60岁以上原发性肝癌患者术后谵妄发生风险预测模型的构建及验证
DOI: 10.12449/JCH240916
Construction and validation of a risk prediction model for postoperative delirium in primary liver cancer patients aged 60 years or older
-
摘要:
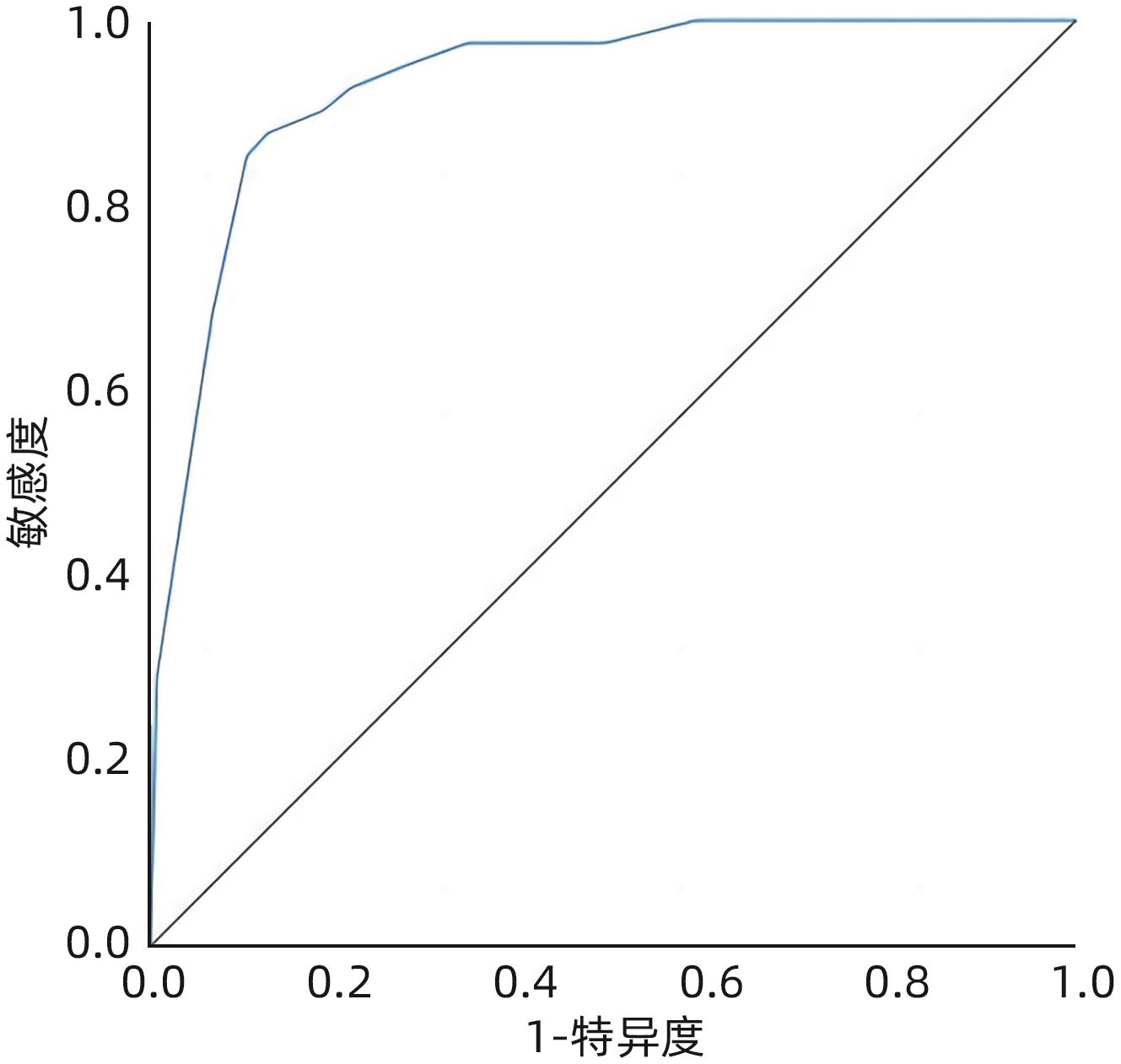
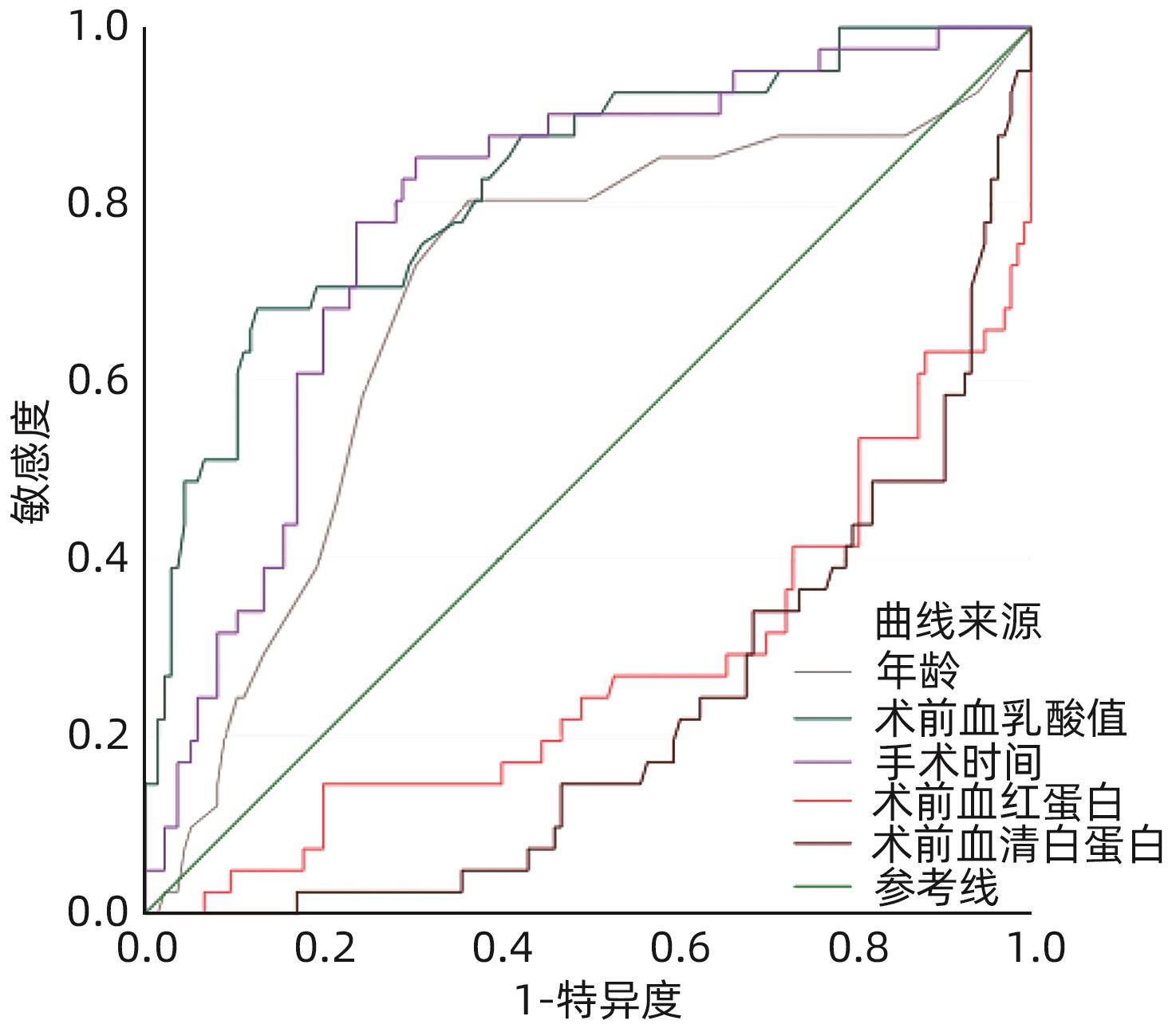
目的 分析构建老年原发性肝癌患者术后谵妄发生风险预测模型,并验证其应用价值。 方法 采用回顾性分析方式,选择2020年3月—2023年1月武汉科技大学附属天佑医院收治的老年原发性肝癌患者175例,记录患者术后谵妄发生率,并就可能影响谵妄发生的各因素进行单因素及多因素回归分析,构建其预测模型,并对该预测模型的临床应用价值进行验证分析。计量资料两组间比较采用成组t检验,计数资料两组间比较采用χ2检验,对可能影响老年原发性肝癌患者谵妄发生的各因素进行单因素及多因素Logistic回归分析,采用ROC曲线分析模型对患者谵妄发生的预测价值。 结果 175例老年原发性肝癌患者中,发生术后谵妄患者41例,发生率为23.43%。单因素分析结果显示,年龄、合并两种以上基础疾病、肝功能Child-Pugh分级、术前血乳酸值、手术时间、术前血红蛋白以及术前血清白蛋白与患者术后谵妄发生有关(t=3.534,χ2=12.000,χ2=4.938,t=7.561,t=5.768,t=5.141,t=6.148,P值均<0.05)。对上述单因素分析具有统计学意义的各因素进行多因素Logistic回归分析结果显示,手术时间、术前血红蛋白、术前血清白蛋白以及年龄进入回归模型(P值均<0.05),为影响老年原发性肝癌患者术后谵妄发生的独立危险因素。根据多因素Logistic回归分析结果,构建老年原发性肝癌术后谵妄预测模型:-2.222+3.678×手术时间-2.441×术前血红蛋白-3.904×术前血清白蛋白+1.807×年龄。对上述预测模型的预测效果进行分析,该模型ROC曲线下面积为0.931(P<0.001,95%CI:0.890~0.971),最佳截断值为-1.604(敏感度为87.80%,特异度为87.30%)。前瞻性纳入2023年2月—2023年6月在武汉科技大学附属天佑医院行根治性治疗手术的老年原发性肝癌患者56例进行模型验证,根据上述建立的风险预测模型,其中高危组患者14例,低危组42例,高危组患者术后谵妄发生率显著高于低危组(71.43% vs 11.90%,χ2=16.056,P<0.05)。 结论 年龄、手术时间、术前血清白蛋白以及术前血红蛋白是影响老年原发性肝癌患者术后谵妄发生的重要因素,根据上述因素拟定相应的风险预测模型,且该模型预测效果良好,值得进一步深入分析。 -
关键词:
- 肝肿瘤 /
- 肝切除术 /
- 谵妄 /
- 老年人 /
- Logistic模型
Abstract:Objective To construct a risk prediction model for postoperative delirium in elderly patients with primary liver cancer, and to validate its application value. Methods A retrospective analysis was performed for 175 elderly patients with primary liver cancer who were admitted to Tianyou Hospital Affiliated to Wuhan University of Science and Technology from March 2020 to January 2023. The incidence rate of postoperative delirium was recorded, and the univariate and multivariate regression analyses was performed for factors that may affect the onset of delirium. A prediction model was constructed, and the clinical application value of the prediction model was analyzed and validated. The independent-samples t test was used for comparison of continuous data between two groups, and the chi-square test was used for comparison of categorical data between two groups. The univariate and multivariate logistic regression analyses were performed for factors that may affect the onset of delirium in elderly patients with primary liver cancer, and the receiver operating characteristic (ROC) curve was used to investigate the value of the model in predicting the onset of delirium. Results Among the 175 elderly patients with primary liver cancer, 41 experienced postoperative delirium, with an incidence rate of 23.43%. The univariate analysis showed that age, presence of more than two underlying diseases, Child-Pugh class of liver function, preoperative blood lactate, time of operation, preoperative hemoglobin, and preoperative serum albumin were associated with the onset of postoperative delirium (t=3.534, χ2=12.000, χ2=4.938, t=7.561, t=5.768, t=5.141, t=6.148, P<0.05). The multivariate logistic regression analysis of the factors with statistical significance in the univariate analysis showed that time of operation, preoperative hemoglobin, preoperative serum albumin, and age were included in the regression model (P<0.05), and they were independent risk factors for the onset of postoperative delirium in elderly patients with primary liver cancer. According to the results of the multivariate logistic regression analysis, a prediction model for postoperative delirium in elderly patients with primary liver cancer was constructed as follows: -2.222+3.678×time of operation-2.441×preoperative hemoglobin-3.904×preoperative serum albumin+1.807×age. The prediction performance of this model was analyzed, with an area under the ROC curve of 0.931 (95% confidence interval: 0.890 — 0.971, P<0.001) and an optimal cut-off value of -1.604 (with a sensitivity of 87.80% and a specificity of 87.30%). A total of 56 elderly patients with primary liver cancer who underwent radical surgery in Tianyou Hospital Affiliated to Wuhan University of Science and Technology from February 2023 to June 2023 were enrolled in a prospective study for model validation. According to the above risk prediction model, there were 14 patients in the high-risk group and 42 patients in the low-risk group, and the high-risk group had a significantly higher incidence rate of postoperative delirium than the low-risk group (71.43% vs 11.90%, χ²=16.056, P<0.05). Conclusion Age, time of operation, preoperative serum albumin, and preoperative hemoglobin are important influencing factors for the onset of postoperative delirium in elderly patients with primary liver cancer. The risk prediction model based on these factors has a good prediction performance, which holds promise for further in-depth research. -
Key words:
- Liver Neoplasms /
- Hepatectomy /
- Delirious Speech /
- Aged /
- Logistic Models
-
表 1 老年原发性肝癌患者术后谵妄发生单因素分析
Table 1. Single factor analysis of postoperative delirium in elderly patients with primary liver cancer
因素 谵妄(n=41) 无谵妄(n=134) 统计值 P值 性别(例) χ2=0.048 0.827 男 24 81 女 17 53 年龄(岁) 71.95±6.48 67.78±6.65 t=3.534 0.001 BMI(kg/m2) 23.08±2.15 23.11±2.03 t=0.082 0.935 高血压(例) χ2=2.718 0.099 是 28 72 否 13 62 糖尿病(例) χ2=0.624 0.430 是 20 56 否 21 78 冠心病(例) χ2=0.035 0.852 是 14 35 否 27 99 合并2种以上基础疾病(例) χ2=12.000 <0.001 是 15 17 否 26 117 肿瘤大小(例) χ2=0.244 0.622 <5 cm 19 68 ≥5 cm 22 66 肿瘤位置(例) χ2=0.063 0.969 肝左叶 13 40 肝右叶 17 56 交界部位(例) 11 38 肿瘤个数(例) χ2=1.053 0.305 单发 29 83 多发 12 51 肝功能Child-Pugh分级(例) χ2=4.938 0.026 A级 19 88 B级 22 46 术前AFP(例) χ2=0.267 0.605 ≤400 μg/L 18 65 >400 μg/L 23 69 肝硬化(例) χ2=0.345 0.557 是 11 30 否 30 104 血管侵犯(例) χ2=0.093 0.761 是 17 52 否 24 82 术后病理分型(例) χ2=0.481 0.786 肝细胞癌 31 108 肝内胆管癌 8 21 混合细胞癌 2 5 术前血乳酸值(mmol/L) 2.73±0.42 2.19±0.41 t=7.561 <0.001 手术时间(min) 197.52±25.63 164.38±33.92 t=5.768 <0.001 手术切除方式(例) χ2=0.039 0.843 半肝切除 25 84 肝叶、局部切除 16 50 术前血红蛋白(g/L) 115.48±10.21 123.64±8.46 t=5.141 <0.001 术前血清白蛋白(g/L) 38.74±2.10 41.27±2.37 t=6.148 <0.001 表 2 谵妄与非谵妄患者连续变量ROC曲线参数
Table 2. Continuous variable ROC curve parameters for delirious and non-delirious patients
指标 AUC 截断值 P值 95%CI 年龄 0.695 69岁 <0.001 0.599~0.791 术前血乳酸值 0.824 2.575 mmol/L <0.001 0.749~0.899 手术时间 0.788 177.745 min <0.001 0.712~0.864 术前血红蛋白 0.270 118.725 g/L <0.001 0.174~0.366 术前血清白蛋白 0.217 40.145 g/L <0.001 0.142~0.293 表 3 多因素分析赋值表
Table 3. Multifactor analysis assignment table
因素 赋值 年龄 <69岁=0;≥69岁=1 合并2种以上基础疾病 无=0;有=1 肝功能Child-Pugh分级 A=0;B=1 术前血乳酸值 <2.575 mmol/L=0;≥2.575 mmol/L=1 手术时间 <177.745 min=0;≥177.745 min=1 术前血红蛋白 >118.725 g/L=0,≤118.725 g/L=1 术前血清白蛋白 >40.145 g/L=0,≤40.145 g/L=1 表 4 老年原发性肝癌患者术后谵妄多因素Logistic回归分析
Table 4. Multivariate Logistic regression analysis of postoperative delirium in elderly patients with primary liver cancer
因素 B值 SE Wald χ2 P值 OR 95%CI 常量 -2.222 0.829 7.189 0.007 手术时间 3.687 0.884 17.395 <0.001 39.935 7.060~225.882 术前血红蛋白 -2.441 0.748 10.638 0.001 0.870 0.020~0.378 术前血清白蛋白 -3.904 0.890 19.249 <0.001 0.020 0.004~0.115 年龄 1.807 0.716 6.373 0.012 6.092 1.498~24.779 -
[1] LUETZ A, GRUNOW JJ, MÖRGELI R, et al. Innovative ICU solutions to prevent and reduce delirium and post-intensive care unit syndrome[J]. Semin Respir Crit Care Med, 2019, 40( 5): 673- 686. DOI: 10.1055/s-0039-1698404. [2] WANG J, SHUANG PZ, ZHAO LB, et al. Risk factors of postoperative delirium in elderly patients undergoing hip fracture repair surgery[J]. J Clin Anesthesiol, 2023, 39( 3): 235- 240. DOI: 10.12089/jca.2023.03.002.王洁, 双鹏展, 赵龙彪, 等. 老年患者髋部骨折修复术后谵妄的危险因素[J]. 临床麻醉学杂志, 2023, 39( 3): 235- 240. DOI: 10.12089/jca.2023.03.002. [3] LI XP, WANG L, ZHANG H, et al. Construction and evaluation of a risk prediction model of postoperative delirium in patients with Stanford type A aortic dissection[J]. Chin J Nurs, 2022, 57( 8): 950- 957. DOI: 10.3761/j.issn.0254-1769.2022.08.009.李雪苹, 王磊, 张淮, 等. Stanford A型主动脉夹层患者术后谵妄风险预测评分模型的构建与效果验证[J]. 中华护理杂志, 2022, 57( 8): 950- 957. DOI: 10.3761/j.issn.0254-1769.2022.08.009. [4] YIN SL, SHI Y, CUI H, et al. Correlation between preoperative insomnia subtypes and postoperative delirium in elderly patients[J]. Anhui Med J, 2023, 44( 3): 314- 320. DOI: 10.3969/j.issn.1000-0399.2023.03.015.尹世梁, 施源, 崔虎, 等. 老年患者术前失眠障碍亚型与术后谵妄的相关性[J]. 安徽医学, 2023, 44( 3): 314- 320. DOI: 10.3969/j.issn.1000-0399.2023.03.015. [5] KRINITSKI D, KASINA R, KLÖPPEL S, et al. Associations of delirium with urinary tract infections and asymptomatic bacteriuria in adults aged 65 and older: A systematic review and meta-analysis[J]. J Am Geriatr Soc, 2021, 69( 11): 3312- 3323. DOI: 10.1111/jgs.17418. [6] BAHJI A, BACH P, DANILEWITZ M, et al. Comparative efficacy and safety of pharmacotherapies for alcohol withdrawal: A systematic review and network meta-analysis[J]. Addiction, 2022, 117( 10): 2591- 2601. DOI: 10.1111/add.15853. [7] National Health and Family Planning Commission, People’s Republic of China. Diagnosis, management, and treatment of hepatocellular carcinoma(V2017)[J]. J Clin Hepatol, 2017, 33( 8): 1419- 1431. DOI: 10.3969/j.issn.1001-5256.2017.08.003.中华人民共和国国家卫生和计划生育委员会. 原发性肝癌诊疗规范(2017年版)[J]. 临床肝胆病杂志, 2017, 33( 8): 1419- 1431. DOI: 10.3969/j.issn.1001-5256.2017.08.003. [8] MARGIOTTA A, BIANCHETTI A, RANIERI P, et al. Clinical characteristics and risk factors of delirium in demented and not demented elderly medical inpatients[J]. J Nutr Health Aging, 2006, 10( 6): 535- 539. [9] LIU QG, SONG T, WANG HH. Re-understanding of surgical resection techniques for liver cancer[J]. Chin J Dig Surg, 2024, 23( 1): 75- 79. DOI: 10.3760/cma.j.cn115610-20231214-00253.刘青光, 宋涛, 王欢欢. 肝癌外科手术切除技术的再认识[J]. 中华消化外科杂志, 2024, 23( 1): 75- 79. DOI: 10.3760/cma.j.cn115610-20231214-00253. [10] XU R, HUA Z. Epidemiological characteristics, risk factors and related preventive intervention strategies for cirrhosis complicated with primary liver cancer[J]. Chin J Integr Tradit West Med Liver Dis, 2020, 30( 4): 357- 359, 366. DOI: 10.3969/j.issn.1005-0264.2020.04.021.徐蓉, 华忠. 肝硬化并发原发性肝癌的流行病学特征、危险因素及相预防干预对策研究[J]. 中西医结合肝病杂志, 2020, 30( 4): 357- 359, 366. DOI: 10.3969/j.issn.1005-0264.2020.04.021. [11] ZHANG WL, LOU JS, SONG YX, et al. Research advances in application of biomarkers in diagnosis and treatment of postoperative delirium in elderly patients[J]. Acad J Chin PLA Med Sch, 2023, 44( 2): 197- 200. DOI: 10.3969/j.issn.2095-5227.2023.02.018.张伟丽, 娄景盛, 宋玉祥, 等. 生物标志物在老年患者术后谵妄诊疗中的应用综述[J]. 解放军医学院学报, 2023, 44( 2): 197- 200. DOI: 10.3969/j.issn.2095-5227.2023.02.018. [12] WILDES TS, MICKLE AM, ABDALLAH A BEN, et al. Effect of electroencephalography-guided anesthetic administration on postoperative delirium among older adults undergoing major surgery: The ENGAGES randomized clinical trial[J]. JAMA, 2019, 321( 5): 473- 483. DOI: 10.1001/jama.2018.22005. [13] XU YN, MA QQ, DU HM, et al. Postoperative delirium in neurosurgical patients: Recent insights into the pathogenesis[J]. Brain Sci, 2022, 12( 10): 1371. DOI: 10.3390/brainsci12101371. [14] YANG JJ, LEI L, QIU D, et al. Effect of remimazolam on postoperative delirium in older adult patients undergoing orthopedic surgery: A prospective randomized controlled clinical trial[J]. Drug Des Devel Ther, 2023, 17: 143- 153. DOI: 10.2147/DDDT.S392569. [15] SUMNER M, DENG C, EVERED L, et al. Processed electroencephalography-guided general anaesthesia to reduce postoperative delirium: A systematic review and meta-analysis[J]. Br J Anaesth, 2023, 130( 2): e243- e253. DOI: 10.1016/j.bja.2022.01.006. [16] WU D, LI JQ, YUAN H, et al. Effect of dexmedetomidine on postoperative delirium and cerebral oxygen metabolism in elderly patients undergoing pulmonary surgery[J]. China J Mod Med, 2022, 32( 14): 71- 76. DOI: 10.3969/j.issn.1005-8982.2022.14.013.吴迪, 李俊青, 袁浩, 等. 右美托咪定对老年肺部手术患者术后谵妄发生率、脑氧代谢的影响[J]. 中国现代医学杂志, 2022, 32( 14): 71- 76. DOI: 10.3969/j.issn.1005-8982.2022.14.013. [17] FU HM, ZHONG CC, ZHOU WW, et al. Effect of acute normovolemic hemodilution on postoperative delirium and inflammation in elderly patients undergoing total hip arthroplasty[J]. J Clin Anesthesiol, 2021, 37( 6): 583- 587. DOI: 10.12089/jca.2021.06.005.付慧敏, 钟超超, 周伟伟, 等. 急性等容血液稀释对老年患者全髋关节置换术后谵妄和炎症水平的影响[J]. 临床麻醉学杂志, 2021, 37( 6): 583- 587. DOI: 10.12089/jca.2021.06.005. [18] ZHANG H, LI SP. Analysis of the current status of delirium in elderly patients after hip replacement and its related influencing factors[J]. J Changchun Univ Chin Med, 2022, 38( 10): 1155- 1159. DOI: 10.13463/j.cnki.cczyy.2022.10.022.张宏, 李淑萍. 老年患者髋关节置换术后谵妄的发生现状及其相关影响因素分析[J]. 长春中医药大学学报, 2022, 38( 10): 1155- 1159. DOI: 10.13463/j.cnki.cczyy.2022.10.022. [19] AHRENS E, TARTLER TM, SULEIMAN A, et al. Dose-dependent relationship between intra-procedural hypoxaemia or hypocapnia and postoperative delirium in older patients[J]. Br J Anaesth, 2023, 130( 2): e298- e306. DOI: 10.1016/j.bja.2022.08.032. [20] TAYLOR J, PAYNE T, CASEY C, et al. Sevoflurane dose and postoperative delirium: A prospective cohort analysis[J]. Br J Anaesth, 2023, 130( 2): e289- e297. DOI: 10.1016/j.bja.2022.08.022. [21] SUN GQ, ZHOU SL, ZENG TL, et al. Expression of calcitonin gene-related peptide-receptor component protein in hepatocellular carcinoma and its association with prognosis[J]. J Clin Hepatol, 2022, 38( 6): 1328- 1333. DOI: 10.3969/j.issn.1001-5256.2022.06.021.孙冠群, 周思蕾, 曾榃伦, 等. 降钙素基因相关肽受体成分蛋白在肝细胞癌中的表达及其与预后的关系[J]. 临床肝胆病杂志, 2022, 38( 6): 1328- 1333. DOI: 10.3969/j.issn.1001-5256.2022.06.021. [22] HAN LY, GAO CJ. Anesthetic effect of different doses of esketamine in radical thyroidectomy and its influence on early postoperative emotional response[J]. Shandong Med J, 2023, 63( 2): 71- 75. DOI: 10.3969/j.issn.1002-266X.2023.02.018.韩礼业, 高成杰. 不同剂量艾司氯胺酮在甲状腺癌根治术中的麻醉效果及对术后早期情绪反应的影响[J]. 山东医药, 2023, 63( 2): 71- 75. DOI: 10.3969/j.issn.1002-266X.2023.02.018. -



 PDF下载 ( 799 KB)
PDF下载 ( 799 KB)

 下载:
下载: