肝衰竭并发急性胰腺炎的机制及预防
DOI: 10.12449/JCH240434
-
摘要: 肝衰竭病情进展快,并发症多,病情十分凶险。在肝衰竭发展过程中,并发急性胰腺炎十分常见;而急性胰腺炎的临床症状及体征与肝衰竭并发自发性腹膜炎极其相似,易被忽略。本文通过炎症反应、十二指肠乳头功能障碍、肠道菌群失调、氧化应激、微循环障碍等5个方面对肝衰竭并发急性胰腺炎的机制进行阐述,并根据其作用机制提出相应预防手段。
-
关键词:
- 肝功能衰竭 /
- 胰腺炎, 急性坏死性 /
- 病理过程 /
- 早期医疗干预
Abstract: Liver failure often has rapid progression, multiple complications, and dangerous conditions. Acute pancreatitis is a common comorbidity during the progression of liver failure, and since acute pancreatitis has extremely similar clinical symptoms and signs to liver failure complicated by spontaneous peritonitis, it is often neglected in clinical practice. This article elaborates on the mechanisms of liver failure complicated by acute pancreatitis from the five aspects of inflammatory response, duodenal papillary dysfunction, gut microbiota dysbiosis, oxidative stress, and microcirculatory disturbance and proposes corresponding preventive measures based on these mechanisms. -
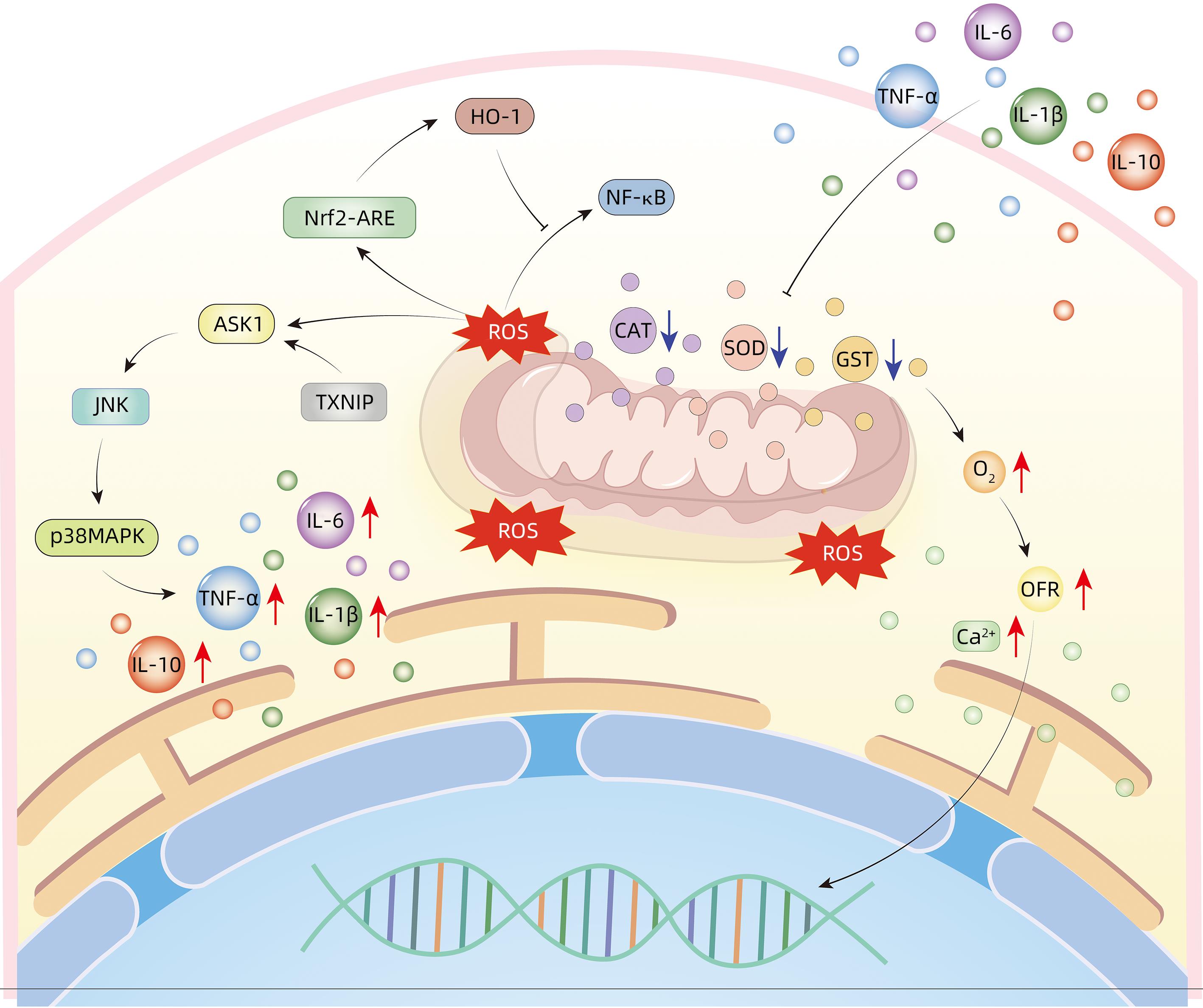
表 1 肝衰竭过程中细胞因子对胰腺的作用
Table 1. Effect of cytokines on pancreas during liver failure
细胞因子 作用机制 IL-1β 通过改变Ca2+稳态失衡诱导胰蛋白酶活化并降低胰腺腺泡细胞的细胞活力[6];诱导炎性细胞产生IL-6、IL-18、TNF-α等,介导炎症反应等过程[7] IL-6 通过gp130蛋白激活JAK-STAT信号通路诱导胰腺炎的发生[8];IL-6激活胰腺腺泡细胞中STAT-3磷酸化,增加急性胰腺炎的严重程度 IL-18 协同IL-12诱导IFN-γ的生成,从而提升T淋巴细胞以及NK细胞的功能; 激活MAPK和PI3K/AKT信号通路,导致大量细胞因子的产生,进一步加剧了炎症损害[9] IL-33 触发腺泡释放炎症因子,使得急性胰腺炎病情加重;诱导IL-6及IL-8等炎症因子的产生,介入炎症反应[10] TNF-α 刺激NF-κB信号通路的激活,有助于炎症反应的全身性进展[11]。激活T淋巴细胞,促进炎症因子释放,诱发炎症反应[12] MCP-1 诱导单核细胞的趋化与激活,使其积极参与免疫应答[13] MIF 激活MAPK、NF-κB信号通路,刺激巨噬细胞产生IL-1、IL-6、IL-12、TNF等炎症因子[14] ICAM-1 其通过激活白细胞和血管内皮细胞的黏连与聚集过程,从而增加微血管的通透性,引致血管内皮的损害,形成微循环障碍[15] ROS 激活JNK、NF-κB、MAPK、AP-1信号通路,诱导IL-1、IL-6、TNF-α、iNOS等炎症因子产生[16] 注:MCP-1,单核细胞趋化蛋白-1;ROS,活性氧;ICAM-1,细胞间黏附分子-1。 -
[1] Liver Failure and Artificial Hepatology Group, Infectious Diseases Branch of Chinese Medical Association, Severe Liver Disease and Artificial Hepatology Group, Hepatology Branch of Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [2] Pancreatic Surgery Group, Surgery Branch of Chinese Medical Association. Guidelines for the diagnosis and treatment of acute pancreatitis in China(2021)[J]. Chin J Dig Surg, 2021, 20( 7): 730- 739. DOI: 10.3760/cma.j.cn115610-20210622-00297.中华医学会外科学分会胰腺外科学组. 中国急性胰腺炎诊治指南(2021)[J]. 中华消化外科杂志, 2021, 20( 7): 730- 739. DOI: 10.3760/cma.j.cn115610-20210622-00297. [3] PANIC N, MIHAJLOVIC S, VUJASINOVIC M, et al. Pancreatitis associated with viral hepatitis: Systematic review[J]. J Clin Med, 2020, 9( 10): 3309. DOI: 10.3390/jcm9103309. [4] XU WQ, GUO M, WANG X, et al. Molecular mechanism of liver injury in acute pancreatitis[J]. J Clin Hepatol, 2022, 38( 11): 2663- 2668. DOI: 10.3969/j.issn.1001-5256.2022.11.045.徐文倩, 郭敏, 王晓, 等. 急性胰腺炎肝损伤的分子机制[J]. 临床肝胆病杂志, 2022, 38( 11): 2663- 2668. DOI: 10.3969/j.issn.1001-5256.2022.11.045. [5] ALANAZI A, NAGI MN, ALHARETH DY, et al. Crosstalk of TNF-α, IFN-γ, NF-κB, STAT1 and redox signaling in lipopolysaccharide/d-galactosamine/dimethylsulfoxide-induced fulminant hepatic failure in mice[J]. Saudi Pharm J, 2023, 31( 3): 370- 381. DOI: 10.1016/j.jsps.2023.01.005. [6] XU B, BAI B, SHA SM, et al. Interleukin-1β induces autophagy by affecting calcium homeostasis and trypsinogen activation in pancreatic acinar cells[J]. Int J Clin Exp Pathol, 2014, 7( 7): 3620- 3631. [7] KANY S, VOLLRATH JT, RELJA B. Cytokines in inflammatory disease[J]. Int J Mol Sci, 2019, 20( 23): 6008. DOI: 10.3390/ijms20236008. [8] LESINA M, WÖRMANN SM, NEUHÖFER P, et al. Interleukin-6 in inflammatory and malignant diseases of the pancreas[J]. Semin Immunol, 2014, 26( 1): 80- 87. DOI: 10.1016/j.smim.2014.01.002. [9] REX DAB, AGARWAL N, PRASAD TSK, et al. A comprehensive pathway map of IL-18-mediated signalling[J]. J Cell Commun Signal, 2020, 14( 2): 257- 266. DOI: 10.1007/s12079-019-00544-4. [10] KURIMOTO M, WATANABE T, KAMATA K, et al. IL-33 as a critical cytokine for inflammation and fibrosis in inflammatory bowel diseases and pancreatitis[J]. Front Physiol, 2021, 12: 781012. DOI: 10.3389/fphys.2021.781012. [11] MALLEO G, MAZZON E, SIRIWARDENA AK, et al. Role of tumor necrosis factor-alpha in acute pancreatitis: From biological basis to clinical evidence[J]. Shock Augusta Ga, 2007, 28( 2): 130- 140. DOI: 10.1097/shk.0b013e3180487ba1. [12] TIEGS G, HORST AK. TNF in the liver: Targeting a central player in inflammation[J]. Semin Immunopathol, 2022, 44( 4): 445- 459. DOI: 10.1007/s00281-022-00910-2. [13] ISHIBASHI T, ZHAO HF, KAWABE K, et al. Blocking of monocyte chemoattractant protein-1(MCP-1) activity attenuates the severity of acute pancreatitis in rats[J]. J Gastroenterol, 2008, 43( 1): 79- 85. DOI: 10.1007/s00535-007-2126-9. [14] ZHU CJ, LIU YN, SONG YD, et al. Deletion of macrophage migration inhibitory factor ameliorates inflammation in mice model severe acute pancreatitis[J]. Biomed Pharmacother, 2020, 125: 109919. DOI: 10.1016/j.biopha.2020.109919. [15] AMPOFO E, BERG JJ, MENGER MD, et al. Maslinic acid alleviates ischemia/reperfusion-induced inflammation by downregulation of NFκB-mediated adhesion molecule expression[J]. Sci Rep, 2019, 9( 1): 6119. DOI: 10.1038/s41598-019-42465-7. [16] LI Z, LIU T, FENG Y, et al. PPARγ alleviates sepsis-induced liver injury by inhibiting hepatocyte pyroptosis via inhibition of the ROS/TXNIP/NLRP3 signaling pathway[J]. Oxid Med Cell Longev, 2022, 2022: 1269747. DOI: 10.1155/2022/1269747. [17] SATOH A, GUKOVSKAYA AS, NIETO JM, et al. PKC-δ and-ε regulate NF-κB activation induced by cholecystokinin and TNF-α in pancreatic acinar cells[J]. Am J Physiol Gastrointest Liver Physiol, 2004, 287( 3): G582- G591. DOI: 10.1152/ajpgi.00087.2004. [18] ZHANG XP, ZHANG J, MA ML, et al. Pathological changes at early stage of multiple organ injury in a rat model of severe acute pancreatitis[J]. Hepatobiliary Pancreat Dis Int, 2010, 9( 1): 83- 87. [19] ZHU MH, XU Y, ZHANG WB, et al. Inhibition of PAK1 alleviates cerulein-induced acute pancreatitis via p38 and NF-κB pathways[J]. Biosci Rep, 2019, 39( 3): BSR20182221. DOI: 10.1042/bsr20182221. [20] CHEN Z, DONG WH, WU Q, et al. Two-layer regulation of TRAF6 mediated by both TLR4/NF-kB signaling and miR-589-5p increases proinflammatory cytokines in the pathology of severe acute pancreatitis[J]. Am J Transl Res, 2020, 12( 6): 2379- 2395. [21] LI G, WU XJ, YANG L, et al. TLR4-mediated NF-κB signaling pathway mediates HMGB1-induced pancreatic injury in mice with severe acute pancreatitis[J]. Int J Mol Med, 2016, 37( 1): 99- 107. DOI: 10.3892/ijmm.2015.2410. [22] SENDLER M, VAN DEN BRANDT C, GLAUBITZ J, et al. NLRP3 inflammasome regulates development of systemic inflammatory response and compensatory anti-inflammatory response syndromes in mice with acute pancreatitis[J]. Gastroenterology, 2020, 158( 1): 253- 269. e 14. DOI: 10.1053/j.gastro.2019.09.040. [23] MAO Q. Pathogenesis and management strategies of liver failure-associated cholestasis[J]. J Clin Hepatol, 2019, 35( 2): 258- 261. DOI: 10.3969/j.issn.1001-5256.2019.02.004.毛青. 肝衰竭时胆汁淤积的发生机制及处置对策[J]. 临床肝胆病杂志, 2019, 35( 2): 258- 261. DOI: 10.3969/j.issn.1001-5256.2019.02.004. [24] COUCKE EM, AKBAR H, KAHLOON A, et al. Biliary obstruction[M]. Treasure Island(FL): StatPearls Publishing, 2023. [25] WANG GJ, GAO CF, WEI D, et al. Acute pancreatitis: Etiology and common pathogenesis[J]. World J Gastroenterol, 2009, 15( 12): 1427- 1430. DOI: 10.3748/wjg.15.1427. [26] ZHAN XB, WAN JH, ZHANG GW, et al. Elevated intracellular trypsin exacerbates acute pancreatitis and chronic pancreatitis in mice[J]. Am J Physiol Gastrointest Liver Physiol, 2019, 316( 6): G816- G825. DOI: 10.1152/ajpgi.00004.2019. [27] ZHENG Q, LIU JS, ZHENG BF, et al. The role of pancreatic duct in the pathogenesis of acute pancreatitis[J]. Chin J Clin Res, 2020, 33( 11): 1598- 1600. DOI: 10.13429/j.cnki.cjcr.2020.11.038. [28] MEI QX, FU Y, HUANG ZH, et al. Intestinal TLR4 deletion exacerbates acute pancreatitis through gut microbiota dysbiosis and Paneth cells deficiency[J]. Gut Microbes, 2022, 14( 1): 2112882. DOI: 10.1080/19490976.2022.2112882. [29] ZHANG ZW, TANAKA I, PAN Z, et al. Intestinal homeostasis and inflammation: Gut microbiota at the crossroads of pancreas-intestinal barrier axis[J]. Eur J Immunol, 2022, 52( 7): 1035- 1046. DOI: 10.1002/eji.202149532. [30] PATEL BK, PATEL KH, BHATIA M, et al. Gut microbiome in acute pancreatitis: A review based on current literature[J]. World J Gastroenterol, 2021, 27( 30): 5019- 5036. DOI: 10.3748/wjg.v27.i30.5019. [31] LIU XQ, HUSSAIN R, MEHMOOD K, et al. Mitochondrial-endoplasmic reticulum communication-mediated oxidative stress and autophagy[J]. Biomed Res Int, 2022, 2022: 6459585. DOI: 10.1155/2022/6459585. [32] RAMUDO L, MANSO MA. N-acetylcysteine in acute pancreatitis[J]. World J Gastrointest Pharmacol Ther, 2010, 1( 1): 21- 26. DOI: 10.4292/wjgpt.v1.i1.21. [33] BICZO G, VEGH ET, SHALBUEVA N, et al. Mitochondrial dysfunction, through impaired autophagy, leads to endoplasmic reticulum stress, deregulated lipid metabolism, and pancreatitis in animal models[J]. Gastroenterology, 2018, 154( 3): 689- 703. DOI: 10.1053/j.gastro.2017.10.012. [34] LIU YN, LI MK, MEI CP, et al. Thioredoxin-interacting protein deficiency protects against severe acute pancreatitis by suppressing apoptosis signal-regulating kinase 1[J]. Cell Death Dis, 2022, 13( 10): 914. DOI: 10.1038/s41419-022-05355-x. [35] XIONG J, WANG KZ, YUAN CX, et al. Luteolin protects mice from severe acute pancreatitis by exerting HO-1-mediated anti-inflammatory and antioxidant effects[J]. Int J Mol Med, 2017, 39( 1): 113- 125. DOI: 10.3892/ijmm.2016.2809. [36] LIU XN, ZHU QT, ZHANG M, et al. Isoliquiritigenin ameliorates acute pancreatitis in mice via inhibition of oxidative stress and modulation of the Nrf2/HO-1 pathway[J]. Oxid Med Cell Longev, 2018, 2018: 7161592. DOI: 10.1155/2018/7161592. [37] PLUSCZYK T, BERSAL B, WESTERMANN S, et al. ET-1 induces pancreatitis-like microvascular deterioration and acinar cell injury[J]. J Surg Res, 1999, 85( 2): 301- 310. DOI: 10.1006/jsre.1999.5610. [38] AMBUDKAR IS. Polarization of calcium signaling and fluid secretion in salivary gland cells[J]. Curr Med Chem, 2012, 19( 34): 5774- 5781. DOI: 10.2174/092986712804143321. [39] KABBANI AR, TERGAST TL, MANNS MP, et al. Behandlungsstrategien des akut-auf-chronischen leberversagens[J]. Med Klin Intensivmedizin Und Notfallmedizin, 2021, 116( 1): 3- 16. DOI: 10.1007/s00063-019-00613-x. [40] KHANAM A, KOTTILIL S. Acute-on-chronic liver failure: Pathophysiological mechanisms and management[J]. Front Med(Lausanne), 2021, 8: 752875. DOI: 10.3389/fmed.2021.752875. [41] YE C, LI WY, LI L, et al. Glucocorticoid treatment strategies in liver failure[J]. Front Immunol, 2022, 13: 846091. DOI: 10.3389/fimmu.2022.846091. [42] ZHANG XF, WANG LY, ZHANG Y, et al. Etiological characteristics, laboratory test indexes and prognosis of hepatic failure patients with secondary infection[J]. Chin J Nosocomiology, 2023, 9( 17): 2590- 2594.张晓芳, 汪陆叶, 章颖, 等. 肝衰竭继发感染病原学和实验室指标水平变化及预后[J]. 中华医院感染学杂志, 2023, 9( 17): 2590- 2594. [43] WANG XM. Diagnostic value of inflammation index in hepatitis B virus-associated chronic and acute liver failure complicated with infection[J]. China Mod Med, 2020, 27( 32): 86- 89. DOI: 10.3969/j.issn.1674-4721.2020.32.026.王香梅. 炎症指标在乙肝病毒相关慢加急性肝衰竭并发感染中的诊断价值[J]. 中国当代医药, 2020, 27( 32): 86- 89. DOI: 10.3969/j.issn.1674-4721.2020.32.026. [44] XIE SA. Clinical study of ERCP in the treatment of acute biliary pancreatitis[D]. Guangzhou: Guangzhou Medical University, 2022.谢水安. ERCP治疗急性胆源性胰腺炎的临床研究[D]. 广州: 广州医科大学, 2022. [45] Expert Committee on Diagnosis and Treatment of Intrahepatic Cholestasis. Expert consensus for diagnosis and treatment of intrahepatic cholestasis[J]. Chin J Clin Infect Dis, 2015, 8( 5): 402- 406. DOI: 10.3760/cma.j.issn.1674-2397.2015.05.002.肝内胆汁积症诊治专家委员会. 肝内胆汁淤积症诊治专家共识[J]. 中华临床感染病杂志, 2015, 8( 5): 402- 406. DOI: 10.3760/cma.j.issn.1674-2397.2015.05.002. [46] YU BJ. Protective effect of rifaximin on severe acute pancreatitis and its mechanism[D]. Nanchang: Nanchang University, 2021.喻冰君. 利福昔明对重症急性胰腺炎的保护作用及机制初探[D]. 南昌: 南昌大学, 2021. [47] HAN H, LIU X. Current application status of probiotics in the treatment of acute pancreatitis[J]. Clin J Med Offic, 2021, 49( 4): 374- 375, 379. DOI: 10.16680/j.1671-3826.2021.04.05.韩浩, 刘旭. 益生菌在急性胰腺炎治疗中应用现状[J]. 临床军医杂志, 2021, 49( 4): 374- 375, 379. DOI: 10.16680/j.1671-3826.2021.04.05. [48] LU WW, CHEN X, NI JL, et al. The role of gut microbiota in the pathogenesis and treatment of acute pancreatitis: A narrative review[J]. Ann Palliat Med, 2021, 10( 3): 3445- 3451. DOI: 10.21037/apm-21-429. [49] LUO YY, LIU X. Research progress in probiotic assisted treatment of severe acute pancreatitis[J]. Trauma and Crit Medicine, 2021, 9( 2): 161- 164. DOI: 10.16048/j.issn.2095-5561.2021.02.22.罗娅媛, 刘旭. 益生菌辅助治疗重症急性胰腺炎研究进展[J]. 创伤与急危重病医学, 2021, 9( 2): 161- 164. DOI: 10.16048/j.issn.2095-5561.2021.02.22. -



 PDF下载 ( 1192 KB)
PDF下载 ( 1192 KB)


 下载:
下载: