胆道微生物群在常见胆道疾病发生发展中的作用
DOI: 10.12449/JCH240831
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:霍丽负责收集整理文献,撰写论文;畅智慧负责拟定写作思路,指导撰写文章并最后定稿。
Role of biliary microbiota in the development and progression of common biliary tract diseases
-
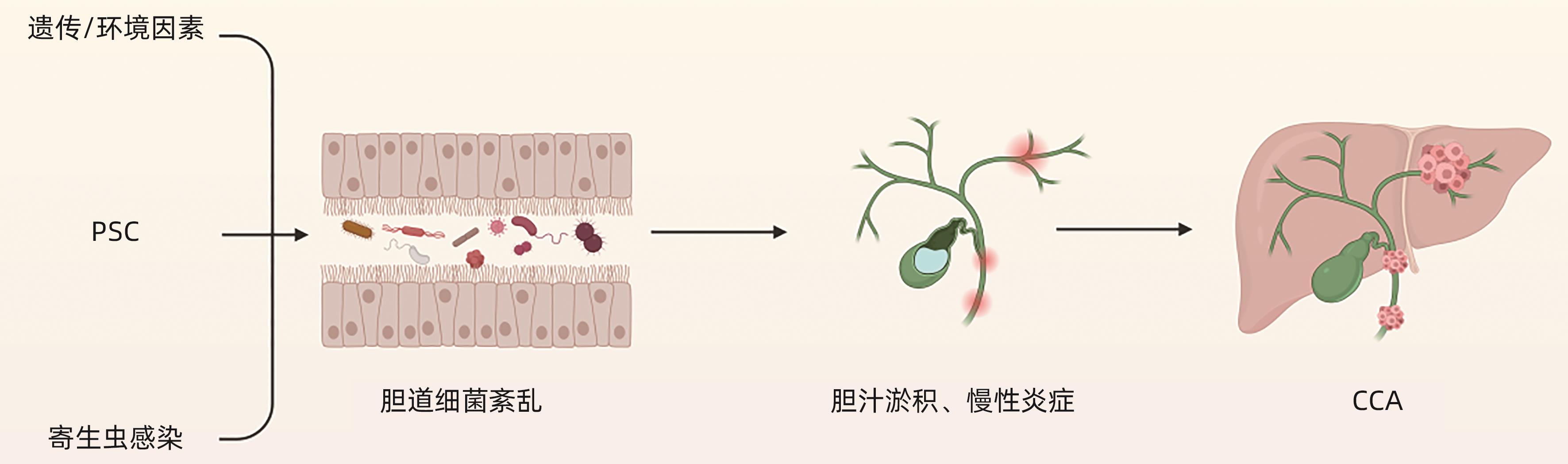
摘要: 胆道微生物群的组成与胆道疾病的发生和发展密切相关。胆道微生物群的失衡可能导致胆结石、胆道感染、自身免疫性胆管炎和胆管癌等一系列胆道疾病的发生。本文整理了胆道微生物群与胆道疾病关系的相关文献并进行综述,总结胆道微生物群对各种胆道疾病的影响,以及胆道中特定菌群在胆道疾病中发挥的作用,以期指导进一步的临床研究,为胆道疾病的预防、诊断、治疗提供新见解。Abstract: The composition of biliary microbiota is closely associated with the development and progression of biliary diseases, and imbalance of biliary microbiota may lead to a series of biliary tract diseases such as gallstones, biliary tract infections, autoimmune cholangitis, and cholangiocarcinoma. This article reviews the articles on the association between biliary microbiota and biliary tract diseases and summarizes the influence of biliary microbiota on various biliary tract diseases and the role of specific bacterial flora in biliary tract diseases, in order to guide further clinical research and provide new ideas for the prevention, diagnosis, and treatment of biliary tract diseases.
-
Key words:
- Gallstones /
- Cholangitis /
- Biliary Tract Infections /
- Cholangiocarcinoma /
- Microbiota
-
[1] SWANSON KS, de VOS WM, MARTENS EC, et al. Effect of fructans, prebiotics and fibres on the human gut microbiome assessed by 16S rRNA-based approaches: A review[J]. Benef Microbes, 2020, 11( 2): 101- 129. DOI: 10.3920/BM2019.0082. [2] LI ZQ, CHU JT, SU FX, et al. Characteristics of bile microbiota in cholelithiasis, perihilar cholangiocarcinoma, distal cholangiocarcinoma, and pancreatic cancer[J]. Am J Transl Res, 2022, 14( 5): 2962- 2971. [3] SINAGRA E, UTZERI E, MORREALE GC, et al. Microbiota-gut-brain axis and its affect inflammatory bowel disease: Pathophysiological concepts and insights for clinicians[J]. World J Clin Cases, 2020, 8( 6): 1013- 1025. DOI: 10.12998/wjcc.v8.i6.1013. [4] NASCIMENTO FSD, SUZUKI MO, TABA JV, et al. Analysis of biliary MICRObiota in hepatoBILIOpancreatic diseases compared to healthy people[MICROBILIO]: Study protocol[J]. PLoS One, 2020, 15( 11): e0242553. DOI: 10.1371/journal.pone.0242553. [5] BOYER JL. Bile formation and secretion[J]. Compr Physiol, 2013, 3( 3): 1035- 1078. DOI: 10.1002/cphy.c120027. [6] CSENDES A, BURDILES P, MALUENDA F, et al. Simultaneous bacteriologic assessment of bile from gallbladder and common bile duct in control subjects and patients with gallstones and common duct stones[J]. Arch Surg, 1996, 131( 4): 389- 394. DOI: 10.1001/archsurg.1996.01430160047008. [7] JIMÉNEZ E, SÁNCHEZ B, FARINA A, et al. Characterization of the bile and gall bladder microbiota of healthy pigs[J]. Microbiologyopen, 2014, 3( 6): 937- 949. DOI: 10.1002/mbo3.218. [8] MOLINERO N, RUIZ L, MILANI C, et al. The human gallbladder microbiome is related to the physiological state and the biliary metabolic profile[J]. Microbiome, 2019, 7( 1): 100. DOI: 10.1186/s40168-019-0712-8. [9] BERG G, RYBAKOVA D, FISCHER D, et al. Correction to: Microbiome definition re-visited: Old concepts and new challenges[J]. Microbiome, 2020, 8( 1): 119. DOI: 10.1186/s40168-020-00905-x. [10] WU T, ZHANG ZG, LIU B, et al. Gut microbiota dysbiosis and bacterial community assembly associated with cholesterol gallstones in large-scale study[J]. BMC Genomics, 2013, 14: 669. DOI: 10.1186/1471-2164-14-669. [11] YE FQ, SHEN HZ, LI Z, et al. Influence of the biliary system on biliary bacteria revealed by bacterial communities of the human biliary and upper digestive tracts[J]. PLoS One, 2016, 11( 3): e0150519. DOI: 10.1371/journal.pone.0150519. [12] SCHNEIDER J, DE WAHA P, HAPFELMEIER A, et al. Risk factors for increased antimicrobial resistance: A retrospective analysis of 309 acute cholangitis episodes[J]. J Antimicrob Chemother, 2014, 69( 2): 519- 525. DOI: 10.1093/jac/dkt373. [13] SUNG JY, COSTERTON JW, SHAFFER EA. Defense system in the biliary tract against bacterial infection[J]. Dig Dis Sci, 1992, 37( 5): 689- 696. DOI: 10.1007/BF01296423. [14] LEE J, PARK JS, BAE J, et al. Bile microbiome in patients with recurrent common bile duct stones and correlation with the duodenal microbiome[J]. Life(Basel), 2022, 12( 10): 1540. DOI: 10.3390/life12101540. [15] KIM MH, MYUNG SJ, SEO DW, et al. Association of periampullary diverticula with primary choledocholithiasis but not with secondary choledocholithiasis[J]. Endoscopy, 1998, 30( 7): 601- 604. DOI: 10.1055/s-2007-1001363. [16] LAI KH, PENG NJ, LO GH, et al. Prediction of recurrent choledocholithiasis by quantitative cholescintigraphy in patients after endoscopic sphincterotomy[J]. Gut, 1997, 41( 3): 399- 403. DOI: 10.1136/gut.41.3.399. [17] CHEN M, WANG L, WANG Y, et al. Risk factor analysis of post-ERCP cholangitis: A single-center experience[J]. Hepatobiliary Pancreat Dis Int, 2018, 17( 1): 55- 58. DOI: 10.1016/j.hbpd.2018.01.002. [18] MAKI T. Pathogenesis of calcium bilirubinate gallstone: Role of E. coli, beta-glucuronidase and coagulation by inorganic ions, polyelectrolytes and agitation[J]. Ann Surg, 1966, 164( 1): 90- 100. DOI: 10.1097/00000658-196607000-00010. [19] TAJEDDIN E, SHERAFAT SJ, MAJIDI MRS, et al. Association of diverse bacterial communities in human bile samples with biliary tract disorders: A survey using culture and polymerase chain reaction-denaturing gradient gel electrophoresis methods[J]. Eur J Clin Microbiol Infect Dis, 2016, 35( 8): 1331- 1339. DOI: 10.1007/s10096-016-2669-x. [20] HUANG D, WAN XJ. Research progress in the formation mechanism of bile duct stones[J]. Adv Clin Med, 2023, 9( 10): 16950- 16959.黄丹, 宛新建. 胆管结石形成机制的研究进展[J]. 临床医学进展, 2023, 9( 10): 16950- 16959. [21] HU FL, CHEN HT, GUO FF, et al. Biliary microbiota and mucin 4 impact the calcification of cholesterol gallstones[J]. Hepatobiliary Pancreat Dis Int, 2021, 20( 1): 61- 66. DOI: 10.1016/j.hbpd.2020.12.002. [22] NOMURA T, SHIRAI Y, HATAKEYAMA K. Enterococcal bactibilia in patients with malignant biliary obstruction[J]. Dig Dis Sci, 2000, 45( 11): 2183- 2186. DOI: 10.1023/a:1026640603312. [23] KIM B, PARK JS, BAE J, et al. Bile microbiota in patients with pigment common bile duct stones[J]. J Korean Med Sci, 2021, 36( 15): e94. DOI: 10.3346/jkms.2021.36.e94. [24] CHOE JW, LEE JM, HYUN JJ, et al. Analysis on microbial profiles& components of bile in patients with recurrent CBD stones after endoscopic CBD stone removal: A preliminary study[J]. J Clin Med, 2021, 10( 15): 3303. DOI: 10.3390/jcm10153303. [25] GUZIOR DV, QUINN RA. Review: Microbial transformations of human bile acids[J]. Microbiome, 2021, 9( 1): 140. DOI: 10.1186/s40168-021-01101-1. [26] BELZER C, KUSTERS JG, KUIPERS EJ, et al. Urease induced calcium precipitation by Helicobacter species may initiate gallstone formation[J]. Gut, 2006, 55( 11): 1678- 1679. DOI: 10.1136/gut.2006.098319. [27] SIPOS P, KRISZTINA H, BLÁZOVICS A, et al. Cholecystitis, gallstones and free radical reactions in human gallbladder[J]. Med Sci Monit, 2001, 7( 1): 84- 88. [28] GRIGOR'EVA IN, ROMANOVA TI. Gallstone disease and microbiome[J]. Microorganisms, 2020, 8( 6): 835. DOI: 10.3390/microorganisms8060835. [29] HAN JY, WU SD, FAN Y, et al. Biliary microbiota in choledocholithiasis and correlation with duodenal microbiota[J]. Front Cell Infect Microbiol, 2021, 11: 625589. DOI: 10.3389/fcimb.2021.625589. [30] LIU J, LIU B, LI HF, et al. Etiological analysis of biliary tract infection[J]. Chin J Nosocomiology, 2018, 28( 20): 3111- 3114. DOI: 10.11816/cn.ni.2018-182836.刘娟, 刘波, 李惠芬, 等. 胆道感染病原学分析[J]. 中华医院感染学杂志, 2018, 28( 20): 3111- 3114. DOI: 10.11816/cn.ni.2018-182836. [31] HU FL, SHANG D, ZHANG HX, et al. A review of Tokyo Guidelines 2018 for the management of acute biliary infections[J]. Chin J Pract Surg, 2018, 38( 7): 763- 766. DOI: 10.19538/j.cjps.issn1005-2208.2018.07.15.胡凤林, 尚东, 张浩翔, 等.《东京指南(2018)》急性胆道感染诊疗策略更新解读[J]. 中国实用外科杂志, 2018, 38( 7): 763- 766. DOI: 10.19538/j.cjps.issn1005-2208.2018.07.15. [32] XIONG GZ, ZHANG JF, DAI XP, et al. Bacterial spectrum and antimicrobial resistance of pathogens from bile culture in patients with biliary tract infection[J]. Chin J Nosocomiology, 2012, 22( 1): 198- 199.熊国祚, 张俊方, 戴先鹏, 等. 胆道感染患者胆汁培养的菌谱调查及耐药性分析[J]. 中华医院感染学杂志, 2012, 22( 1): 198- 199. [33] DALE AP, WOODFORD N. Extra-intestinal pathogenic Escherichia coli(ExPEC): Disease, carriage and clones[J]. J Infect, 2015, 71( 6): 615- 626. DOI: 10.1016/j.jinf.2015.09.009. [34] WU ZY, WU XS, YAO WY, et al. Pathogens' distribution and changes of antimicrobial resistance in the bile of acute biliary tract infection patients[J]. Chin J Surg, 2021, 59( 1): 24- 31. DOI: 10.3760/cma.j.cn112139-20200717-00559.吴自友, 吴向嵩, 姚文衍, 等. 急性胆道感染患者胆汁病原菌分布及耐药率变迁[J]. 中华外科杂志, 2021, 59( 1): 24- 31. DOI: 10.3760/cma.j.cn112139-20200717-00559. [35] China Antimicrobial Resistance Surveillance System. Antimicrobial resistance of bacteria from bile: surveillance report from China Antimicrobial Resistance Surveillance System in 2014-2019[J]. Chin J Infect Contr, 2021, 20( 1): 76- 84. DOI: 10.12138/j.issn.1671-9638.20216177.全国细菌耐药监测网. 全国细菌耐药监测网2014—2019年胆汁细菌耐药监测报告[J]. 中国感染控制杂志, 2021, 20( 1): 76- 84. DOI: 10.12138/j.issn.1671-9638.20216177. [36] MUSSA M, PÉREZ-CRESPO PMM, LOPEZ-CORTES LE, et al. Risk factors and predictive score for bacteremic biliary tract infections due to Enterococcus faecalis and Enterococcus faecium: A multicenter cohort study from the PROBAC project[J]. Microbiol Spectr, 2022, 10( 4): e0005122. DOI: 10.1128/spectrum.00051-22. [37] ZHAO CW, LIU SS, BAI X, et al. A retrospective study on bile culture and antibiotic susceptibility patterns of patients with biliary tract infections[J]. Evid Based Complement Alternat Med, 2022, 2022: 9255444. DOI: 10.1155/2022/9255444. [38] SARCOGNATO S, SACCHI D, GRILLO F, et al. Autoimmune biliary diseases: Primary biliary cholangitis and primary sclerosing cholangitis[J]. Pathologica, 2021, 113( 3): 170- 184. DOI: 10.32074/1591-951X-245. [39] KUMMEN M, THINGHOLM LB, RÜHLEMANN MC, et al. Altered gut microbial metabolism of essential nutrients in primary sclerosing cholangitis[J]. Gastroenterology, 2021, 160( 5): 1784- 1798. DOI: 10.1053/j.gastro.2020.12.058. [40] OLSSON R, BJÖRNSSON E, BÄCKMAN L, et al. Bile duct bacterial isolates in primary sclerosing cholangitis: A study of explanted livers[J]. J Hepatol, 1998, 28( 3): 426- 432. DOI: 10.1016/s0168-8278(98)80316-4. [41] LIWINSKI T, ZENOUZI R, JOHN C, et al. Alterations of the bile microbiome in primary sclerosing cholangitis[J]. Gut, 2020, 69( 4): 665- 672. DOI: 10.1136/gutjnl-2019-318416. [42] HIRAMATSU K, HARADA K, TSUNEYAMA K, et al. Amplification and sequence analysis of partial bacterial 16S ribosomal RNA gene in gallbladder bile from patients with primary biliary cirrhosis[J]. J Hepatol, 2000, 33( 1): 9- 18. DOI: 10.1016/s0168-8278(00)80153-1. [43] CARDINALE V. Classifications and misclassification in cholangiocarcinoma[J]. Liver Int, 2019, 39( 2): 260- 262. DOI: 10.1111/liv.13998. [44] KHAN SA, THOMAS HC, DAVIDSON BR, et al. Cholangiocarcinoma[J]. Lancet, 2005, 366( 9493): 1303- 1314. DOI: 10.1016/s0140-6736(05)67530-7. [45] BRINDLEY PJ, BACHINI M, ILYAS SI, et al. Cholangiocarcinoma[J]. Nat Rev Dis Primers, 2021, 7: 65. DOI: 10.1038/s41572-021-00300-2. [46] PINTO C, GIORDANO DM, MARONI L, et al. Role of inflammation and proinflammatory cytokines in cholangiocyte pathophysiology[J]. Biochim Biophys Acta Mol Basis Dis, 2018, 1864( 4 Pt B): 1270- 1278. DOI: 10.1016/j.bbadis.2017.07.024. [47] KHAN SA, TAVOLARI S, BRANDI G. Cholangiocarcinoma: Epidemiology and risk factors[J]. Liver Int, 2019, 39( Suppl 1): 19- 31. DOI: 10.1111/liv.14095. [48] BARNER-RASMUSSEN N, PUKKALA E, JUSSILA A, et al. Epidemiology, risk of malignancy and patient survival in primary sclerosing cholangitis: A population-based study in Finland[J]. Scand J Gastroenterol, 2020, 55( 1): 74- 81. DOI: 10.1080/00365521.2019.1707277. [49] PEREIRA P, AHO V, AROLA J, et al. Bile microbiota in primary sclerosing cholangitis: Impact on disease progression and development of biliary dysplasia[J]. PLoS One, 2017, 12( 8): e0182924. DOI: 10.1371/journal.pone.0182924. [50] DYSON JK, BEUERS U, JONES DEJ, et al. Primary sclerosing cholangitis[J]. Lancet, 2018, 391( 10139): 2547- 2559. DOI: 10.1016/s0140-6736(18)30300-3. [51] SUTTIPRAPA S, SOTILLO J, SMOUT M, et al. Opisthorchis viverrini proteome and host-parasite interactions[J]. Adv Parasitol, 2018, 102: 45- 72. DOI: 10.1016/bs.apar.2018.06.002. [52] XU T, ZHANG B, ZHOU WC. Research progress on the relationship between biliary flora and cholangiocarcinoma[J]. Chin J Bases Clin Gen Surg, 2021, 28( 3): 404- 408. DOI: 10.7507/1007-9424.202006047.徐涛, 张波, 周文策. 胆道菌群与胆管癌关系的研究进展[J]. 中国普外基础与临床杂志, 2021, 28( 3): 404- 408. DOI: 10.7507/1007-9424.202006047. [53] CHNG KR, CHAN SH, NG AHQ, et al. Tissue microbiome profiling identifies an enrichment of specific enteric bacteria in Opisthorchis viverrini associated cholangiocarcinoma[J]. EBioMedicine, 2016, 8: 195- 202. DOI: 10.1016/j.ebiom.2016.04.034. [54] CHEN BR, FU SW, LU LG, et al. A preliminary study of biliary microbiota in patients with bile duct stones or distal cholangiocarcinoma[J]. Biomed Res Int, 2019, 2019: 1092563. DOI: 10.1155/2019/1092563. -



 PDF下载 ( 1104 KB)
PDF下载 ( 1104 KB)

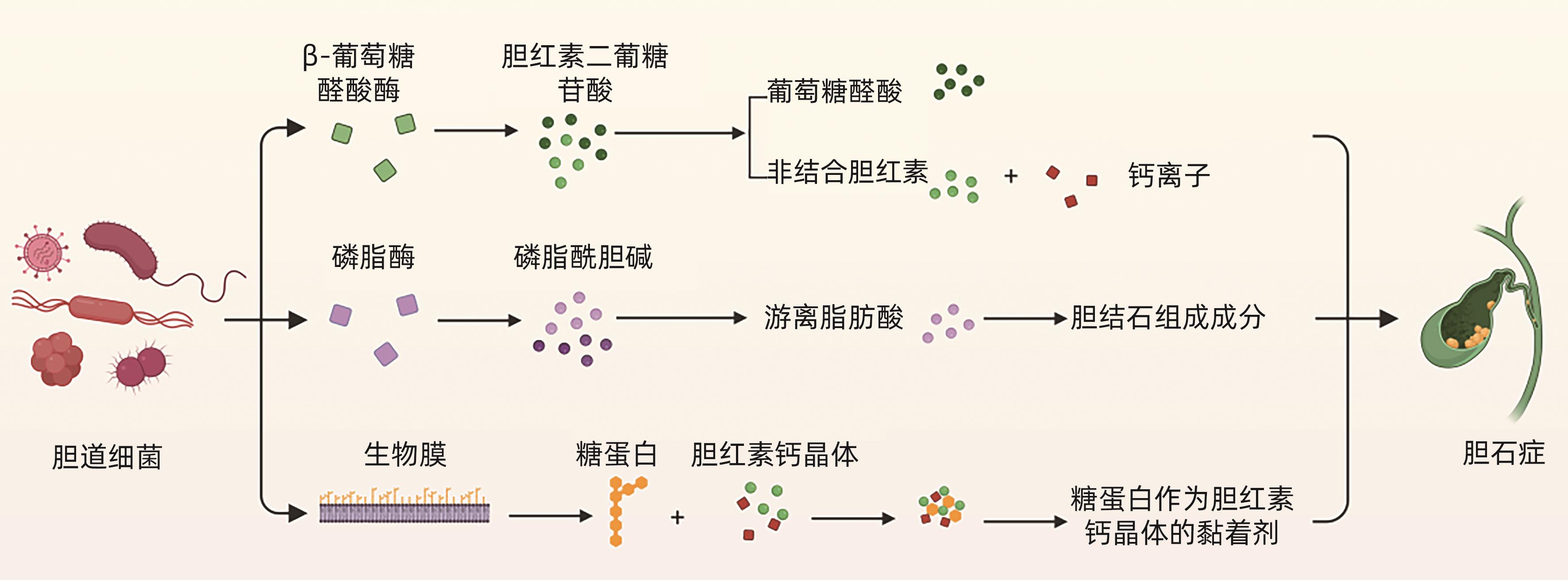
 下载:
下载: