| [1] |
MCGLYNN K A, PETRICK JL, EL-SERAG HB. Epidemiology of hepatocellular carcinoma[J]. Hepatology, 2021, 73(Suppl 1): 4-13. DOI: 10.1002/hep.31288. |
| [2] |
SUNG H, FERLAY J, SIEGEL RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71(3): 209-249. DOI: 10.3322/caac.21660. |
| [3] |
NAN Y, AN J, BAO J, et al. The Chinese Society of Hepatology position statement on the redefinition of fatty liver disease[J]. J Hepatol, 2021, 75(2): 454-461. DOI: 10.1016/j.jhep.2021.05.003. |
| [4] |
European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma[J]. J Hepatol, 2018, 69(1): 182-236. DOI: 10.1016/j.jhep.2018.03.019. |
| [5] |
HEIMBACH JK, KULIK LM, FINN RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma[J]. Hepatology, 2018, 67(1): 358-380. DOI: 10.1002/hep.29086. |
| [6] |
ESLAM M, SARIN SK, WONG VW, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease[J]. Hepatol Int, 2020, 14(6): 889-919. DOI: 10.1007/s12072-020-10094-2. |
| [7] |
STINE JG, WENTWORTH BJ, ZIMMET A, et al. Systematic review with meta-analysis: Risk of hepatocellular carcinoma in non-alcoholic steatohepatitis without cirrhosis compared to other liver diseases[J]. Aliment Pharmacol Ther, 2018, 48(7): 696-703. DOI: 10.1111/apt.14937. |
| [8] |
PISCAGLIA F, SVEGLIATI-BARONI G, BARCHETTI A, et al. Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver disease: A multicenter prospective study[J]. Hepatology, 2016, 63(3): 827-838. DOI: 10.1002/hep.28368. |
| [9] |
HUANG DQ, EL-SERAG HB, LOOMBA R. Global epidemiology of NAFLD-related HCC: Trends, predictions, risk factors and prevention[J]. Nat Rev Gastroenterol Hepatol, 2021, 18(4): 223-238. DOI: 10.1038/s41575-020-00381-6. |
| [10] |
YOUNOSSI Z, STEPANOVA M, ONG JP, et al. Nonalcoholic steatohepatitis is the fastest growing cause of hepatocellular carcinoma in liver transplant candidates[J]. Clin Gastroenterol Hepatol, 2019, 17(4): 748-755. e3. DOI: 10.1016/j.cgh.2018.05.057. |
| [11] |
YOUNOSSI ZM, OTGONSUREN M, HENRY L, et al. Association of nonalcoholic fatty liver disease (NAFLD) with hepatocellular carcinoma (HCC) in the United States from 2004 to 2009[J]. Hepatology, 2015, 62(6): 1723-1730. DOI: 10.1002/hep.28123. |
| [12] |
PAIS R, FARTOUX L, GOUMARD C, et al. Temporal trends, clinical patterns and outcomes of NAFLD-related HCC in patients undergoing liver resection over a 20-year period[J]. Aliment Pharmacol Ther, 2017, 46(9): 856-863. DOI: 10.1111/apt.14261. |
| [13] |
ZHOU F, ZHOU J, WANG W, et al. Unexpected rapid increase in the burden of NAFLD in China from 2008 to 2018: A systematic review and Meta-analysis[J]. Hepatology, 2019, 70(4): 1119-1133. DOI: 10.1002/hep.30702. |
| [14] |
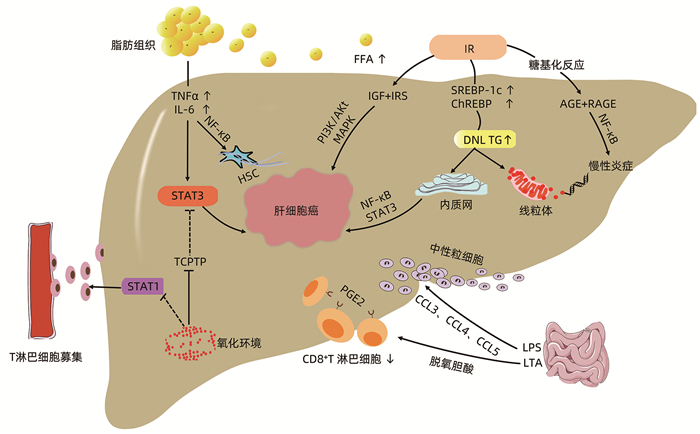
PARK EJ, LEE JH, YU GY, et al. Dietary and genetic obesity promote liver inflammation and tumorigenesis by enhancing IL-6 and TNF expression[J]. Cell, 2010, 140(2): 197-208. DOI: 10.1016/j.cell.2009.12.052. |
| [15] |
CZAUDERNA C, CASTVEN D, MAHN FL, et al. Context-dependent role of NF-κB signaling in primary liver cancer-from tumor development to therapeutic implications[J]. Cancers (Basel), 2019, 11(8): 1053. DOI: 10.3390/cancers11081053. |
| [16] |
GROHMANN M, WIEDE F, DODD GT, et al. Obesity drives STAT-1-dependent NASH and STAT-3-dependent HCC[J]. Cell, 2018, 175(5): 1289-1306. e20. DOI: 10.1016/j.cell.2018.09.053. |
| [17] |
ARROYAVE-OSPINA JC, WU Z, GENG Y, et al. Role of oxidative stress in the pathogenesis of non-alcoholic fatty liver disease: Implications for prevention and therapy[J]. Antioxidants (Basel), 2021, 10(2): 174. DOI: 10.3390/antiox10020174. |
| [18] |
LEBEAUPIN C, VALLÉE D, HAZARI Y, et al. Endoplasmic reticulum stress signalling and the pathogenesis of non-alcoholic fatty liver disease[J]. J Hepatol, 2018, 69(4): 927-947. DOI: 10.1016/j.jhep.2018.06.008. |
| [19] |
WU Y, SHAN B, DAI J, et al. Dual role for inositol-requiring enzyme 1α in promoting the development of hepatocellular carcinoma during diet-induced obesity in mice[J]. Hepatology, 2018, 68(2): 533-546. DOI: 10.1002/hep.29871. |
| [20] |
SCHWABE RF, GRETEN TF. Gut microbiome in HCC - Mechanisms, diagnosis and therapy[J]. J Hepatol, 2020, 72(2): 230-238. DOI: 10.1016/j.jhep.2019.08.016. |
| [21] |
PONZIANI FR, BHOORI S, CASTELLI C, et al. Hepatocellular carcinoma is associated with gut microbiota profile and inflammation in nonalcoholic fatty liver disease[J]. Hepatology, 2019, 69(1): 107-120. DOI: 10.1002/hep.30036. |
| [22] |
LOO TM, KAMACHI F, WATANABE Y, et al. Gut microbiota promotes obesity-associated liver cancer through PGE2-mediated suppression of antitumor immunity[J]. Cancer Discov, 2017, 7(5): 522-538. DOI: 10.1158/2159-8290.CD-16-0932. |
| [23] |
YUAN J, CHEN C, CUI J, et al. Fatty liver disease caused by high-alcohol-producing Klebsiella pneumoniae[J]. Cell Metab, 2019, 30(4): 675-688. e7. DOI: 10.1016/j.cmet.2019.08.018. |
| [24] |
SMITH GI, SHANKARAN M, YOSHINO M, et al. Insulin resistance drives hepatic de novo lipogenesis in nonalcoholic fatty liver disease[J]. J Clin Invest, 2020, 130(3): 1453-1460. DOI: 10.1172/JCI134165. |
| [25] |
FABBRINI E, TIEMANN LUECKING C, LOVE-GREGORY L, et al. Physiological mechanisms of weight gain-induced steatosis in people with obesity[J]. Gastroenterology, 2016, 150(1): 79-81. e2. DOI: 10.1053/j.gastro.2015.09.003. |
| [26] |
WENG CJ, HSIEH YH, TSAI CM, et al. Relationship of insulin-like growth factors system gene polymorphisms with the susceptibility and pathological development of hepatocellular carcinoma[J]. Ann Surg Oncol, 2010, 17(7): 1808-1815. DOI: 10.1245/s10434-009-0904-8. |
| [27] |
JABIR NR, AHMAD S, TABREZ S. An insight on the association of glycation with hepatocellular carcinoma[J]. Semin Cancer Biol, 2018, 49: 56-63. DOI: 10.1016/j.semcancer.2017.06.005. |
| [28] |
BROADFIELD LA, DUARTE J, SCHMIEDER R, et al. Fat induces glucose metabolism in nontransformed liver cells and promotes liver tumorigenesis[J]. Cancer Res, 2021, 81(8): 1988-2001. DOI: 10.1158/0008-5472.CAN-20-1954. |
| [29] |
CANTERO I, ABETE I, BABIO N, et al. Dietary Inflammatory Index and liver status in subjects with different adiposity levels within the PREDIMED trial[J]. Clin Nutr, 2018, 37(5): 1736-1743. DOI: 10.1016/j.clnu.2017.06.027. |
| [30] |
AREM H, LOFTFIELD E, SAINT-MAURICE PF, et al. Physical activity across the lifespan and liver cancer incidence in the NIH-AARP Diet and Health Study cohort[J]. Cancer Med, 2018, 7(4): 1450-1457. DOI: 10.1002/cam4.1343. |
| [31] |
GUO XF, SHAO XF, LI JM, et al. Fruit and vegetable intake and liver cancer risk: A Meta-analysis of prospective cohort studies[J]. Food Funct, 2019, 10(8): 4478-4485. DOI: 10.1039/c9fo00804g. |
| [32] |
SCHMIDT-ARRAS D, ROSE-JOHN S. IL-6 pathway in the liver: From physiopathology to therapy[J]. J Hepatol, 2016, 64(6): 1403-1415. DOI: 10.1016/j.jhep.2016.02.004. |
| [33] |
JUNG KH, YOO W, STEVENSON HL, et al. Multifunctional effects of a small-molecule STAT3 inhibitor on NASH and hepatocellular carcinoma in mice[J]. Clin Cancer Res, 2017, 23(18): 5537-5546. DOI: 10.1158/1078-0432.CCR-16-2253. |
| [34] |
WANG ST, HUANG SW, LIU KT, et al. Atorvastatin-induced senescence of hepatocellular carcinoma is mediated by downregulation of hTERT through the suppression of the IL-6/STAT3 pathway[J]. Cell Death Discov, 2020, 6: 17. DOI: 10.1038/s41420-020-0252-9. |
| [35] |
LEE DE, LEE SJ, KIM SJ, et al. Curcumin ameliorates nonalcoholic fatty liver disease through inhibition of O-GlcNacylation[J]. Nutrients, 2019, 11(11): 2702. DOI: 10.3390/nu11112702. |
| [36] |
SHAO S, DUAN W, XU Q, et al. Curcumin suppresses hepatic stellate cell-induced hepatocarcinoma angiogenesis and invasion through downregulating CTGF[J]. Oxid Med Cell Longev, 2019, 2019: 8148510. DOI: 10.1155/2019/8148510. |
| [37] |
LEE DH, HAN DH, NAM KT, et al. Ezetimibe, an NPC1L1 inhibitor, is a potent Nrf2 activator that protects mice from diet-induced nonalcoholic steatohepatitis[J]. Free Radic Biol Med, 2016, 99: 520-532. DOI: 10.1016/j.freeradbiomed.2016.09.009. |
| [38] |
MIURA K, OHNISHI H, MORIMOTO N, et al. Ezetimibe suppresses development of liver tumors by inhibiting angiogenesis in mice fed a high-fat diet[J]. Cancer Sci, 2019, 110(2): 771-783. DOI: 10.1111/cas.13902. |
| [39] |
LI J, SUNG CY, LEE N, et al. Probiotics modulated gut microbiota suppresses hepatocellular carcinoma growth in mice[J]. Proc Natl Acad Sci U S A, 2016, 113(9): e1306-e1315. DOI: 10.1073/pnas.1518189113. |
| [40] |
FUJINAGA Y, KAWARATANI H, KAYA D, et al. Effective combination therapy of angiotensin-Ⅱ receptor blocker and rifaximin for hepatic fibrosis in rat model of nonalcoholic steatohepatitis[J]. Int J Mol Sci, 2020, 21(15): 5589. DOI: 10.3390/ijms21155589. |
| [41] |
YU LX, SCHWABE RF. The gut microbiome and liver cancer: Mechanisms and clinical translation[J]. Nat Rev Gastroenterol Hepatol, 2017, 14(9): 527-539. DOI: 10.1038/nrgastro.2017.72. |
| [42] |
VILAR-GOMEZ E, VUPPALANCHI R, DESAI AP, et al. Long-term metformin use may improve clinical outcomes in diabetic patients with non-alcoholic steatohepatitis and bridging fibrosis or compensated cirrhosis[J]. Aliment Pharmacol Ther, 2019, 50(3): 317-328. DOI: 10.1111/apt.15331. |
| [43] |
SHANKARAIAH RC, CALLEGARI E, GUERRIERO P, et al. Metformin prevents liver tumourigenesis by attenuating fibrosis in a transgenic mouse model of hepatocellular carcinoma[J]. Oncogene, 2019, 38(45): 7035-7045. DOI: 10.1038/s41388-019-0942-z. |
| [44] |
BOECKMANS J, NATALE A, ROMBAUT M, et al. Human hepatic in vitro models reveal distinct anti-NASH potencies of PPAR agonists[J]. Cell Biol Toxicol, 2021, 37(2): 293-311. DOI: 10.1007/s10565-020-09544-2. |
| [45] |
YANG Y, ZHAO LH, HUANG B, et al. Pioglitazone, a PPARγ agonist, inhibits growth and invasion of human hepatocellular carcinoma via blockade of the rage signaling[J]. Mol Carcinog, 2015, 54(12): 1584-1595. DOI: 10.1002/mc.22231. |







 DownLoad:
DownLoad: