慢性乙型肝炎及肝硬化患者血清血管生成素1、2及其比值变化与HBV DNA和ALT的相关性分析
DOI: 10.12449/JCH240609
Correlation of serum angiopoietin-1, angiopoietin-2, and angiopoietin-1/angiopoietin-2 ratio with HBV DNA and alanine aminotransferase in patients with chronic hepatitis B or liver cirrhosis
-
摘要:
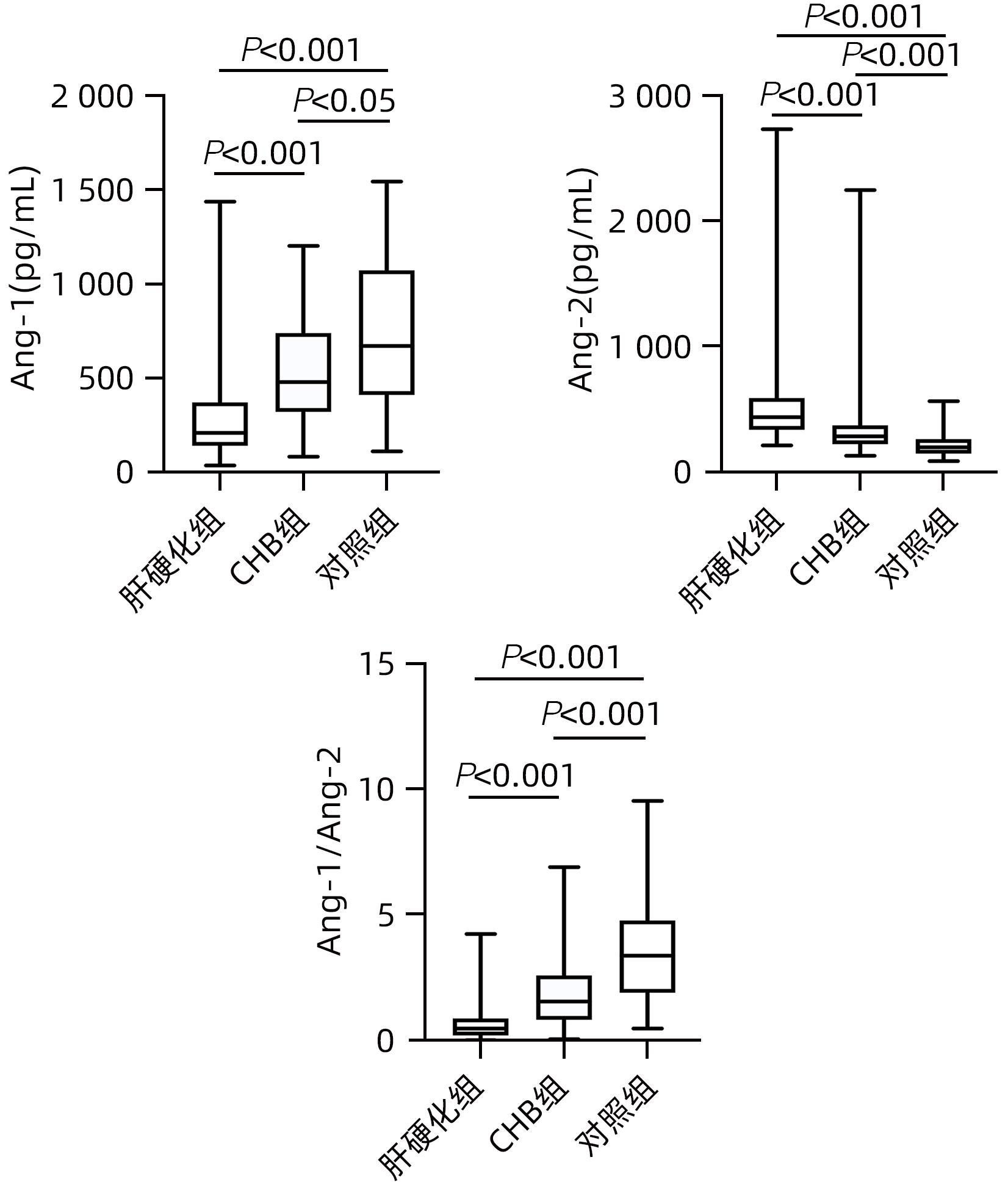
目的 分析血清血管生成素(Ang)1、2及其比值变化与慢性乙型肝炎(CHB)、肝硬化患者HBV DNA和ALT的相关性。 方法 选取2018年3月—2019年10月首都医科大学附属北京佑安医院收治的CHB患者99例,肝硬化患者59例,收集临床资料和血清标本;另选同期46例健康体检者作为对照组。所有患者均采用PCR法检测血清HBV DNA;采用酶联免疫吸附法检测血清Ang-1和Ang-2水平,比较各组血清Ang-1和Ang-2及Ang-1/Ang-2的差异。非正态分布的计量资料多组间比较采用Kruskal-Wallis H检验,进一步两两比较采用Bonferroni法;采用Spearman方法分析Ang-1、Ang-2、Ang-1/Ang-2与HBV DNA、ALT的相关性。 结果 与对照组(671.0 pg/mL)相比,CHB组(479.0 pg/mL)和肝硬化组(208.4 pg/mL)Ang-1水平显著降低(P值均<0.05);与CHB组相比,肝硬化组Ang-1水平显著降低(P<0.001)。与对照组(198.0 pg/mL)相比,CHB组(286.1 pg/mL)和肝硬化组(438.4 pg/mL)Ang-2水平显著升高(P值均<0.001);与CHB组相比,肝硬化组Ang-2水平显著升高(P<0.001)。与对照组(3.4)相比,CHB组(1.6)和肝硬化组(0.5)Ang-1/Ang-2比值显著降低(P值均<0.001);与CHB组相比,肝硬化组Ang-1/Ang-2比值显著降低(P<0.001)。Spearman分析显示,CHB组Ang-1与HBV DNA及ALT均呈负相关(r值分别为-0.400、-0.394,P值均˂0.001);Ang-2与HBV DNA及ALT均呈正相关(r值分别为0.365、0.351,P值均˂0.001);Ang-1/Ang-2与HBV DNA及ALT均呈负相关(r值分别为-0.463、-0.473,P值均˂0.001);而肝硬化组Ang-1、Ang-2及Ang-1/Ang-2均与HBV DNA和ALT无相关性(P值均˃0.05)。 结论 CHB、肝硬化患者血清Ang-1、Ang-2及Ang-1/Ang-2有显著改变,其中肝炎组Ang-1、Ang-2及Ang-1/Ang-2在一定程度上反映CHB患者肝损伤的程度。 Abstract:Objective To investigate the correlation of serum angiopoietin-1 (Ang-1), angiopoietin-2 (Ang-2), and Ang-1/Ang-2 ratio with HBA DNA and alanine aminotransferase (ALT) in patients with chronic hepatitis B (CHB) or liver cirrhosis. Methods Clinical data and serum specimens were collected from 99 patients with CHB and 59 patients with liver cirrhosis who were admitted to Beijing YouAn Hospital, Capital Medical University, from March 2018 to October 2019, and 46 individuals who underwent physical examination were enrolled as control group. PCR was used to measure serum HBV DNA level, and ELISA was used to measure the serum levels of Ang-1 and Ang-2. The serum levels of Ang-1 and Ang-2 and Ang-1/Ang-2 ratio were compared between groups. The Kruskal-Wallis H test was used for comparison of non-normally distributed continuous data between multiple groups, and the Bonferroni method was used for further comparison between two groups; the Spearman correlation analysis was used to investigate the correlation of Ang-1, Ang-2, and Ang-1/Ang-2 ratio with HBV DNA and ALT. Results Compared with the control group, the CHB group and the liver cirrhosis group had a significant reduction in the level of Ang-1 (479.0 pg/mL and 208.4 pg/mL vs 671.0 pg/mL, both P<0.05), and compared with the CHB group, the liver cirrhosis group had a significant reduction in the level of Ang-1 (P<0.001). Compared with the control group, the CHB group and the liver cirrhosis group had a significant increase in the level of Ang-2 (286.1 pg/mL and 438.4 pg/mL vs 198.0 pg/mL, both P<0.001), and compared with the CHB group, the liver cirrhosis group had a significant increase in the level of Ang-2 (P<0.001). Compared with the control group, the CHB group and the liver cirrhosis group had a significant reduction in Ang-1/Ang-2 ratio (1.6 and 0.5 vs 3.4, both P<0.001), and compared with the CHB group, the liver cirrhosis group had a significant reduction in Ang-1/Ang-2 ratio (P<0.001). The Spearman correlation analysis showed that in the CHB group, Ang-1 was negatively correlated with HBV DNA and ALT (r=-0.400 and -0.394, both P˂0.001), Ang-2 was positively correlated with HBV DNA and ALT (r=0.365 and 0.351, both P<0.001), and Ang-1/Ang-2 ratio was negatively correlated with HBV DNA and ALT (r=-0.463 and -0.473, both P<0.001); in the liver cirrhosis group, Ang-1, Ang-2, and Ang-1/Ang-2 ratio had no correlation with HBV DNA or ALT (all P>0.05). Conclusion There are significant changes in the serum levels of Ang-1 and Ang-2 and Ang-1/Ang-2 ratio in patients with CHB or liver cirrhosis, and Ang-1, Ang-2, and Ang-1/Ang-2 ratio reflects the degree of liver injury in patients with CHB to a certain extent. -
Key words:
- Angiopoietin-1 /
- Angiopoietin-2 /
- Hepatitis B, Chronic /
- Liver Cirrhosis /
- Hepatitis B virus /
- Alanine Transaminase
-
表 1 各组血清Ang-1、Ang-2表达水平及Ang-1/Ang-2比值
Table 1. The levels of Ang-1、Ang-2 and radio of Ang-1/Ang-2 in groups
组别 例数 Ang-1(pg/mL) Ang-2(pg/mL) Ang-1/Ang-2 对照组 46 671.0(410.8~1 072.5) 198.0(149.3~263.1) 3.4(1.9~4.8) CHB组 99 479.0(320.9~740.0)1) 286.1(224.3~373.2)2) 1.6(0.8~2.6)2) 肝硬化组 59 208.4(140.1~370.0)1)3) 438.4(338.0~590.5)2)3) 0.5(0.2~0.9)2)3) χ2值 56.66 70.20 86.33 P值 <0.001 <0.001 <0.001 注:与对照组比较,1)P<0.05,2)P<0.001;与CHB组比较,3)P<0.001。 表 2 CHB组Ang-1、Ang-2及Ang-1/Ang-2比值与HBV DNA、ALT的相关性分析
Table 2. Correlation analysis of Ang-1, Ang-2, and Ang-1/Ang-2 ratios with HBV DNA and ALT in hepatitis group
指标 HBV DNA(IU/mL) ALT(U/L) r值 P值 r值 P值 Ang-1 -0.400 <0.001 -0.394 <0.001 Ang-2 0.365 <0.001 0.351 <0.001 Ang-1/Ang-2 -0.463 <0.001 -0.473 <0.001 表 3 肝硬化组Ang-1、Ang-2及Ang-1/Ang-2比值与HBV DNA、ALT的相关性分析
Table 3. Correlation analysis of Ang-1, Ang-2, and Ang-1/Ang-2 ratios with HBV DNA and ALT in cirrhosis group
指标 HBV DNA(IU/mL) ALT(U/L) r值 P值 r值 P值 Ang-1 0.204 0.121 -0.001 0.992 Ang-2 0.032 0.812 -0.089 0.501 Ang-1/Ang-2 0.141 0.287 0.007 0.960 -
[1] SAHARINEN P, LEPPÄNEN VM, ALITALO K. SnapShot: Angiopoietins and their functions[J]. Cell, 2017, 171( 3): 724- 724. DOI: 10.1016/j.cell.2017.10.009. [2] JEANSSON M, GAWLIK A, ANDERSON G, et al. Angiopoietin-1 is essential in mouse vasculature during development and in response to injury[J]. J Clin Invest, 2011, 121( 6): 2278- 2289. DOI: 10.1172/JCI46322. [3] LEE SJ, LEE CK, KANG S, et al. Angiopoietin-2 exacerbates cardiac hypoxia and inflammation after myocardial infarction[J]. J Clin Invest, 2018, 128( 11): 5018- 5033. DOI: 10.1172/JCI99659. [4] MELENDEZ E, WHITNEY JE, NORTON JS, et al. Systemic angiopoietin-1/2 dysregulation in pediatric sepsis and septic shock[J]. Int J Med Sci, 2019, 16( 2): 318- 323. DOI: 10.7150/ijms.27731. [5] KUMAR NP, VELAYUTHAM B, NAIR D, et al. Angiopoietins as biomarkers of disease severity and bacterial burden in pulmonary tuberculosis[J]. Int J Tuberc Lung Dis, 2017, 21( 1): 93- 99. DOI: 10.5588/ijtld.16.0565. [6] van MEURS M, KÜMPERS P, LIGTENBERG JJ, et al. Bench-to-bedside review: Angiopoietin signalling in critical illness-a future target?[J]. Crit Care, 2009, 13( 2): 207. DOI: 10.1186/cc7153. [7] Chinese Society of Infectious Diseases, Chinese Medical Association; Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B(version 2019)[J]. J Clin Hepatol, 2019, 35( 12): 2648- 2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007.中华医学会感染病学分会, 中华医学会肝病学分会. 慢性乙型肝炎防治指南(2019年版)[J]. 临床肝胆病杂志, 2019, 35( 12): 2648- 2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007. [8] PARIKH SM. Dysregulation of the angiopoietin-Tie-2 axis in sepsis and ARDS[J]. Virulence, 2013, 4( 6): 517- 524. DOI: 10.4161/viru.24906. [9] FAILLACI F, MARZI L, CRITELLI R, et al. Liver angiopoietin-2 is a key predictor of de novo or recurrent hepatocellular cancer after hepatitis C virus direct-acting antivirals[J]. Hepatology, 2018, 68( 3): 1010- 1024. DOI: 10.1002/hep.29911. [10] UEHARA M, ENOMOTO N, MIKAMO M, et al. Impact of angiopoietin-1 and-2 on clinical course of idiopathic pulmonary fibrosis[J]. Respir Med, 2016, 114: 18- 26. DOI: 10.1016/j.rmed.2016.03.001. [11] LIN MH, SHI Y, XIE F, et al. Research progress of angiogenesis in liver fibrosis[J]. Beijing Med J, 2014, 36( 6): 468- 470. DOI: 10.15932/j.0253-9713.2014.06.031.林明华, 石英, 谢放, 等. 血管生成在肝纤维化中的研究进展[J]. 北京医学, 2014, 36( 6): 468- 470. DOI: 10.15932/j.0253-9713.2014.06.031. [12] SAHARINEN P, EKLUND L, ALITALO K. Therapeutic targeting of the angiopoietin-TIE pathway[J]. Nat Rev Drug Discov, 2017, 16( 9): 635- 661. DOI: 10.1038/nrd.2016.278. [13] PAUTA M, RIBERA J, MELGAR-LESMES P, et al. Overexpression of angiopoietin-2 in rats and patients with liver fibrosis. Therapeutic consequences of its inhibition[J]. Liver Int, 2015, 35( 4): 1383- 1392. DOI: 10.1111/liv.12505. [14] LEFERE S, van de VELDE F, HOORENS A, et al. Angiopoietin-2 promotes pathological angiogenesis and is a therapeutic target in murine nonalcoholic fatty liver disease[J]. Hepatology, 2019, 69( 3): 1087- 1104. DOI: 10.1002/hep.30294. [15] WHITEHEAD M, OSBORNE A, WIDDOWSON PS, et al. Angiopoietins in diabetic retinopathy: Current understanding and therapeutic potential[J]. J Diabetes Res, 2019, 2019: 5140521. DOI: 10.1155/2019/5140521. [16] YU XL, YE FC. Role of angiopoietins in development of cancer and neoplasia associated with viral infection[J]. Cells, 2020, 9( 2): 457. DOI: 10.3390/cells9020457. [17] KHANANI AM, RUSSELL MW, AZIZ AA, et al. Angiopoietins as potential targets in management of retinal disease[J]. Clin Ophthalmol, 2021, 15: 3747- 3755. DOI: 10.2147/OPTH.S231801. [18] COLLAZOS-ALEMÁN JD, GNECCO-GONZÁLEZ S, JARAMILLO-ZARAMA B, et al. The role of angiopoietins in neovascular diabetes-related retinal diseases[J]. Diabetes Ther, 2022, 13( 11-12): 1811- 1821. DOI: 10.1007/s13300-022-01326-9. [19] ZHANG HM, ZHAO ZB, XIONG YX, et al. Research progress of angiopoietins in hepatocellular carcinoma[J]. J Clin Hepatol, 2011, 27( 4): 433- 436. DOI: 10.3969/j.issn.1001-5256.2011.04.030.张华敏, 赵正斌, 熊亚星, 等. 血管生成素在肝细胞癌中的研究进展[J]. 临床肝胆病杂志, 2011, 27( 4): 433- 436. DOI: 10.3969/j.issn.1001-5256.2011.04.030. [20] FIEDLER U, REISS Y, SCHARPFENECKER M, et al. Angiopoietin-2 sensitizes endothelial cells to TNF-alpha and has a crucial role in the induction of inflammation[J]. Nat Med, 2006, 12( 2): 235- 239. DOI: 10.1038/nm1351. [21] LE CRAS TD, MOBBERLEY-SCHUMAN PS, BROERING M, et al. Angiopoietins as serum biomarkers for lymphatic anomalies[J]. Angiogenesis, 2017, 20( 1): 163- 173. DOI: 10.1007/s10456-016-9537-2. [22] HERNÁNDEZ-BARTOLOMÉ Á, LÓPEZ-RODRÍGUEZ R, BORQUE MJ, et al. Angiopoietin-2/angiopoietin-1 as non-invasive biomarker of cirrhosis in chronic hepatitis C[J]. World J Gastroenterol, 2016, 22( 44): 9744- 9751. DOI: 10.3748/wjg.v22.i44.9744. -



 PDF下载 ( 661 KB)
PDF下载 ( 661 KB)

 下载:
下载:


