基于体检人群调查代谢相关脂肪性肝病患者特征及生活方式
DOI: 10.12449/JCH250614
Characteristics and lifestyles of patients with metabolic dysfunction-associated fatty liver disease based on the physical examination population
-
摘要:
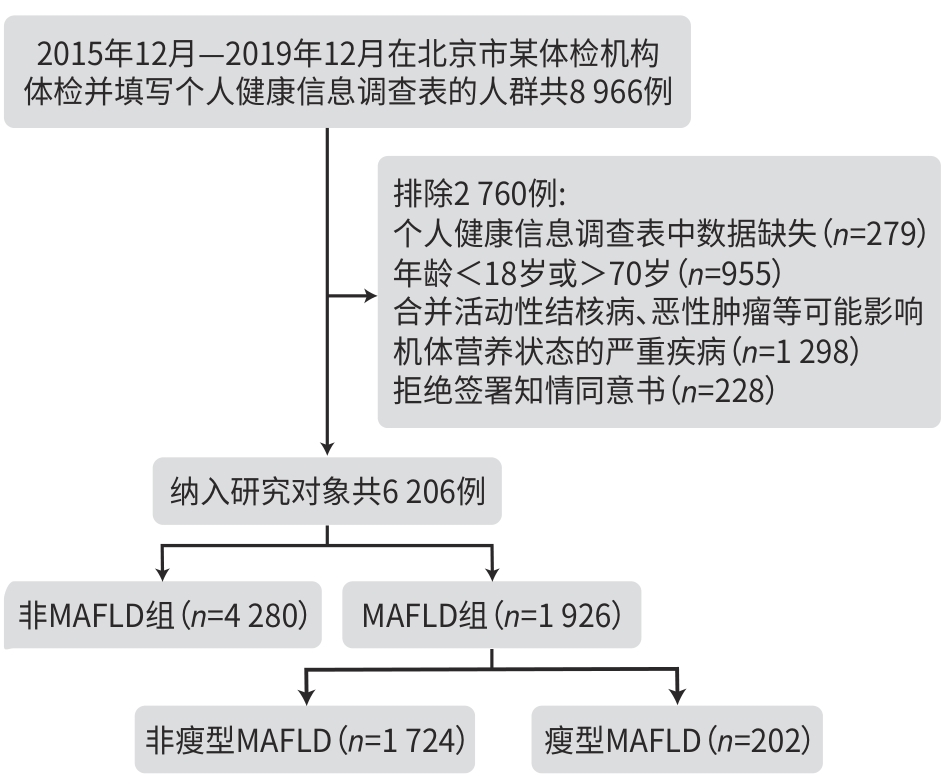
目的 对体检人群进行代谢相关脂肪性肝病(MAFLD)筛查,观察MAFLD患者特征,并对比MAFLD组与非MAFLD组在生活方式方面的差异。 方法 纳入2015年12月—2019年12月北京市某体检机构体检人群共6 206例进行横断面研究,按照新版MAFLD诊断标准将体检人群分为MAFLD组和非MAFLD组;按照BMI水平,进一步将MAFLD组分为瘦型MAFLD组(BMI<24 kg/m2)和非瘦型MAFLD组(BMI≥24 kg/m2),对比各组之间的人口学指标、学历、工作压力、身体测量指标及睡眠、饮食、运动等生活方式的差异。正态分布的计量资料两组间比较采用成组t检验,非正态分布的计量资料两组间比较采用Mann-Whitney U秩和检验,计数资料两组间比较采用χ2检验。 结果 MAFLD组1 926例(31.0%),非MAFLD组4 280例(69.0%)。MAFLD组年龄(Z=-14.459,P<0.001)、男性占比(χ2=72.004,P<0.001)、工作压力(χ2=7.744,P=0.005)、体质量(Z=-43.508,P<0.001)、BMI(Z=-47.621,P<0.001)、腰围(Z=-48.515,P<0.001)、臀围(Z=-42.121,P<0.001)、腰臀比(Z=-43.535,P<0.001)均显著高于非MAFLD组,但学历较低(χ2=33.583,P<0.001)。在行为方面,MAFLD组睡眠时间较少(χ2=5.820,P=0.016),进餐速度更快(χ2=74.476,P<0.001)。在饮食方面,MAFLD组摄入了更多的高钠、高糖、高热量(χ2=42.667,P<0.001)及低膳食纤维饮食(χ2=4.367,P=0.008)。在运动方面,MAFLD组无运动习惯占比高(χ2=10.278,P=0.001)。进一步分析显示,瘦型MAFLD组202例(10.5%),非瘦型MAFLD组1 724例(89.5%)。瘦型MAFLD组年龄(Z=3.368,P=0.001)、学历(χ2=9.647,P=0.002)显著高于非瘦型MAFLD组,而男性占比(χ2=27.664,P<0.001)、体质量(Z=-18.483,P<0.001)、BMI(Z=-23.286,P<0.001)、腰围(Z=-18.565,P<0.001)、臀围(Z=-18.097,P<0.001)均显著低于非瘦型MAFLD组;在行为方面,非瘦型MAFLD组进餐速度较快(χ2=4.549,P=0.033)。 结论 北京市体检人群中MAFLD患病率较高,且存在不良生活方式的人数较非MAFLD人群更多。 Abstract:Objective To screen for the patients with metabolic dysfunction-associated fatty liver disease (MAFLD) among the physical examination population, to observe the characteristics of MAFLD patients, and to compare the differences in lifestyle between the MAFLD population and the non-MAFLD population. Methods A cross-sectional study was conducted among 6 206 individuals who underwent physical examination in a physical examination institution in Beijing from December 2015 to December 2019, and according to the new diagnostic criteria for MAFLD, the examination population was divided into MAFLD group and non-MAFLD group. Based on body mass index (BMI), the MAFLD group was further divided into lean MAFLD group (BMI<24 kg/m2) and non-lean MAFLD group (BMI ≥24 kg/m2). Related data were compared between groups, including demographic indicators, education level, work pressure, physical measurement indicators, and lifestyles such as sleep, diet, and exercise. The independent-samples t test was used for comparison of normally distributed continuous data between two groups, the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups, and the chi-square test was used for comparison of categorical data between groups. Results Of all individuals in this study, 1 926 (31.1%) had MAFLD and 4 280 (68.9%) did not have MAFLD. Compared with the non-MAFLD group, the MAFLD group had significantly higher age (Z=-14.459, P<0.001), proportion of male patients (χ2=72.004, P<0.001), work pressure (χ2=7.744, P=0.005), body weight (Z=-43.508, P<0.001), BMI (Z=-47.621, P<0.001), waist circumference (Z=-48.515, P<0.001), hip circumference (Z=-42.121, P<0.001), and waist-hip ratio (Z=-43.535, P<0.001), as well as a significantly lower education level (χ2=33.583, P<0.001). In terms of behavior, the MAFLD group had a significantly shorter sleep time (χ2=5.820, P=0.016) and a significantly faster eating speed (χ2=74.476, P<0.001). In terms of diet, the patients in the MAFLD group consumed more high-sodium, high-sugar, and high-calorie diets (χ2=42.667, P<0.001) and low-fiber diet (χ2=4.367, P=0.008). In terms of exercise, the MAFLD group had a significantly higher proportion of patients without exercise habits (χ2=10.278, P=0.001). Further analysis showed that there were 202 individuals (10.5%) in the lean MAFLD group and 1 724 (89.5%) in the non-lean MAFLD group. Compared with the non-lean MAFLD group, the lean MAFLD group had significantly higher age (Z=3.368, P=0.001) and education level (χ2=9.647, P=0.002) and significantly lower proportion of male patients (χ2=27.664, P<0.001), body weight (Z=-18.483, P<0.001), BMI (Z=-23.286, P<0.001), waist circumference (Z=-18.565, P<0.001), and hip circumference (Z=-18.097, P<0.001), and in terms of behavior, the non-lean MAFLD group had a significantly faster eating speed (χ2=4.549, P=0.033). Conclusion There is a relatively high prevalence rate of MAFLD among the physical examination population in Beijing, with a higher number of people with unhealthy lifestyles compared with the non-MAFLD population. -
表 1 按MAFLD分层的患者特征
Table 1. Patient characteristics stratified by MAFLD
观察指标 MAFLD(n=1 926) 非MAFLD(n=4 280) 统计值 P值 年龄(岁) 39.0(32.0~52.0) 34.0(28.0~44.0) Z=-14.459 <0.001 男性[例(%)] 1 340(69.6) 1 576(36.8) χ2=72.004 <0.001 体质量(kg) 78.0(70.0~87.0) 61.0(54.0~69.0) Z=-43.508 <0.001 BMI(kg/m2) 27.1(25.3~29.3) 22.4(20.5~24.5) Z=-47.621 <0.001 腰围(cm) 91.0(86.0~97.0) 76.0(70.0~83.0) Z=-48.515 <0.001 臀围(cm) 104.0(100.0~108.0) 95.0(90.0~100.0) Z=-42.121 <0.001 腰臀比 0.88(0.85~0.92) 0.80(0.76~0.84) Z=-43.535 <0.001 最高学历[例(%)] χ2=33.583 <0.001 高中及以下 477(24.8) 786(18.4) 初中及以下 120(6.2) 231(5.4) 高中、中专 357(18.6) 555(13.0) 专科及以上 1 449(75.2) 3 494(81.6) 大学本科、专科 1 237(64.2) 2 700(63.1) 研究生及以上 212(11.0) 794(18.5) 工作压力[例(%)] χ2=7.744 0.005 压力不大 1 315(68.3) 3 071(71.8) 无 275(14.3) 374(8.7) 很小 115(6.0) 219(5.1) 较小 149(7.7) 419(9.9) 适中 776(40.3) 2 059(48.1) 压力大 611(31.7) 1 209(28.2) 较大 490(25.4) 1 024(23.9) 很大 121(6.3) 185(4.3) 表 2 按MAFLD分层的患者生活方式
Table 2. Patient lifestyles stratified by MAFLD
观察指标 MAFLD(n=1 926) 非MAFLD(n=4 280) χ2值 P值 每日睡眠时间[例(%)] 5.820 0.016 <8 h 1 379(71.6) 2 934(68.6) 5 h 129(6.7) 217(5.1) 6 h 550(28.6) 911(21.3) 7 h 700(36.3) 1 806(42.2) ≥8 h 547(28.4) 1 346(31.4) 8 h 496(25.7) 1 213(28.2) 9 h 28(1.4) 89(2.1) 10 h 21(1.1) 41(1.0) 11 h 1(0.1) 0(0.0) 12 h 1(0.1) 3(0.1) 每周早餐次数[例(%)] 0.005 0.944 不吃早餐 297(15.4) 663(15.5) 吃早餐 1 629(84.6) 3 617(84.5) 1~3次 180(9.4) 330(7.7) 4~6次 249(12.9) 511(11.9) 每天 1 200(62.3) 2 776(64.9) 进餐速度[例(%)] 74.476 <0.001 不快 1 114(57.8) 2 957(69.1) 慢(细嚼慢咽) 139(7.2) 575(13.4) 中等速度 975(50.6) 2 382(55.7) 快 812(42.2) 1 323(30.9) 有点快 734(38.2) 1 229(28.7) 很快(狼吞虎咽) 78(4.0) 94(2.2) 饮食口味[例(%)] 42.667 <0.001 口味重 1 434(74.5) 2 876(67.2) 偏咸 354(18.4) 792(18.5) 甜食多 628(32.6) 1 254(29.3) 油量大 452(23.5) 830(19.4) 中等适宜 492(25.5) 1 404(32.8) 饮食结构[例(%)] 4.367 0.008 粗粮多(如玉米、小米及豆类) 626(32.5) 1 678(39.2) 细粮多(精米、白面) 1 300(67.5) 2 602(60.8) 运动强度[例(%)] 10.278 0.001 不运动 991(51.5) 1 840(43.0) 运动 935(48.5) 2 440(57.0) 轻度(散步、打太极、跳舞) 453(23.5) 1 198(28.0) 中度(慢跑、骑车、爬山) 405(21.0) 907(21.2) 重度(游泳、打球、跳绳) 77(4.0) 335(7.8) 运动频率[例(%)] 不运动 991(51.5) 1 840(43.0) <1次/周 601(31.2) 1 198(28.0) ≥1次/周 334(17.3) 1 067(24.9) ≥1次/天 0(0.0) 175(4.1) 表 3 按BMI分层的患者特征
Table 3. Patient characteristics stratified by BMI
观察指标 瘦型MAFLD(n=202) 非瘦型MAFLD(n=1 724) 统计值 P值 年龄(岁) 43.0(34.0~56.0) 39.0(32.0~52.0) Z=3.368 0.001 男性[例(%)] 108(53.5) 1 232(71.5) χ2=27.664 <0.001 体质量(kg) 64.0(59.0~69.0) 79.4(73.0~88.0) Z=-18.483 <0.001 BMI(kg/m2) 23.0(22.1~23.6) 27.4(25.9~29.6) Z=-23.286 <0.001 腰围(cm) 81.0(78.0~85.0) 92.0(87.0~98.0) Z=-18.565 <0.001 臀围(cm) 96.0(94.0~100.0) 104.0(100.0~108.0) Z=-18.097 <0.001 腰臀比 0.842±0.003 0.886±0.001 t=-11.686 >0.05 最高学历[例(%)] χ2=9.647 0.002 高中及以下 32(15.8) 445(25.8) 初中及以下 6(2.9) 114(6.6) 高中、中专 26(12.9) 331(19.2) 专科及以上 170(84.2) 1 279(74.2) 大学本科、专科 141(69.8) 1 096(63.6) 研究生及以上 29(14.4) 183(10.6) 工作压力[例(%)] χ2=0.426 0.514 压力不大 142(70.3) 1 173(68.0) 无 41(20.3) 234(13.6) 很小 13(6.4) 102(5.8) 较小 15(7.4) 134(7.8) 适中 73(36.2) 703(40.8) 压力大 60(29.7) 551(32.0) 较大 49(24.3) 441(25.6) 很大 11(5.4) 110(6.4) 表 4 按BMI分层的患者生活方式
Table 4. Patient lifestyles stratified by BMI
观察指标 瘦型MAFLD(n=202) 非瘦型MAFLD(n=1 724) χ2值 P值 每日睡眠时间[例(%)] 0.051 0.821 <8 h 146(72.3) 1 233(71.4) 5 h 13(6.4) 116(6.7) 6 h 51(25.3) 499(28.9) 7 h 82(40.6) 618(35.8) ≥8 h 56(27.7) 491(28.6) 8 h 52(25.7) 444(25.8) 9 h 2(1.0) 26(1.5) 10 h 1(0.5) 20(1.2) 11 h 1(0.5) 0(0.0) 12 h 0(0.0) 1(0.1) 每周早餐次数[例(%)] 0.730 0.393 不吃早餐 27(13.4) 270(15.7) 吃早餐 175(86.8) 1 454(84.3) 1~3次 17(8.5) 163(9.4) 4~6次 20(9.9) 229(13.3) 每天 138(68.4) 1 062(61.6) 进餐速度[例(%)] 4.549 0.033 不快 131(64.8) 983(57.0) 慢(细嚼慢咽) 17(8.4) 122(7.1) 中等速度 114(56.4) 861(49.9) 快 71(35.2) 741(43.0) 有点快 65(32.2) 669(38.8) 很快(狼吞虎咽) 6(3.0) 72(4.2) 饮食口味[例(%)] 0.667 0.098 口味重 144(71.4) 1 291(74.9) 偏咸 39(19.3) 314(18.2) 甜食多 58(28.6) 572(33.2) 油量大 47(23.5) 405(23.5) 中等适宜 58(28.6) 433(25.1) 饮食结构[例(%)] 0.367 0.997 粗粮多(如玉米、小米及豆类) 64(31.9) 562(32.6) 细粮多(精米白面) 138(68.1) 1 162(67.4) 运动强度[例(%)] 0.875 0.350 不运动 103(51.1) 900(52.2) 运动 99(48.9) 824(47.8) 轻度(散步、打太极、跳舞) 41(20.2) 419(24.3) 中度(慢跑、骑车、爬山) 44(22.1) 361(20.9) 重度(游泳、打球、跳绳) 14(6.6) 44(2.6) 运动频率[例(%)] 不运动 103(51.0) 900(52.2) <1次/周 67(33.2) 512(29.7) ≥1次/周 32(15.8) 312(18.1) ≥1次/天 0(0.0) 0(0.0) -
[1] ESLAM M, SANYAL AJ, GEORGE J, et al. MAFLD: A consensus-driven proposed nomenclature for metabolic associated fatty liver disease[J]. Gastroenterology, 2020, 158( 7): 1999- 2014. e 1. DOI: 10.1053/j.gastro.2019.11.312. [2] Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of metabolic dysfunction-associated(non-alcoholic) fatty liver disease(Version 2024)[J]. J Pract Hepatol, 2024, 27( 4): 494- 510. DOI: 10.3760/cma.j.cn501113-20240327-00163.中华医学会肝病学分会. 代谢相关(非酒精性)脂肪性肝病防治指南(2024年版)[J]. 实用肝脏病杂志, 2024, 27( 4): 494- 510. DOI: 10.3760/cma.j.cn501113-20240327-00163. [3] RINELLA ME, NEUSCHWANDER-TETRI BA, SIDDIQUI MS, et al. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease[J]. Hepatology, 2023, 77( 5): 1797- 1835. DOI: 10.1097/HEP.0000000000000323. [4] YOUNOSSI ZM, ZELBER-SAGI S, HENRY L, et al. Lifestyle interventions in nonalcoholic fatty liver disease[J]. Nat Rev Gastroenterol Hepatol, 2023, 20( 11): 708- 722. DOI: 10.1038/s41575-023-00800-4. [5] CHAI XN, ZHOU BQ, NING N, et al. Effects of lifestyle intervention on adults with metabolic associated fatty liver disease: A systematic review and meta-analysis[J]. Front Endocrinol(Lausanne), 2023, 14: 1081096. DOI: 10.3389/fendo.2023.1081096. [6] LU JF, YU YL, ZHAO Y, et al. The correlation between workers' working pressure and physical and mental health analyzed by the job demand-resource stress model[J]. Work, 2021, 69( 2): 573- 583. DOI: 10.3233/WOR-213500. [7] BALAKRISHNAN M, LIU K, SCHMITT S, et al. Behavioral weight-loss interventions for patients with NAFLD: A systematic scoping review[J]. Hepatol Commun, 2023, 7( 8): e0224. DOI: 10.1097/HC9.0000000000000224. [8] JI TT, LI XF, YU YY, et al. Progress of lifestyle interventions for metabolic dysfunction-associated fatty liver disease[J]. J Clin Hepatol, 2023, 39( 8): 1789- 1796. DOI: 10.3969/j.issn.1001-5256.2023.08.004.纪童童, 李鑫飞, 于岩岩, 等. 代谢相关脂肪性肝病生活方式干预治疗进展[J]. 临床肝胆病杂志, 2023, 39( 8): 1789- 1796. DOI: 10.3969/j.issn.1001-5256.2023.08.004. [9] TANG A, NG CH, PHANG PH, et al. Comparative burden of metabolic dysfunction in lean NAFLD vs non-lean NAFLD- A systematic review and meta-analysis[J]. Clin Gastroenterol Hepatol, 2023, 21( 7): 1750- 1760. e 12. DOI: 10.1016/j.cgh.2022.06.029. [10] ZOU ZY, WONG VW, FAN JG. Epidemiology of nonalcoholic fatty liver disease in non-obese populations: Meta-analytic assessment of its prevalence, genetic, metabolic, and histological profiles[J]. J Dig Dis, 2020, 21( 7): 372- 384. DOI: 10.1111/1751-2980.12871. [11] KIM NH, KIM JH, KIM YJ, et al. Clinical and metabolic factors associated with development and regression of nonalcoholic fatty liver disease in nonobese subjects[J]. Liver Int, 2014, 34( 4): 604- 611. DOI: 10.1111/liv.12454. [12] FU Y, YU B, YANG B, et al. Association between chronotype and metabolic-associated fatty liver disease in employed adults: A longitudinal study in Southwestern China[J]. Chronobiol Int, 2023, 40( 12): 1557- 1565. DOI: 10.1080/07420528.2023.2285316. [13] WENG ZY, OU WJ, HUANG JF, et al. Circadian misalignment rather than sleep duration is associated with MAFLD: A population-based propensity score-matched study[J]. Nat Sci Sleep, 2021, 13: 103- 111. DOI: 10.2147/NSS.S290465. [14] WANG T, JIANG YY, WANG XW, et al. Effect of different diet and exercise strategies on patients with nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2020, 36( 2): 437- 441. DOI: 10.3969/j.issn.1001-5256.2020.02.045.汪涛, 蒋元烨, 王学伟, 等. 不同饮食及运动方案对非酒精性脂肪性肝病患者的影响[J]. 临床肝胆病杂志, 2020, 36( 2): 437- 441. DOI: 10.3969/j.issn.1001-5256.2020.02.045. [15] KWAK MS, KIM D. Non-alcoholic fatty liver disease and lifestyle modifications, focusing on physical activity[J]. Korean J Intern Med, 2018, 33( 1): 64- 74. DOI: 10.3904/kjim.2017.343. -



 PDF下载 ( 812 KB)
PDF下载 ( 812 KB)

 下载:
下载:


