髓系细胞触发受体1(TREM-1)在肝硬化腹水合并腹腔感染患者中的表达及其预后价值
DOI: 10.12449/JCH250517
Expression and prognostic value of triggering receptor expressed on myeloid cells-1 in patients with cirrhotic ascites and intra-abdominal infection
-
摘要:
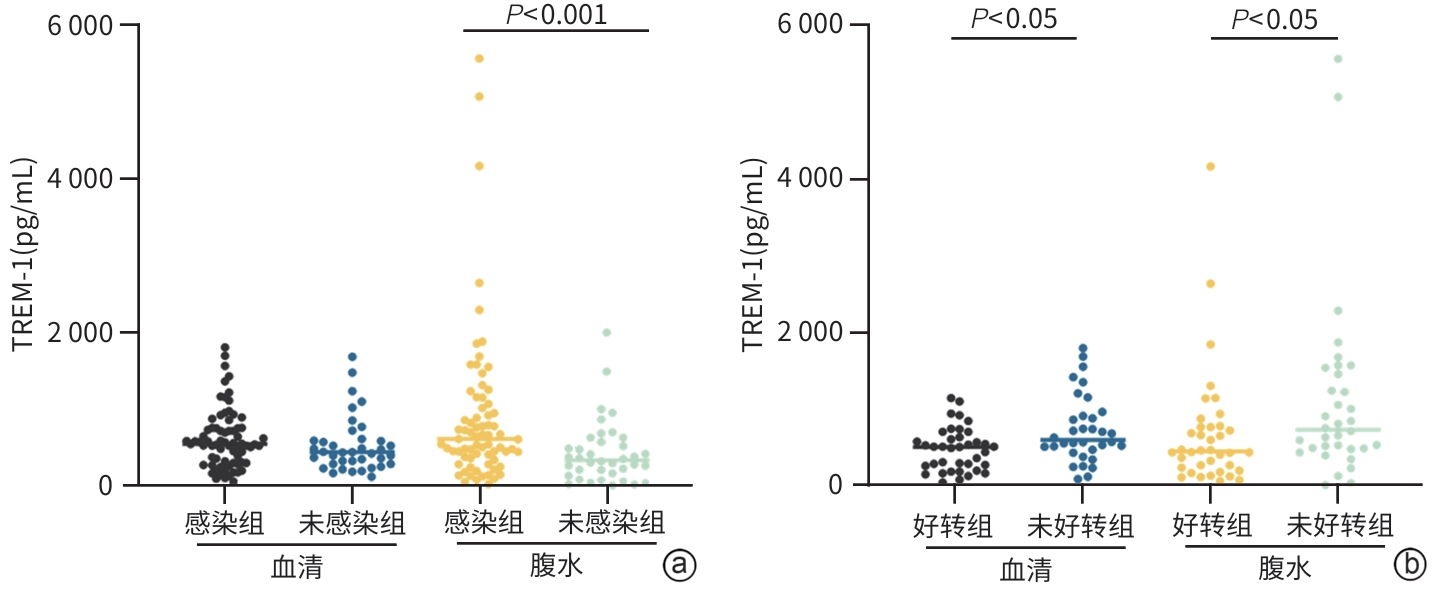
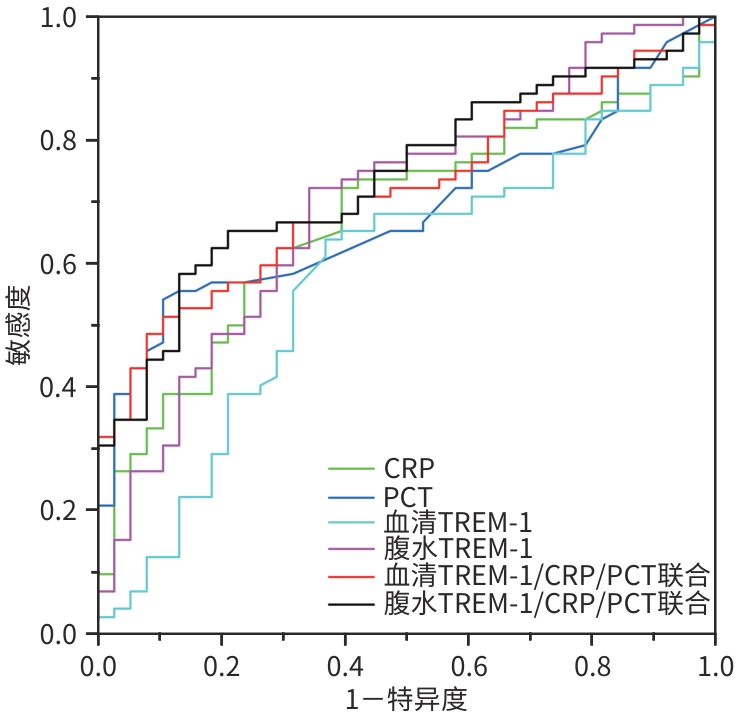
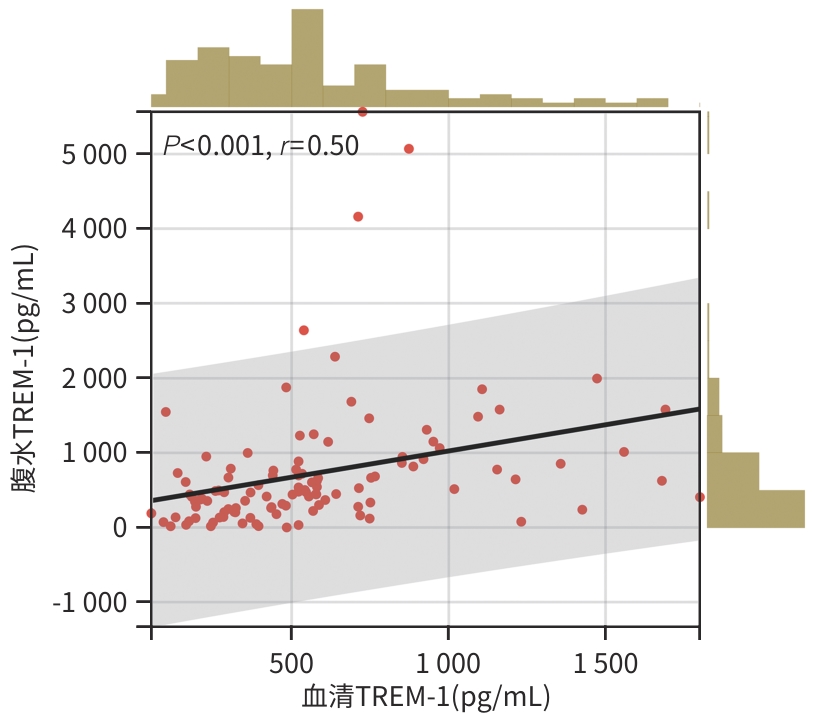
目的 分析肝硬化腹水患者血清和腹水中髓系细胞触发受体1(TREM-1)的表达水平,并探讨其与临床特征、炎症标志物的相关性,以及TREM-1在感染诊断和预后中的作用。 方法 选取2019年1月—2020年12月在石家庄市第五医院住院治疗的肝硬化腹水患者110例,根据腹腔感染情况分为感染组(n=72)和未感染组(n=38);在合并感染的患者中,根据预后情况将其分为好转组(n=38)与未好转组(n=34)。收集患者的临床资料及实验室检查指标。采集血清和腹水,应用酶联免疫吸附试验检测TREM-1水平。正态分布的计量资料两组间比较采用成组t检验;非正态分布的计量资料两组间比较采用Mann-Whitney U检验,多组间比较采用Kruskal-Wallis H检验。计数资料两组间比较采用χ2检验。各项指标之间的相关性采用Spearman相关分析。采用多因素Logistic回归分析影响肝硬化腹水合并感染患者预后的因素,受试者操作特征曲线(ROC曲线)评价各项指标的诊断和预后预测效能,并用Delong检验比较ROC曲线下面积(AUC)之间的差异。 结果 腹水和血清中的TREM-1水平存在显著正相关(r=0.50,P<0.001)。未好转组患者腹水TREM-1(Z=-2.391,P=0.017)和血清TREM-1(Z=-2.544,P=0.011)水平均明显高于好转组;感染组患者腹水TREM-1水平显著高于未感染组(Z=-3.420,P<0.001),而血清TREM-1在两组之间差异无统计学意义(P>0.05)。血清和腹水TREM-1水平与C反应蛋白(CRP)、降钙素原(PCT)、白细胞计数及中性粒细胞/淋巴细胞比值呈显著正相关(r值分别为0.288、0.344、0.530、0.510、0.534、0.454、0.330、0.404,P值均<0.05)。ROC曲线分析显示,PCT、CRP与血清或腹水TREM-1三者联合应用诊断肝硬化腹水合并感染时,AUC分别达0.715和0.740。多因素Logistic回归分析表明,CRP(OR=1.019,95%CI:1.001~1.038,P=0.043)和血清TREM-1(OR=1.002,95%CI:1.000~1.003,P=0.016)是影响肝硬化腹水合并腹腔感染患者预后的独立危险因素,两者联合预测不良预后的AUC为0.728。 结论 肝硬化腹水患者的TREM-1水平与感染程度及预后密切相关。联合检测TREM-1与CRP和PCT可提高对感染诊断的准确性,并有助于评估患者预后。 Abstract:Objective To analyze the expression level of triggering receptor expressed on myeloid cells-1 (TREM-1) in serum and ascites of patients with cirrhotic ascites, and to investigate its correlation with clinical features and inflammatory markers and its role in the diagnosis of infection and prognostic evaluation. Methods A total of 110 patients with cirrhotic ascites who were hospitalized in The Fifth Hospital of Shijiazhuang from January 2019 to December 2020 were enrolled, and according to the presence or absence of intra-abdominal infection, they were divided into infection group with 72 patients and non-infection group with 38 patients. The patients with infection were further divided into improvement group with 38 patients and non-improvement group with 34 patients. Clinical data and laboratory markers were collected from all patients. Serum and ascites samples were collected, and ELISA was used to measure the level of TREM-1. The independent-samples t test was used for comparison of normally distributed continuous data between two groups; the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups, and the Kruskal-Wallis H test was used for comparison between multiple groups; the chi-square test was used for comparison of categorical data between two groups. A Spearman correlation analysis was used to investigate the correlation between indicators. A multivariate Logistic regression analysis was used to identify the influencing factors for the prognosis of patients with cirrhotic ascites and infection. The receiver operating characteristic (ROC) curve was used to evaluate the diagnostic and prognostic efficacy of each indicator, and the Delong test was used for comparison of the area under the ROC curve (AUC). Results The level of TREM-1 in ascites was significantly positively correlated with that in serum (r=0.50, P<0.001). Compared with the improvement group, the non-improvement group had a significantly higher level of TREM-1 in ascites (Z=-2.391, P=0.017) and serum (Z=-2.544, P=0.011), and compared with the non-infection group, the infection group had a significantly higher level of TREM-1 in ascites (Z=-3.420, P<0.001), while there was no significant difference in the level of TREM-1 in serum between the two groups (P>0.05). The level of TREM-1 in serum and ascites were significantly positively correlated with C-reactive protein (CRP), procalcitonin (PCT), white blood cell count, and neutrophil-lymphocyte ratio (r=0.288, 0.344, 0.530, 0.510, 0.534, 0.454, 0.330, and 0.404, all P<0.05). The ROC curve analysis showed that when PCT, CRP, and serum or ascitic TREM-1 were used in combination for the diagnosis of cirrhotic ascites with infection, the AUCs were 0.715 and 0.740, respectively. The multivariate Logistic regression analysis showed that CRP (odds ratio [OR]=1.019, 95% confidence interval [CI]: 1.001 — 1.038, P=0.043) and serum TREM-1 (OR=1.002, 95%CI: 1.000 — 1.003, P=0.016) were independent risk factors for the prognosis of patients with cirrhotic ascites and infection, and the combination of these two indicators had an AUC of 0.728 in predicting poor prognosis. Conclusion The level of TREM-1 is closely associated with the severity of infection and prognosis in patients with cirrhotic ascites, and combined measurement of TREM-1 and CRP/PCT can improve the diagnostic accuracy of infection and provide support for prognostic evaluation. -
Key words:
- Liver Cirrhosis /
- Ascites /
- Infections /
- Triggering Receptor Expressed on Myeloid Cells-1 /
- Diagnosis /
- Prognosis
-
表 1 不同临床特征患者TREM-1表达水平比较
Table 1. Comparison of TREM-1 levels in patients with different clinical characteristics
项目 例数 血清 腹水 TREM-1(pg/mL) 统计值 P值 TREM-1(pg/mL) 统计值 P值 性别 Z=-0.933 0.351 Z=-1.102 0.270 男 94 521.76(303.96~713.35) 492.83(271.05~869.85) 女 16 608.14(249.29~1 096.90) 426.02(121.91~801.73) 年龄 Z=-1.664 0.096 Z=-0.276 0.780 <50岁 31 484.06(257.04~554.57) 489.31(262.52~788.81) ≥50岁 79 545.37(320.48~765.29) 475.44(239.16~864.63) 发现原发病时间 H=3.042 0.385 H=0.942 0.815 ≤1年 63 521.76(270.13~711.71) 489.31(261.14~788.81) 1~3年 22 455.72(284.27~695.36) 457.38(226.28~704.16) >3~5年 7 545.37(317.03~725.81) 527.65(208.69~914.94) >5年 18 605.78(357.66~1 067.65) 646.03(319.46~1 014.80) 原发病来源 H=0.328 0.849 H=0.244 0.885 病毒性肝炎 69 521.76(290.40~749.42) 489.31(206.36~796.84) 非病毒性肝炎 27 538.68(285.04~852.76) 445.88(262.52~945.70) 两种混合 14 521.76(303.89~609.11) 516.85(295.04~950.97) 合并症 Z=-0.375 0.708 Z=-1.169 0.242 有 59 525.88(298.88~750.57) 514.81(293.16~885.51) 无 51 502.44(305.84~689.95) 441.70(179.13~776.36) 并发肝硬化相关症状 Z=-2.250 0.024 Z=-3.094 0.002 有 65 564.24(336.78~808.02) 625.14(325.65~1 038.06) 无 45 435.67(253.20~585.45) 415.40(132.21~617.87) 表 2 血清和腹水TREM-1水平与炎症指标间的相关性
Table 2. The correlation between serum and ascites TREM-1 and inflammatory markers
检测指标 炎症指标 所有患者(n=110) 感染组(n=72) 未感染组(n=38) r值 P值 r值 P值 r值 P值 血清TREM-1(pg/mL) CRP(mg/L) 0.288 0.002 0.274 0.020 0.157 0.346 PCT(ng/L) 0.344 <0.001 0.280 0.017 0.521 0.001 WBC(×109/L) 0.530 <0.001 0.536 <0.001 0.492 0.002 NLR 0.510 <0.001 0.535 <0.001 0.371 0.022 腹水TREM-1(pg/mL) CRP(mg/L) 0.534 <0.001 0.547 <0.001 0.363 0.025 PCT(ng/L) 0.454 <0.001 0.427 <0.001 0.319 0.051 WBC(×109/L) 0.330 <0.001 0.233 0.049 0.273 0.097 NLR 0.404 <0.001 0.316 0.007 0.465 0.003 表 3 肝硬化合并腹腔感染患者预后好转组与未好转组间各项指标比较
Table 3. Comparison of various indicators between the improved-patients and non-improved patients with liver cirrhosis complicated with abdominal infection
项目 好转组(n=38) 未好转组(n=34) 统计值 P值 年龄(岁) 55.605±11.558 58.059±13.191 t=-0.841 0.403 性别[例(%)] χ2=1.305 0.253 男 33(86.84) 26(76.47) 女 5(13.16) 8(23.53) 原发病来源[例(%)] χ2=5.114 0.078 病毒性肝炎 20(52.63) 25(73.53) 非病毒性肝炎 13(34.21) 4(11.76) 两种混合 5(13.16) 5(11.71) 除腹水外其他并发症[例(%)] χ2=5.678 0.017 有 20(52.63) 27(79.41) 无 18(47.37) 7(20.59) 合并症[例(%)] χ2=1.939 0.164 有 23(60.53) 15(44.12) 无 15(39.47) 19(55.88) WBC(×109/L) 4.990(3.560~7.193) 6.145(4.570~9.243) Z=-1.963 0.050 中性粒细胞百分比(%) 71.650(63.675~78.775) 80.450(73.800~83.475) Z=-2.826 0.005 淋巴细胞百分比(%) 17.500(9.525~24.075) 10.200(7.350~16.525) Z=-2.459 0.014 NLR 3.963(2.712~8.560) 7.774(4.658~11.408) Z=-2.515 0.012 单核细胞百分比(%) 7.300(6.125~9.850) 7.300(6.250~9.050) Z=-0.344 0.731 CRP(mg/L) 17.910(6.383~30.100) 29.770(17.350~66.570) Z=-2.577 0.010 PCT(ng/L) 0.185(0.058~0.505) 0.810(0.248~2.383) Z=-3.667 <0.001 腹水细胞数(×106/L) 86.500(49.500~525.000) 80.000(50.000~308.750) Z=-0.090 0.928 李凡他试验[例(%)] χ2=0.134 0.715 阳性 15(39.47) 12(35.29) 阴性 23(60.53) 22(64.71) ALT(U/L) 28.800(17.850~53.450) 74.150(32.625~99.675) Z=-3.407 0.001 AST(U/L) 48.000(30.750~92.575) 142.800(74.850~255.775) Z=-4.585 <0.001 TBil(μmol/L) 36.800(20.975~60.750) 94.800(33.625~203.200) Z=-2.984 0.003 IBil(μmol/L) 18.650(11.325~34.225) 70.900(19.700~150.175) Z=-3.311 0.001 ALP(U/L) 104.100(77.075~150.975) 143.500(93.825~224.275) Z=-2.335 0.020 GGT(U/L) 61.000(22.575~106.200) 115.250(46.075~274.075) Z=-2.527 0.012 尿素氮(mmol/L) 6.225(4.628~11.695) 8.625(6.305~13.988) Z=-1.805 0.071 肌酐(μmol/L) 80.450(59.500~109.375) 72.850(61.375~112.950) Z=-0.479 0.632 血清TREM-1(pg/mL) 517.875(254.694~659.001) 609.098(472.158~932.683) Z=-2.544 0.011 腹水TREM-1(pg/mL) 459.250(237.970~779.467) 741.361(494.582~1 483.407) Z=-2.391 0.017 -
[1] WANG YK, WANG MQ, LIU CR, et al. Global burden of liver cirrhosis 1990-2019 and 20 years forecast: Results from the global burden of disease study 2019[J]. Ann Med, 2024, 56( 1): 2328521. DOI: 10.1080/07853890.2024.2328521. [2] ZHANG XY, ZHAO JJ, LIANG Y, et al. Research progress on relationship between TREMs and ulcerative colitis and related carcinogenesis[J]. Chin J Immunol, 2023, 39( 1): 211- 214. DOI: 10.3969/j.issn.1000-484X.2023.01.035.张馨月, 赵俊佳, 梁媛, 等. 髓样细胞触发受体与溃疡性结肠炎及其相关癌变的研究进展[J]. 中国免疫学杂志, 2023, 39( 1): 211- 214. DOI: 10.3969/j.issn.1000-484X.2023.01.035. [3] RAO SZ, HUANG JS, SHEN ZJ, et al. Inhibition of TREM-1 attenuates inflammation and lipid accumulation in diet-induced nonalcoholic fatty liver disease[J]. J Cell Biochem, 2019, 120( 7): 11867- 11877. DOI: 10.1002/jcb.28468. [4] WU XJ, CAI B, LU W, et al. HBV upregulated triggering receptor expressed on myeloid cells-1(TREM-1) expression on monocytes participated in disease progression through NF-κB pathway[J]. Clin Immunol, 2021, 223: 108650. DOI: 10.1016/j.clim.2020.108650. [5] Chinese Society of Hepatology, Chinese Medical Association. Guidelines on the management of ascites and complications in cirrhosis[J]. J Clin Hepatol, 2017, 33( 10): 1847- 1863. DOI: 10.3969/j.issn.1001-5256.2017.10.003.中华医学会肝病学分会. 肝硬化腹水及相关并发症的诊疗指南[J]. 临床肝胆病杂志, 2017, 33( 10): 1847- 1863. DOI: 10.3969/j.issn.1001-5256.2017.10.003. [6] LI BL, CHEN JJ. Diagnosis and treatment of abdominal infection in patients with liver cirrhosis: Advances and challenges[J]. J Clin Hepatol, 2021, 37( 4): 757- 760. DOI: 10.3969/j.issn.1001-5256.2021.04.003.黎倍伶, 陈金军. 肝硬化腹腔感染的诊疗进展及挑战[J]. 临床肝胆病杂志, 2021, 37( 4): 757- 760. DOI: 10.3969/j.issn.1001-5256.2021.04.003. [7] ZHANG LL, HU JH, DAI XC, et al. Research progress on the relationship between cirrhotic ascites and intestinal mucosal barrier function[J/CD]. Chin J Liver Dis(Electronic Version), 2023, 15( 2): 23- 27. DOI: 10.3969/j.issn.1674-7380.2023.02.005.张丽丽, 胡建华, 代欣璨, 等. 肝硬化腹水与肠黏膜屏障功能关系研究进展[J/CD]. 中国肝脏病杂志(电子版), 2023, 15( 2): 23- 27. DOI: 10.3969/j.issn.1674-7380.2023.02.005. [8] SISKIND S, BRENNER M, WANG P. TREM-1 modulation strategies for sepsis[J]. Front Immunol, 2022, 13: 907387. DOI: 10.3389/fimmu.2022.907387. [9] JOLLY L, CARRASCO K, SALCEDO-MAGGUILLI M, et al. sTREM-1 is a specific biomarker of TREM-1 pathway activation[J]. Cell Mol Immunol, 2021, 18( 8): 2054- 2056. DOI: 10.1038/s41423-021-00733-5. [10] da SILVA-NETO PV, de CARVALHO JCS, PIMENTEL VE, et al. sTREM-1 predicts disease severity and mortality in COVID-19 patients: Involvement of peripheral blood leukocytes and MMP-8 activity[J]. Viruses, 2021, 13( 12): 2521. DOI: 10.3390/v13122521. [11] VANDESTIENNE M, BRAIK R, LAVILLEGRAND JR, et al. Soluble TREM-1 plasma levels are associated with acute kidney injury, acute atrial fibrillation and prolonged ICU stay after cardiac surgery- a proof-concept study[J]. Front Cardiovasc Med, 2023, 10: 1098914. DOI: 10.3389/fcvm.2023.1098914. [12] TREBICKA J, HERNAEZ R, SHAWCROSS DL, et al. Recent advances in the prevention and treatment of decompensated cirrhosis and acute-on-chronic liver failure(ACLF) and the role of biomarkers[J]. Gut, 2024, 73( 6): 1015- 1024. DOI: 10.1136/gutjnl-2023-330584. [13] CHANG W, PENG F, MENG SS, et al. Diagnostic value of serum soluble triggering expressed receptor on myeloid cells 1(sTREM-1) in suspected sepsis: A meta-analysis[J]. BMC Immunol, 2020, 21( 1): 2. DOI: 10.1186/s12865-020-0332-x. [14] QIN Q, LIANG LJ, XIA YQ. Diagnostic and prognostic predictive values of circulating sTREM-1 in sepsis: A meta-analysis[J]. Infect Genet Evol, 2021, 96: 105074. DOI: 10.1016/j.meegid.2021.105074. [15] XIA Y, WANG Y, HE HW, et al. Predictive value of white blood cell, procalcitonin and high-sensitivity C-reactive protein for the bloodstream infection in the super-elderly critically-ill patients[J]. Natl Med J China, 2019, 99( 5): 365- 369. DOI: 10.3760/cma.j.issn.0376-2491.2019.05.009.夏莹, 王颖, 何怀武, 等. 白细胞、降钙素原和超敏C反应蛋白在超高龄重症患者血流感染的诊断预测价值[J]. 中华医学杂志, 2019, 99( 5): 365- 369. DOI: 10.3760/cma.j.issn.0376-2491.2019.05.009. [16] YANG P, XIAO LY, YANG N, et al. The evaluation value of procalcitonin and prothrombin activity in the prognosis of liver failure complicated by infection[J]. Chin J Nosocomiol, 2022, 32( 4): 531- 534. DOI: 10.11816/cn.ni.2022-210509.杨平, 肖乐尧, 杨娜, 等. 降钙素原和凝血酶原活动度在肝衰竭合并感染预后中的评估价值[J]. 中华医院感染学杂志, 2022, 32( 4): 531- 534. DOI: 10.11816/cn.ni.2022-210509. [17] KANG MK, LEE YR, PARK SY, et al. Diagnostic performance of procalcitonin for bacterial infection in severe alcoholic hepatitis compared with C-reactive protein[J]. BMC Gastroenterol, 2024, 24( 1): 428. DOI: 10.1186/s12876-024-03519-x. [18] SUN HF, FENG JG, TANG LL. Function of TREM1 and TREM2 in liver-related diseases[J]. Cells, 2020, 9( 12): 2626. DOI: 10.3390/cells9122626. [19] COLONNA M. The biology of TREM receptors[J]. Nat Rev Immunol, 2023, 23( 9): 580- 594. DOI: 10.1038/s41577-023-00837-1. [20] LIN XY, LI C, ZHANG T, et al. Changes of intestinal wall barrier function and its correlation with susceptibility to infection in patients with cirrhotic portal hypertension[J]. Chin J Hepatol, 2023, 31( 1): 70- 76. DOI: 10.3760/cma.j.cn501113-20220118-00031.林晓宇, 李琛, 张婷, 等. 肝硬化门静脉高压症患者肠壁屏障功能的改变及其与易发感染的关系[J]. 中华肝脏病杂志, 2023, 31( 1): 70- 76. DOI: 10.3760/cma.j.cn501113-20220118-00031. -



 PDF下载 ( 1445 KB)
PDF下载 ( 1445 KB)

 下载:
下载: