慢性HBV感染自然史不同阶段的HBV RNA水平特征及其与HBV DNA、HBsAg的相关性分析
DOI: 10.12449/JCH250407
Features of HBV RNA level in different stages of the natural history of chronic hepatitis B virus infection and its correlation with HBV DNA and HBsAg
-
摘要:
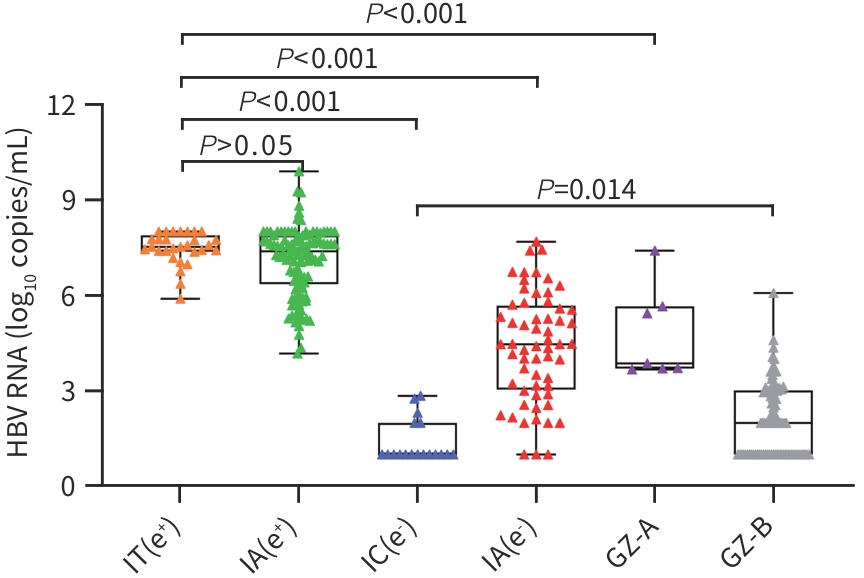
目的 观察未经抗病毒治疗的慢性HBV感染自然史不同阶段的血清HBV RNA特点及其与血清HBV DNA、HBsAg的相关性。 方法 选取2023年1月—2024年6月于山东大学第二医院感染性疾病/肝病科就诊且未经治疗的慢性HBV感染者306例,根据自然史不同阶段分为6组:HBeAg阳性慢性HBV感染者29例、HBeAg阳性慢性乙型肝炎(CHB)患者107例、HBeAg阴性慢性HBV感染者18例、HBeAg阴性CHB患者60例、HBeAg阳性或阴性慢性HBV感染不确定期感染者分别7例和85例。采用RNA实时荧光恒温扩增检测技术进行血清高敏HBV RNA定量检测。计量资料多组间比较采用Kruskal-Wallis H检验,两组间比较采用Mann-Whitney U检验。采用Spearman法分析HBV RNA与HBV DNA、HBsAg的相关性。 结果 血清HBV RNA水平在HBeAg阳性慢性HBV感染者、HBeAg阳性CHB患者、HBeAg阴性CHB患者及HBeAg阴性慢性HBV感染者中递减,依次为7.5(7.4~7.9)、7.4(6.4~7.9)、4.5(3.0~5.7)、1.0(1.0~2.0)log10 copies/mL;HBeAg阳性慢性HBV感染不确定期患者的血清HBV RNA水平为3.9(3.7~5.7)log10 copies/mL;HBeAg阴性慢性HBV感染不确定期患者的血清HBV RNA水平为2.0(1.0~3.0)log10 copies/mL,6组间血清HBV RNA水平有统计学差异(H=830.770,P<0.001)。除与HBeAg阳性CHB组无统计学差异外,HBeAg阳性慢性HBV感染组HBV RNA水平与其他各组的差异均有统计学意义(P值均<0.001)。306例HBV感染者中,HBV RNA与HBV DNA呈强相关(r=0.92,P<0.001),与HBsAg中度相关(r=0.67,P<0.001)。在HBeAg阳性者中,血清HBV RNA与HBsAg的相关性(r=0.61,P<0.001)强于HBeAg阴性者(r=0.31,P<0.001)。在HBeAg阳性慢性HBV感染者中,ALT>30 U/L的男性及ALT>19 U/L的女性感染者血清HBV RNA的水平显著低于ALT≤30 U/L的男性及ALT≤19 U/L的女性感染者(P<0.001),但与HBeAg阳性CHB患者HBV RNA水平更为相近,差异无统计学意义(P>0.05)。 结论 在未经抗病毒治疗的慢性HBV感染者中,血清HBV RNA水平在自然史的不同阶段存在差异,其与HBV DNA的相关性最强,而与HBsAg的相关性较弱。在HBeAg阳性慢性HBV感染者中,ALT>30 U/L的男性及ALT>19 U/L的女性感染者血清HBV RNA水平处于HBeAg阳性慢性HBV感染和HBeAg阳性CHB的过渡阶段。 Abstract:Objective To investigate the features of serum HBV RNA in different stages of the natural history of chronic hepatitis B virus (HBV) infection without antiviral treatment, as well as its correlation with serum HBV DNA and HBsAg. Methods A total of 306 treatment-naïve patients with chronic HBV infection who attended Department of Infections Diseases and Hepatoloty, the Second Hospital of Shandong University from January 2023 to June 2024 were divided into six groups based on the different stages of natural history, i.e., HBeAg-positive chronic HBV infection group with 29 patients, HBeAg-positive chronic hepatitis B (CHB) group with 107 patients, HBeAg-negative chronic HBV infection group with 18 patients, HBeAg-negative CHB group with 60 patients, HBeAg-positive indeterminate-phase chronic HBV infection group with 7 patients, and HBeAg-negative indeterminate-phase chronic HBV infection group with 85 patients. Real-time isothermal RNA amplification was used to measure serum high-sensitivity HBV RNA. The Kruskal-Wallis H test was used for comparison between multiple groups of continuous data, while the Mann-Whitney U test was used for comparison between two groups. The Spearman method was used to investigate the correlation of HBV RNA with HBV DNA and HBsAg. Results The HBeAg-positive chronic HBV infection group showed the highest level of serum HBV RNA [7.5 (7.4 — 7.9) log10 copies/mL], followed by the HBeAg-positive CHB group [7.4 (6.4 — 7.9) log10 copies/mL], the HBeAg-negative CHB group [4.5 (3.0 — 5.7) log10 copies/mL], and the HBeAg-negative chronic HBV infection group [1.0 (1.0 — 2.0) log10 copies/mL]; the HBeAg-positive indeterminate-phase chronic HBV infection group had a serum HBV RNA level of 3.9 (3.7 — 5.7) log10 copies/mL, and the HBeAg-negative indeterminate-phase chronic HBV infection group had a serum HBV RNA level of 2.0 (1.0 — 3.0) log10 copies/mL; there was a significant difference in serum HBV RNA level between the six groups (H=830.770, P<0.001). There was a significant difference in HBV RNA level between the HBeAg-positive chronic HBV infection group and all the other groups except the HBeAg-positive CHB group (all P<0.001). In the 306 patients with HBV infection, HBV RNA was strongly correlated with HBV DNA (r=0.92, P<0.001) and was moderately correlated with HBsAg (r=0.67, P<0.001). The correlation between serum HBV RNA and HBsAg in HBeAg-positive patients (r=0.61, P<0.001) was stronger than that in HBeAg-negative patients (r=0.31, P<0.001). For the patients with HBeAg-positive chronic HBV infection, the male patients with ALT>30 U/L and the female patients with ALT>19 U/L had a significantly lower serum HBV RNA level than the male patients with ALT≤30 U/L and the female patients with ALT≤19 U/L (P<0.001), and there was no significant difference in serum HBV RNA level between the latter group of patients and the HBeAg-positive CHB group (P>0.05). Conclusion In patients with chronic HBV infection who do not receive antiviral therapy, there is a difference in serum HBV RNA level in different stages of natural history, and serum HBV RNA level has the strongest correlation with HBV DNA and a relatively weak correlation with HBsAg. In patients with HBeAg-positive chronic HBV infection, serum HBV RNA level in male patients with ALT>30 U/L and female patients with ALT>19 U/L are in the transition stage between HBeAg-positive chronic HBV infection and HBeAg-positive CHB. -
Key words:
- Hepatitis B Virus /
- Hepatitis B, Chronic /
- HBV RNA
-
表 1 所有患者一般资料及临床特征
Table 1. Demographic and clinical characteristics of patients
项目 HBeAg阳性慢性HBV感染组(n=29) HBeAg阳性CHB组(n=107) HBeAg阴性慢性HBV感染组(n=18) HBeAg阴性CHB组(n=60) HBeAg阳性慢性HBV感染不确定期组(n=7) HBeAg阴性慢性HBV感染不确定期组(n=85) H值 P值 男性[例(%)] 10(34) 69(64) 9(50) 33(55) 4(57) 42(49) 年龄(岁) 38(33~43) 37(31~45) 45(32~56) 42(35~54) 37(34~50) 39(35~48) 72.493 <0.001 ALT(U/L) 20(17~32) 144(76~296) 20(11~22) 127(73~244) 28(16~32) 22(16~29) 939.846 <0.001 AST(U/L) 19
(17~28)
93(51~193) 19(16~22) 73(45~139) 19(17~26) 19(17~24) 849.888 <0.001 ALB(g/L) 44.9
(42.4~47.1)
45.5(40.6~47.6) 47.3(45.2~48.5) 45.0(42.2~48.6) 47.3(46.1~49.3) 47.0(45.5~48.8) 59.351 <0.001 PLT(×109/L) 268(215~304) 194(153~239) 230(141~265) 185(133~230) 246(223~260) 213(175~248) 202.619 <0.001 HBV RNA(log10 copies/mL) 7.5(7.4~7.9) 7.4(6.4~7.9) 1.0
(1.0~2.0)
4.5(3.0~5.7) 3.9(3.7~5.7) 2.0(1.0~3.0) 830.770 <0.001 HBV DNA(log10 IU/mL) 8.2(8.2~8.3) 7.8(6.9~8.2) 1.3(1.0~1.3) 5.8(4.5~6.5) 4.5(3.8~5.3) 2.6(2.2~3.4) 1 033.335 <0.001 HBeAg(log10 S/Co) 3.1(3.1~3.2) 2.8(2.1~3.2) NA NA 1.0(1.0~3.1) NA HBsAg(log10 IU/mL) 4.6(4.5~4.7) 3.9(3.3~4.4) 2.1(1.0~3.2) 3.3(3.0~3.6) 3.8(3.3~4.6) 3.4(2.9~4.0) 511.413 <0.001 注:NA表示不适用。
-
[1] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B(version 2022)[J]. Infect Dis Info, 2023, 36( 1): 1- 17. DOI: 10.3969/j.issn.1007-8134.2023.01.01.中华医学会肝病学分会, 中华医学会感染病学分会. 慢性乙型肝炎防治指南(2022年版)[J]. 传染病信息, 2023, 36( 1): 1- 17. DOI: 10.3969/j.issn.1007-8134.2023.01.01. [2] Chinese Society of Infectious Diseases, Chinese Medical Association, Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B(version 2019)[J]. J Clin Hepatol, 2019, 35( 12): 2648- 2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007.中华医学会感染病学分会, 中华医学会肝病学分会. 慢性乙型肝炎防治指南(2019年版)[J]. 临床肝胆病杂志, 2019, 35( 12): 2648- 2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007. [3] TERRAULT NA, LOK ASF, MCMAHON BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance[J]. Hepatology, 2018, 67( 4): 1560- 1599. DOI: 10.1002/hep.29800. [4] European Association for the Study of the Liver. EASL 2017 clinical practice guidelines on the management of hepatitis B virus infection[J]. J Hepatol, 2017, 67( 2): 370- 398. DOI: 10.1016/j.jhep.2017.03.021. [5] SARIN SK, KUMAR M, LAU GK, et al. Asian-Pacific clinical practice guidelines on the management of hepatitis B: A 2015 update[J]. Hepatol Int, 2016, 10( 1): 1- 98. DOI: 10.1007/s12072-015-9675-4. [6] WANG ML, LIAO J, YE F, et al. Distribution and factors associated with serum HBV pregenomic RNA levels in Chinese chronic hepatitis B patients[J]. J Med Virol, 2021, 93( 6): 3688- 3696. DOI: 10.1002/jmv.26529. [7] GHANY MG, KING WC, LISKER-MELMAN M, et al. Comparison of HBV RNA and hepatitis B core related antigen with conventional HBV markers among untreated adults with chronic hepatitis B in North America[J]. Hepatology, 2021, 74( 5): 2395- 2409. DOI: 10.1002/hep.32018. [8] ZHANG XJ, HUA L/Y), JIN QF, et al. Correlation between HBV RNA and HBV virological markers and liver function indexes in patients with chronic HBV infection[J/OL]. China Ind Econ, 2024: 1- 5.( 2024-04-11). http://kns.cnki.net/KCMS/detail/detail.aspx?filename=ZHYY20240409004&dbname=CJFD&dbcode=CJFQ. http://kns.cnki.net/KCMS/detail/detail.aspx?filename=ZHYY20240409004&dbname=CJFD&dbcode=CJFQ张晓晶, 华乐, 金巧菲, 等. 慢性HBV感染者HBV RNA与乙肝病毒学标志物及肝功能指标的相关性[J/OL]. 中华医院感染学杂志, 2024: 1- 5.( 2024-04-11). http://kns.cnki.net/KCMS/detail/detail.aspx?filename=ZHYY20240409004&dbname=CJFD&dbcode=CJFQ. http://kns.cnki.net/KCMS/detail/detail.aspx?filename=ZHYY20240409004&dbname=CJFD&dbcode=CJFQ [9] WOODDELL CI, YUEN MF, CHAN HL, et al. RNAi-based treatment of chronically infected patients and chimpanzees reveals that integrated hepatitis B virus DNA is a source of HBsAg[J]. Sci Transl Med, 2017, 9( 409): eaan0241. DOI: 10.1126/scitranslmed.aan0241. [10] van CAMPENHOUT MJH, van BÖMMEL F, PFEFFERKORN M, et al. Host and viral factors associated with serum hepatitis B virus RNA levels among patients in need for treatment[J]. Hepatology, 2018, 68( 3): 839- 847. DOI: 10.1002/hep.29872. [11] TESTONI B, SCHOLTÈS C, PLISSONNIER ML, et al. Quantification of circulating HBV RNA expressed from intrahepatic cccDNA in untreated and NUC treated patients with chronic hepatitis B[J]. Gut, 2024, 73( 4): 659- 667. DOI: 10.1136/gutjnl-2023-330644. [12] ZHOU J, WANG FD, WANG ML, et al. Antiviral therapy for chronic HBV infection with persistently normal alanine aminotransferase: Controversy and consensus[J]. Front Med(Lausanne), 2021, 8: 717125. DOI: 10.3389/fmed.2021.717125. [13] TAN Y, YE Y, ZHOU X, et al. Age as a predictor of significant fibrosis features in HBeAg-negative chronic hepatitis B virus infection with persistently normal alanine aminotransferase[J]. PLoS One, 2015, 10( 4): e0123452. DOI: 10.1371/journal.pone.0123452. [14] LI Q, ZHOU Y, HUANG C, et al. A novel diagnostic algorithm to predict significant liver inflammation in chronic hepatitis B virus infection patients with detectable HBV DNA and persistently normal alanine transaminase[J]. Sci Rep, 2018, 8( 1): 15449. DOI: 10.1038/s41598-018-33412-z. [15] PRATI D, TAIOLI E, ZANELLA A, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels[J]. Ann Intern Med, 2002, 137( 1): 1- 10. DOI: 10.7326/0003-4819-137-1-200207020-00006. [16] KEEFFE EB, DIETERICH DT, HAN SB, et al. A treatment algorithm for the management of chronic hepatitis B virus infection in the United States: 2008 update[J]. Clin Gastroenterol Hepatol, 2008, 6( 12): 1315- 1341; quiz1286. DOI: 10.1016/j.cgh.2008.08.021. -



 PDF下载 ( 1368 KB)
PDF下载 ( 1368 KB)

 下载:
下载:




