 to October 31, 2022 were enrolled as subjects, and they were randomly divided into modeling group with 368 patients and validation group with 159 patients at a ratio of 7∶3. The LASSO regression analysis and the multivariate Logistic regression analysis were performed for the modeling group to identify independent risk factors, and a nomogram model was established. The receiver operating characteristic (ROC) curve, the calibration curve, and the decision curve analysis were used to validate the nomogram prediction model in the modeling group and the validation group and assess its discriminatory ability, calibration, and clinical practicability. The Delong test was used to compare the area under the ROC curve (AUC) of the nomogram prediction model and other models. Results The multivariate Logistic regression analysis showed that prealbumin (odds ratio [OR] = 0.993, 95% confidence interval [CI]: 0.988 — 0.999, P= 0.019), thrombin time (OR=1.182, 95% CI: 1.006 — 1.385, P=0.047), log10 total bilirubin (TBil) (OR=1.710, 95%CI: 1.239 — 2.419, P=0.001), and log10 alpha-fetoprotein (AFP) (OR=1.327, 95%CI: 1.052 — 1.683, P=0.018) were independent influencing factors for liver cirrhosis in CHB patients with high metabolic risks. A nomogram model for risk prediction was established based on the multivariate analysis, which had an AUC of 0.837 (95%CI: 0.788 — 0.888), a specificity of 73.5%, and a sensitivity of 84.7%, as well as a significantly higher diagnostic efficiency than the models of FIB-4 (0.739), APRI (0.802), GPR (0.800), and Forns index (0.709) (Z=2.815, 2.271, 1.989, and 2.722, P=0.005, 0.017, 0.045, and 0.006). Conclusion The nomogram model established based on prealbumin, thrombin time, log10 TBil, and log10 AFP has a certain clinical application value. -
Key words:
- Hepatitis B, Chronic /
- High Metabolic Risk /
- Liver Cirrhosis /
- Root Cause Analysis /
- Nomograms
-
表 1 建模组和验证组基线特征
Table 1. Modeling cohort and validating cohort baseline characteristics
项目 建模组(n=368) 验证组(n=159) P值 年龄(岁) 46.96±12.51 46.42±13.05 0.550 性别[例(%)] 0.155 女 85(23.10) 46(28.93) 男 283(76.90) 113(71.07) 身体质量指数(kg/m2) 23.83±3.65 23.87±4.04 0.975 腹围(cm) 65.30±12.72 64.26±12.32 0.304 高血压[例(%)] 105(28.53) 35(22.01) 0.120 糖尿病[例(%)] 90(24.46) 42(26.42) 0.634 LSM[例(%)] 0.145 <7.3 kPa 124(33.70) 54(33.96) 7.3~9.6 kPa 81(22.01) 30(18.87) 9.7~12.3 kPa 57(15.49) 25(15.72) 12.4~16.9 kPa 55(14.95) 17(10.69) ≥17.0 kPa 51(13.86) 33(20.75) 脂肪衰减(db/m) 215.8±33.4 214.6±34.2 0.590 PLT(×109/L) 208.38±68.55 213.43±77.26 0.996 Alb(g/dL) 40.80±6.11 41.08±5.47 0.451 PA(mg/L) 195.49±75.21 189.34±80.07 0.378 TBil(μmol/L) 11.20(7.80~18.06) 11.70(8.40~22.35) 0.281 DBil(μmol/L) 4.40(3.00~7.50) 4.50(3.30~10.20) 0.239 IBil(μmol/L) 6.50(4.28~9.53) 6.90(4.60~10.95) 0.221 AST(U/L) 35.6±8.1 33.2±7.9 0.202 ALT(U/L) 38.2±9.4 39.6±6.5 0.323 空腹血糖(mmol/L) 6.50±3.05 6.38±2.98 0.390 餐后2 h血糖(mmol/L) 9.89±4.73 10.15±4.66 0.419 TG(mg/dL) 1.28(0.94~1.92) 1.29(0.90~1.89) 0.749 HDL(mg/dL) 0.98±0.38 0.95±0.37 0.618 糖化血红蛋白(mmol/L) 7.12±2.50 7.21±2.60 0.955 总胆固醇(mg/dL) 4.15±1.30 4.03±1.09 0.535 TT(s) 14.51±1.90 14.73±2.02 0.134 AFP(μg/L) 2.61(1.82~4.39) 2.64(1.73~4.82) 0.754 HBsAg(IU/mL) 204.5±87.0 187.2±95.9 0.056 抗-HBs(mIU/mL) 1.04(1.00~1.62) 1.02(1.00~1.65) 0.850 HBeAg(PEIU/mL) 1.01(1.00~1.04) 1.01(1.00~1.13) 0.262 抗-HBe(PEIU/mL) 3.9±1.7 3.7±1.8 0.126 抗-HBc(PEIU/mL) 7.7±1.5 7.7±1.5 0.319 HBV DNA(log10 IU/mL) 3.70±1.97 3.60±1.94 0.768 注:PA,前白蛋白;TT,凝血酶时间。
表 2 预测变量多因素Logistic回归分析
Table 2. Multivariate Logistic regression analysis of predictive variables
项目 β值 SE Wald OR(95%CI) P值 截距 -4.953 1.525 -3.249 0.007(0.000~0.134) 0.001 PA -0.007 0.003 -2.343 0.993(0.988~0.999) 0.019 TT 0.159 0.080 1.986 1.182(1.006~1.385) 0.047 log10TBil 0.537 0.171 3.147 1.710(1.239~2.419) 0.001 log10AFP 0.283 0.120 2.375 1.327(1.052~1.683) 0.018 表 3 列线图模型与各评分系统预测高代谢风险CHB患者发生肝硬化的ROC曲线分析
Table 3. Analysis of the ROC curve for the prediction of cirrhosis in patients with high metabolic risk CHB by the nomogram model and various scoring systems
项目 AUC 95%CI 敏感度(%) 特异度(%) cut-off值 PPV NPV 列线图模型 0.837 0.788~0.888 84.7 73.5 0.113 0.379 0.962 FIB-4 0.739 0.682~0.810 66.1 74.8 0.134 0.333 0.920 APRI 0.802 0.742~0.849 78.0 73.8 0.130 0.362 0.946 GPR 0.800 0.751~0.843 86.4 66.0 0.122 0.327 0.962 Forns指数 0.709 0.664~0.799 57.6 87.1 0.234 0.459 0.915 注:PPV,阳性预测值;NPV,阴性预测值。
-
[1] REVILL PA, PENICAUD C, BRECHOT C, et al. Meeting the challenge of eliminating chronic hepatitis B infection[J]. Genes(Basel), 2019, 10( 4): 260. DOI: 10.3390/genes10040260. [2] FANNING GC, ZOULIM F, HOU JL, et al. Therapeutic strategies for hepatitis B virus infection: Towards a cure[J]. Nat Rev Drug Discov, 2019, 18( 11): 827- 844. DOI: 10.1038/s41573-019-0037-0. [3] KHARE S, ARORA A, SHARMA P, et al. Performance of non-invasive blood parameters for ruling out significant liver fibrosis in patients with chronic hepatitis B[J]. J Clin Transl Hepatol, 2020, 8( 2): 143- 149. DOI: 10.14218/JCTH.2020.00002. [4] LU JL, WANG LM, LI M, et al. Metabolic syndrome among adults in China: The 2010 China noncommunicable disease surveillance[J]. J Clin Endocrinol Metab, 2017, 102( 2): 507- 515. DOI: 10.1210/jc.2016-2477. [5] YU MW, LIN CL, LIU CJ, et al. Influence of metabolic risk factors on risk of hepatocellular carcinoma and liver-related death in men with chronic hepatitis B: A large cohort study[J]. Gastroenterology, 2017, 153( 4): 1006- 1017. DOI: 10.1053/j.gastro.2017.07.001. [6] REN HN, WANG JN, GAO Y, et al. Metabolic syndrome and liver-related events: A systematic review and meta-analysis[J]. BMC Endocr Disord, 2019, 19( 1): 40. DOI: 10.1186/s12902-019-0366-3. [7] WONG GL, CHAN HL, YU Z, et al. Coincidental metabolic syndrome increases the risk of liver fibrosis progression in patients with chronic hepatitis B: A prospective cohort study with paired transient elastography examinations[J]. Aliment Pharmacol Ther, 2014, 39( 8): 883- 893. DOI: 10.1111/apt.12658. [8] HUANG SC, SU TH, TSENG TC, et al. Pre-existing and new-onset metabolic dysfunctions increase cirrhosis and its complication risks in chronic hepatitis B[J]. Am J Gastroenterol, 2024. DOI: 10.14309/ajg.0000000000002915.[ Online ahead of print] [9] HUANG YW, WANG TC, LIN SC, et al. Increased risk of cirrhosis and its decompensation in chronic hepatitis B patients with newly diagnosed diabetes: A nationwide cohort study[J]. Clin Infect Dis, 2013, 57( 12): 1695- 1702. DOI: 10.1093/cid/cit603. [10] STERLING RK, KING WC, WAHED AS, et al. Evaluating noninvasive markers to identify advanced fibrosis by liver biopsy in HBV/HIV co-infected adults[J]. Hepatology, 2020, 71( 2): 411- 421. DOI: 10.1002/hep.30825. [11] Chinese Society of Infectious Diseases, Chinese Medical Association; Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B(version 2019)[J]. J Clin Hepatol, 2019, 35( 12): 2648- 2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007.中华医学会感染病学分会, 中华医学会肝病学分会. 慢性乙型肝炎防治指南(2019年版)[J]. 临床肝胆病杂志, 2019, 35( 12): 2648- 2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007. [12] Expert Committee on Clinical Application Consensus of Transient Elastography(TE) Technology. Expert consensus on clinical application of transient elastography(TE)(2015 version)[J/CD]. Chin J Liver Dis(Electronic Version), 2015, 7( 2): 12- 18. DOI: 10.3969/j.issn.1674-7380.2015.02.002.瞬时弹性成像技术(TE)临床应用共识专家委员会. 瞬时弹性成像技术(TE)临床应用专家共识(2015年)[J/CD]. 中国肝脏病杂志(电子版), 2015, 7( 2): 12- 18. DOI: 10.3969/j.issn.1674-7380.2015.02.002. [13] YOU H, WANG FS, LI TS, et al. Guidelines for the prevention and treatment of chronic hepatitis B(version 2022)[J]. J Clin Transl Hepatol, 2023, 11( 6): 1425- 1442. DOI: 10.14218/JCTH.2023.00320. [14] STERLING RK, LISSEN E, CLUMECK N, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection[J]. Hepatology, 2006, 43( 6): 1317- 1325. DOI: 10.1002/hep.21178. [15] WAI CT, GREENSON JK, FONTANA RJ, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C[J]. Hepatology, 2003, 38( 2): 518- 526. DOI: 10.1053/jhep.2003.50346. [16] BOYD A, BOTTERO J, LACOMBE K. The γ-glutamyl transpeptidase-to-platelet ratio as a predictor of liver fibrosis in patients co-infected with HBV and HIV[J]. Gut, 2016, 65( 4): 718- 720. DOI: 10.1136/gutjnl-2015-310607. [17] FORNS X, AMPURDANÈS S, LLOVET JM, et al. Identification of chronic hepatitis C patients without hepatic fibrosis by a simple predictive model[J]. Hepatology, 2002, 36( 4 Pt 1): 986- 992. DOI: 10.1053/jhep.2002.36128. [18] REN CY, FANG WD, CHEN G, et al. Value of albumin to alkaline phosphatase ratio in the clinical prediction of hepatitis B cirrhosis[J]. J Clin Exp Med, 2024, 23( 16): 1707- 1711. DOI: 10.3969/j.issn.1671-4695.2024.16.008.任才月, 方卫东, 陈刚, 等. 白蛋白与碱性磷酸酶比值在乙型肝炎肝硬化预测中的临床价值[J]. 临床和实验医学杂志, 2024, 23( 16): 1707- 1711. DOI: 10.3969/j.issn.1671-4695.2024.16.008. [19] PENG JL, HE GL, CHEN H, et al. Study on correlation between coagulation indexes and disease progression in patients with cirrhosis[J]. Am J Transl Res, 2021, 13( 5): 4614- 4623. [20] FORCE M, PARK G, CHALIKONDA D, et al. Alpha-fetoprotein(AFP) and AFP-L3 is most useful in detection of recurrence of hepatocellular carcinoma in patients after tumor ablation and with low AFP level[J]. Viruses, 2022, 14( 4): 775. DOI: 10.3390/v14040775. [21] WU D, ZHANG XJ, CHEN W. Correlation between serum HBV-DNA levels and liver function, CEA, AFP levels in patients with hepatitis B cirrhosis[J]. Hainan Med J, 2022, 33( 21): 2815- 2817. DOI: 10.3969/j.issn.1003-6350.2022.21.025.吴丹, 张锡坚, 陈伟. 乙肝肝硬化患者血清HBV-DNA水平与肝功能、CEA及AFP水平的相关性[J]. 海南医学, 2022, 33( 21): 2815- 2817. DOI: 10.3969/j.issn.1003-6350.2022.21.025. [22] SCHMIDT LE, DALHOFF K. Alpha-fetoprotein is a predictor of outcome in acetaminophen-induced liver injury[J]. Hepatology, 2005, 41( 1): 26- 31. DOI: 10.1002/hep.20511. [23] ZHANG LR, LIU Y, WANG ZZ. The combined detection predictive valve of in the risk hepatocellular carcinoma in liver cirrhosis patients infected with HBV GDF15, miR-122, AFP, and PIVKA-Ⅱ[J]. J Clin Exp Med, 2024, 23( 2): 121- 126. DOI: 10.3969/j.issn.1671-4695.2024.02.003.张黎然, 刘媛, 王珍子. GDF15、miR-122、AFP和PIVKA-Ⅱ联合评估在HBV感染肝硬化患者肝细胞癌发生风险中的预测价值[J]. 临床和实验医学杂志, 2024, 23( 2): 121- 126. DOI: 10.3969/j.issn.1671-4695.2024.02.003. [24] FUNG J, LAI CL, FONG DY, et al. Correlation of liver biochemistry with liver stiffness in chronic hepatitis B and development of a predictive model for liver fibrosis[J]. Liver Int, 2008, 28( 10): 1408- 1416. DOI: 10.1111/j.1478-3231.2008.01784.x. [25] CASTÉRA L, SEBASTIANI G, LE BAIL B, et al. Prospective comparison of two algorithms combining non-invasive methods for staging liver fibrosis in chronic hepatitis C[J]. J Hepatol, 2010, 52( 2): 191- 198. DOI: 10.1016/j.jhep.2009.11.008. [26] LUO Y. Application of combined detection of serum total bile acids and prealbumin in diagnosis of liver diseases[J]. Chongqing Med, 2007, 36( 12): 1167- 1168, 1170. DOI: 10.3969/j.issn.1671-8348.2007.12.022.罗云. 联合检测血清总胆汁酸和前清蛋白在肝脏疾病诊断中的应用[J]. 重庆医学, 2007, 36( 12): 1167- 1168, 1170. DOI: 10.3969/j.issn.1671-8348.2007.12.022. [27] SHIN SK, KIM JH, PARK H, et al. Improvement of liver function and non-invasive fibrosis markers in hepatitis B virus-associated cirrhosis: 2 years of entecavir treatment[J]. J Gastroenterol Hepatol, 2015, 30( 12): 1775- 1781. DOI: 10.1111/jgh.13020. [28] PURI K, NOBILI V, MELVILLE K, et al. Serum bilirubin level is inversely associated with nonalcoholic steatohepatitis in children[J]. J Pediatr Gastroenterol Nutr, 2013, 57( 1): 114- 118. DOI: 10.1097/MPG.0b013e318291fefe. [29] KUMAR R, RASTOGI A, MARAS JS, et al. Unconjugated hyperbilirubinemia in patients with non-alcoholic fatty liver disease: A favorable endogenous response[J]. Clin Biochem, 2012, 45( 3): 272- 274. DOI: 10.1016/j.clinbiochem.2011.11.017. [30] SAKLAYEN MG. The global epidemic of the metabolic syndrome[J]. Curr Hypertens Rep, 2018, 20( 2): 12. DOI: 10.1007/s11906-018-0812-z. [31] DONG MH, WU JW, YU XP, et al. Validation and comparison of seventeen noninvasive models for evaluating liver fibrosis in Chinese hepatitis B patients[J]. Liver Int, 2018, 38( 9): 1562- 1570. DOI: 10.1111/liv.13688. [32] WANG SM, WANG N, YU Z, et al. Diagnostic values of APRI, AAR, and FIB-4 predictive models in autoimmune cirrhosis combined with esophagogastric fundal varices[J]. J Jilin Univ(Med Edit), 2024, 50( 2): 523- 528. DOI: 10.13481/j.1671-587X.20240227.王素梅, 王楠, 于珍, 等. APRI、AAR和FIB-4等预测模型对自身免疫性肝硬化伴食管胃底静脉曲张的诊断价值[J]. 吉林大学学报(医学版), 2024, 50( 2): 523- 528. DOI: 10.13481/j.1671-587X.20240227. [33] LI XT, HU BB, LIU HY, et al. Effectiveness of fibrosis-4 versus aspartate aminotransferase-to-platelet ratio index in evaluating liver fibrosis degree in patients with chronic HBV infection[J]. J Clin Hepatol, 2024, 40( 12): 2424- 2429. DOI: 10.12449/JCH241212.李小婷, 胡伯斌, 刘宏宇, 等. FIB-4和APRI评估慢性HBV感染者肝纤维化程度的效果比较[J]. 临床肝胆病杂志, 2024, 40( 12): 2424- 2429. DOI: 10.12449/JCH241212. [34] XIAO GQ, YANG JY, YAN LN. Comparison of diagnostic accuracy of aspartate aminotransferase to platelet ratio index and fibrosis-4 index for detecting liver fibrosis in adult patients with chronic hepatitis B virus infection: A systemic review and meta-analysis[J]. Hepatology, 2015, 61( 1): 292- 302. DOI: 10.1002/hep.27382. [35] WANG M, LUO WP, ZHANG GH, et al. Diagnostic value of FibroTouch, FibroScan, and acoustic radiation force impulse for liver fibrosis in patients with primary biliary cholangitis[J]. J Clin Hepatol, 2021, 37( 4): 817- 822. DOI: 10.3969/j.issn.1001-5256.2021.04.019.王民, 罗文萍, 张冠华, 等. FibroTouch、FibroScan及ARFI在原发性胆汁性胆管炎相关肝纤维化中的诊断价值[J]. 临床肝胆病杂志, 2021, 37( 4): 817- 822. DOI: 10.3969/j.issn.1001-5256.2021.04.019. [36] QI M. Study and analysis of correlation of liver hardness tester FibroTouch and FibroScan with pathological stage of liver[J]. China Med Pharm, 2016, 6( 21): 218- 220. DOI: 10.3969/j.issn.2095-0616.2016.21.063.亓民. 研究分析肝脏硬度测定仪FibroTouch与FibroScan与肝脏病理分期的相关性[J]. 中国医药科学, 2016, 6( 21): 218- 220. DOI: 10.3969/j.issn.2095-0616.2016.21.063. [37] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Gastroenterology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. Consensus on the diagnosis and therapy of hepatic fibrosis(2019)[J]. J Clin Hepatol, 2019, 35( 10): 2163- 2172. DOI: 10.3969/j.issn.1001-5256.2019.10.007.中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会感染病学分会. 肝纤维化诊断及治疗共识(2019年)[J]. 临床肝胆病杂志, 2019, 35( 10): 2163- 2172. DOI: 10.3969/j.issn.1001-5256.2019.10.007. -



 PDF下载 ( 2749 KB)
PDF下载 ( 2749 KB)

 下载:
下载: