| [1] |
PALATINI M, MÜLLER SF, LOWJAGA K, et al. Mutational analysis of the GXXXG/A motifs in the human Na(+)/Taurocholate co-transporting polypeptide NTCP on its bile acid transport function and hepatitis B/D virus receptor function[J]. Front Mol Biosci, 2021, 8: 699443. DOI: 10.3389/fmolb.2021.699443. |
| [2] |
YAN H, ZHONG G, XU G, et al. Sodium taurocholate cotransporting polypeptide is a functional receptor for human hepatitis B and D virus[J]. Elife, 2012, 1: e00049. DOI: 10.7554/eLife.00049. |
| [3] |
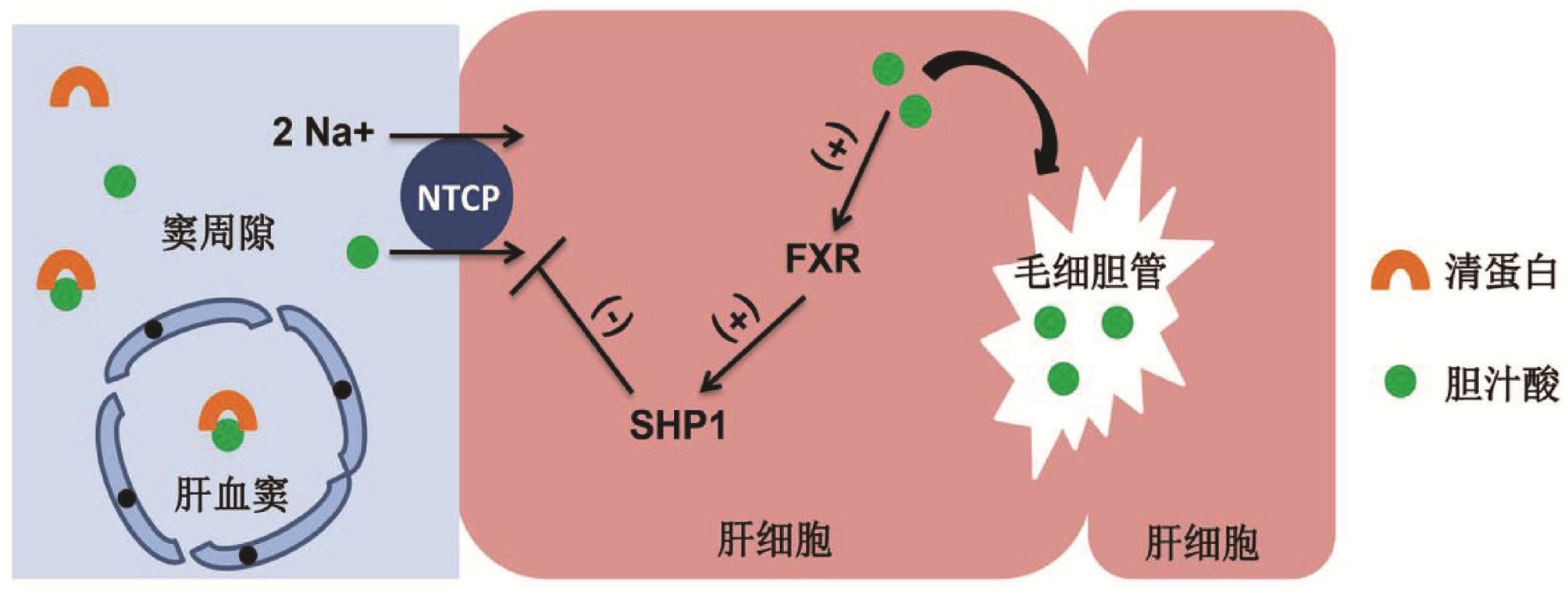
AGUILAR-OLIVOS NE, CARRILLO-CÓRDOVA D, ORIA-HERNÁNDEZ J, et al. The nuclear receptor FXR, but not LXR, up- regulates bile acid transporter expression in non-alcoholic fatty liver disease[J]. Ann Hepatol, 2015, 14(4): 487-493.
|
| [4] |
SALHAB A, AMER J, LU Y, et al. Sodium(+)/taurocholate cotransporting polypeptide as target therapy for liver fibrosis[J]. Gut, 2021. DOI: 10.1136/gutjnl-2020-323345.[Online ahead of print] |
| [5] |
TAKEYAMA Y, SAKISAKA S. Hepatobiliary membrane transporters in primary biliary cirrhosis[J]. Hepatol Res, 2012, 42(2): 120-130. DOI: 10.1111/j.1872-034X.2011.00912.x. |
| [6] |
BINH MT, HOAN NX, van TONG H, et al. NTCP S267F variant associates with decreased susceptibility to HBV and HDV infection and decelerated progression of related liver diseases[J]. Int J Infect Dis, 2019, 80: 147-152. DOI: 10.1016/j.ijid.2019.01.038. |
| [7] |
APPELMAN MD, WETTENGEL JM, PROTZER U, et al. Molecular regulation of the hepatic bile acid uptake transporter and HBV entry receptor NTCP[J]. Biochim Biophys Acta Mol Cell Biol Lipids, 2021, 1866(8): 158960. DOI: 10.1016/j.bbalip.2021.158960. |
| [8] |
WETTENGEL JM, BURWITZ BJ. Innovative HBV animal models based on the entry receptor NTCP[J]. Viruses, 2020, 12(8): 828. DOI: 10.3390/v12080828. |
| [9] |
FUKANO K, OSHIMA M, TSUKUDA S, et al. NTCP oligomerization occurs downstream of the NTCP-EGFR interaction during hepatitis B virus internalization[J]. J Virol, 2021, 95(24): e0093821. DOI: 10.1128/JVI.00938-21. |
| [10] |
MARENINOVA O, SHIN JM, VAGIN O, et al. Topography of the membrane domain of the liver Na +-dependent bile acid transporter[J]. Biochemistry, 2005, 44(42): 13702-13712. DOI: 10.1021/bi051291x. |
| [11] |
KIM JY, KIM KH, LEE JA, et al. Transporter-mediated bile acid uptake causes Ca 2+-dependent cell death in rat pancreatic acinar cells[J]. Gastroenterology, 2002, 122(7): 1941-1953. DOI: 10.1053/gast.2002.33617. |
| [12] |
RUSSELL DW. Fifty years of advances in bile acid synthesis and metabolism[J]. J Lipid Res, 2009, 50 (Suppl): S120-S125. DOI: 10.1194/jlr.R800026-JLR200. |
| [13] |
STIEGER B. The role of the sodium-taurocholate cotransporting polypeptide (NTCP) and of the bile salt export pump (BSEP) in physiology and pathophysiology of bile formation[J]. Handb Exp Pharmacol, 2011, 201: 205-259. DOI: 10.1007/978-3-642-14541-4_5. |
| [14] |
VERRIER ER, COLPITTS CC, BACH C, et al. Solute carrier NTCP regulates innate antiviral immune responses targeting hepatitis C virus infection of hepatocytes[J]. Cell Rep, 2016, 17(5): 1357-1368. DOI: 10.1016/j.celrep.2016.09.084. |
| [15] |
HO RH, LEAKE BF, ROBERTS RL, et al. Ethnicity-dependent polymorphism in Na +-taurocholate cotransporting polypeptide (SLC10A1) reveals a domain critical for bile acid substrate recognition[J]. J Biol Chem, 2004, 279(8): 7213-7222. DOI: 10.1074/jbc.M305782200. |
| [16] |
SU Z, LI Y, LIAO Y, et al. Association of the gene polymorphisms in sodium taurocholate cotransporting polypeptide with the outcomes of hepatitis B infection in Chinese Han population[J]. Infect Genet Evol, 2014, 27: 77-82. DOI: 10.1016/j.meegid.2014.07.001. |
| [17] |
HU HH, LIU J, LIN YL, et al. The rs2296651 (S267F) variant on NTCP (SLC10A1) is inversely associated with chronic hepatitis B and progression to cirrhosis and hepatocellular carcinoma in patients with chronic hepatitis B[J]. Gut, 2016, 65(9): 1514-1521. DOI: 10.1136/gutjnl-2015-310686. |
| [18] |
YU Y, LI S, LIANG W. Bona fide receptor for hepatitis B and D viral infections: Mechanism, research models and molecular drug targets[J]. Emerg Microbes Infect, 2018, 7(1): 134. DOI: 10.1038/s41426-018-0137-7. |
| [19] |
IMAI S, KIKUCHI R, KUSUHARA H, et al. Analysis of DNA methylation and histone modification profiles of liver-specific transporters[J]. Mol Pharmacol, 2009, 75(3): 568-576. DOI: 10.1124/mol.108.052589. |
| [20] |
HALILBASIC E, CLAUDEL T, TRAUNER M. Bile acid transporters and regulatory nuclear receptors in the liver and beyond[J]. J Hepatol, 2013, 58(1): 155-168. DOI: 10.1016/j.jhep.2012.08.002. |
| [21] |
MAYATI A, LE VEE M, MOREAU A, et al. Protein kinase C-dependent regulation of human hepatic drug transporter expression[J]. Biochem Pharmacol, 2015, 98(4): 703-717. DOI: 10.1016/j.bcp.2015.10.007. |
| [22] |
SARGIACOMO C, EL-KEHDY H, POURCHER G, et al. Age-dependent glycosylation of the sodium taurocholate cotransporter polypeptide: From fetal to adult human livers[J]. Hepatol Commun, 2018, 2(6): 693-702. DOI: 10.1002/hep4.1174. |
| [23] |
FERRELL JM, CHIANG J. Understanding bile acid signaling in diabetes: From pathophysiology to therapeutic targets[J]. Diabetes Metab J, 2019, 43(3): 257-272. DOI: 10.4093/dmj.2019.0043. |
| [24] |
YAN H, PENG B, LIU Y, et al. Viral entry of hepatitis B and D viruses and bile salts transportation share common molecular determinants on sodium taurocholate cotransporting polypeptide[J]. J Virol, 2014, 88(6): 3273-3284. DOI: 10.1128/JVI.03478-13. |
| [25] |
GLEBE D, GOLDMANN N, LAUBER C, et al. HBV evolution and genetic variability: Impact on prevention, treatment and development of antivirals[J]. Antiviral Res, 2021, 186: 104973. DOI: 10.1016/j.antiviral.2020.104973. |
| [26] |
|
| [27] |
LIU Y, RUAN H, LI Y, et al. Potent and specific inhibition of NTCP-Mediated HBV/HDV infection and substrate transporting by a novel, oral-available cyclosporine a analogue[J]. J Med Chem, 2021, 64(1): 543-565. DOI: 10.1021/acs.jmedchem.0c01484. |
| [28] |
DONKERS JM, APPELMAN MD, VAN DE GRAAF S. Mechanistic insights into the inhibition of NTCP by myrcludex B[J]. JHEP Rep, 2019, 1(4): 278-285. DOI: 10.1016/j.jhepr.2019.07.006. |
| [29] |
FUKANO K, TSUKUDA S, WATASHI K, et al. Concept of viral inhibitors via NTCP[J]. Semin Liver Dis, 2019, 39(1): 78-85. DOI: 10.1055/s-0038-1676804. |
| [30] |
HUANG DQ, EL-SERAG HB, LOOMBA R. Global epidemiology of NAFLD-related HCC: Trends, predictions, risk factors and prevention[J]. Nat Rev Gastroenterol Hepatol, 2021, 18(4): 223-238. DOI: 10.1038/s41575-020-00381-6. |
| [31] |
HARRISON SA, NEFF G, GUY CD, et al. Efficacy and safety of aldafermin, an engineered FGF19 analog, in a randomized, double-blind, placebo-controlled trial of patients with nonalcoholic steatohepatitis[J]. Gastroenterology, 2021, 160(1): 219-231. e1. DOI: 10.1053/j.gastro.2020.08.004. |
| [32] |
BECHMANN LP, KOCABAYOGLU P, SOWA JP, et al. Free fatty acids repress small heterodimer partner (SHP) activation and adiponectin counteracts bile acid-induced liver injury in superobese patients with nonalcoholic steatohepatitis[J]. Hepatology, 2013, 57(4): 1394-1406. DOI: 10.1002/hep.26225. |
| [33] |
FERSLEW BC, XIE G, JOHNSTON CK, et al. Altered bile acid metabolome in patients with nonalcoholic steatohepatitis[J]. Dig Dis Sci, 2015, 60(11): 3318-3328. DOI: 10.1007/s10620-015-3776-8. |
| [34] |
CHO EJ, YOON JH, KWAK MS, et al. Tauroursodeoxycholic acid attenuates progression of steatohepatitis in mice fed a methionine-choline-deficient diet[J]. Dig Dis Sci, 2014, 59(7): 1461-1474. DOI: 10.1007/s10620-014-3217-0. |
| [35] |
KISSELEVA T, BRENNER D. Molecular and cellular mechanisms of liver fibrosis and its regression[J]. Nat Rev Gastroenterol Hepatol, 2021, 18(3): 151-166. DOI: 10.1038/s41575-020-00372-7. |
| [36] |
SVEGLIATI-BARONI G, RIDOLFI F, HANNIVOORT R, et al. Bile acids induce hepatic stellate cell proliferation via activation of the epidermal growth factor receptor[J]. Gastroenterology, 2005, 128(4): 1042-1055. DOI: 10.1053/j.gastro.2005.01.007. |
| [37] |
TANAKA A. Current understanding of primary biliary cholangitis[J]. Clin Mol Hepatol, 2021, 27(1): 1-21. DOI: 10.3350/cmh.2020.0028. |
| [38] |
KOJIMA H, NIES AT, KÖNIG J, et al. Changes in the expression and localization of hepatocellular transporters and radixin in primary biliary cirrhosis[J]. J Hepatol, 2003, 39(5): 693-702. DOI: 10.1016/s0168-8278(03)00410-0. |
| [39] |
HONDA A, IKEGAMI T, NAKAMUTA M, et al. Anticholestatic effects of bezafibrate in patients with primary biliary cirrhosis treated with ursodeoxycholic acid[J]. Hepatology, 2013, 57(5): 1931-1941. DOI: 10.1002/hep.26018. |
| [40] |
MING J, XU Q, GAO L, et al. Kinsenoside alleviates 17α-ethinylestradiol-induced cholestatic liver injury in rats by inhibiting inflammatory responses and regulating FXR-mediated bile acid homeostasis[J]. Pharmaceuticals (Basel), 2021, 14(5): 452. DOI: 10.3390/ph14050452. |
| [41] |
LOOSEN SH, CASTOLDI M, JÖRDENS MS, et al. Serum levels of circulating microRNA-107 are elevated in patients with early-stage HCC[J]. PLoS One, 2021, 16(3): e0247917. DOI: 10.1371/journal.pone.0247917. |
| [42] |
ZOLLNER G, WAGNER M, FICKERT P, et al. Hepatobiliary transporter expression in human hepatocellular carcinoma[J]. Liver Int, 2005, 25(2): 367-379. DOI: 10.1111/j.1478-3231.2005.01033.x. |
| [43] |
KANG J, WANG J, CHENG J, et al. Down-regulation of NTCP expression by cyclin D1 in hepatitis B virus-related hepatocellular carcinoma has clinical significance[J]. Oncotarget, 2017, 8(34): 56041-56050. DOI: 10.18632/oncotarget.10241. |
| [44] |
JING YY, LIU WT, GUO SW, et al. Hepatitis B virus (HBV) receptors: Deficiency in tumor results in scant HBV infection and overexpression in peritumor leads to higher recurrence risk[J]. Oncotarget, 2015, 6(40): 42952-42962. DOI: 10.18632/oncotarget.5518. |
| [45] |
JANG ES, YOON JH, LEE SH, et al. Sodium taurocholate cotransporting polypeptide mediates dual actions of deoxycholic acid in human hepatocellular carcinoma cells: enhanced apoptosis versus growth stimulation[J]. J Cancer Res Clin Oncol, 2014, 140(1): 133-144. DOI: 10.1007/s00432-013-1554-6. |






 DownLoad:
DownLoad: