| [1] |
FAN JG. Epidemiology of alcoholic and nonalcoholic fatty liver disease in China[J]. J Gastroenterol Hepatol, 2013, 28( Suppl 1): 11- 17. DOI: 10.1111/jgh.12036. |
| [2] |
LAZARUS JV, MARK HE, VILLOTA-RIVAS M, et al. The global NAFLD policy review and preparedness index: Are countries ready to address this silent public health challenge?[J]. J Hepatol, 2022, 76( 4): 771- 780. DOI: 10.1016/j.jhep.2021.10.025. |
| [3] |
YOUNOSSI ZM, KOENIG AB, ABDELATIF D, et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes[J]. Hepatology, 2016, 64( 1): 73- 84. DOI: 10.1002/hep.28431. |
| [4] |
CHEN SD, ZHOU HH, ZHAO ZX, et al. Jiangzhi and Hepatoprotective effect of salidroside on nonalcoholic fatty liver disease[J]. China J Tradit Chin Med Pharm, 2013, 28( 9): 2701- 2703.
陈少东, 周海虹, 赵正晓, 等. 红景天苷对非酒精性脂肪性肝炎的降脂保肝作用研究[J]. 中华中医药杂志, 2013, 28( 9): 2701- 2703.
|
| [5] |
YANG ZR, WANG HF, ZUO TC, et al. Salidroside alleviates oxidative stress in the liver with non- alcoholic steatohepatitis in rats[J]. BMC Pharmacol Toxicol, 2016, 17: 16. DOI: 10.1186/s40360-016-0059-8. |
| [6] |
SUN P, SONG SZ, JIANG S, et al. Salidroside regulates inflammatory response in raw 264.7 macrophages via TLR4/TAK1 and ameliorates inflammation in alcohol binge drinking-induced liver injury[J]. Molecules, 2016, 21( 11): 1490. DOI: 10.3390/molecules21111490. |
| [7] |
ZHANG Z, PING J, XU LM. Screening Chinese medicine components for inhibition of human hepatic stellate cell migration[J]. J Clin Hepatol, 2012, 28( 3): 183- 188, 191. DOI: 10.3969/j.issn.1001-5256.2012.03.007. |
| [8] |
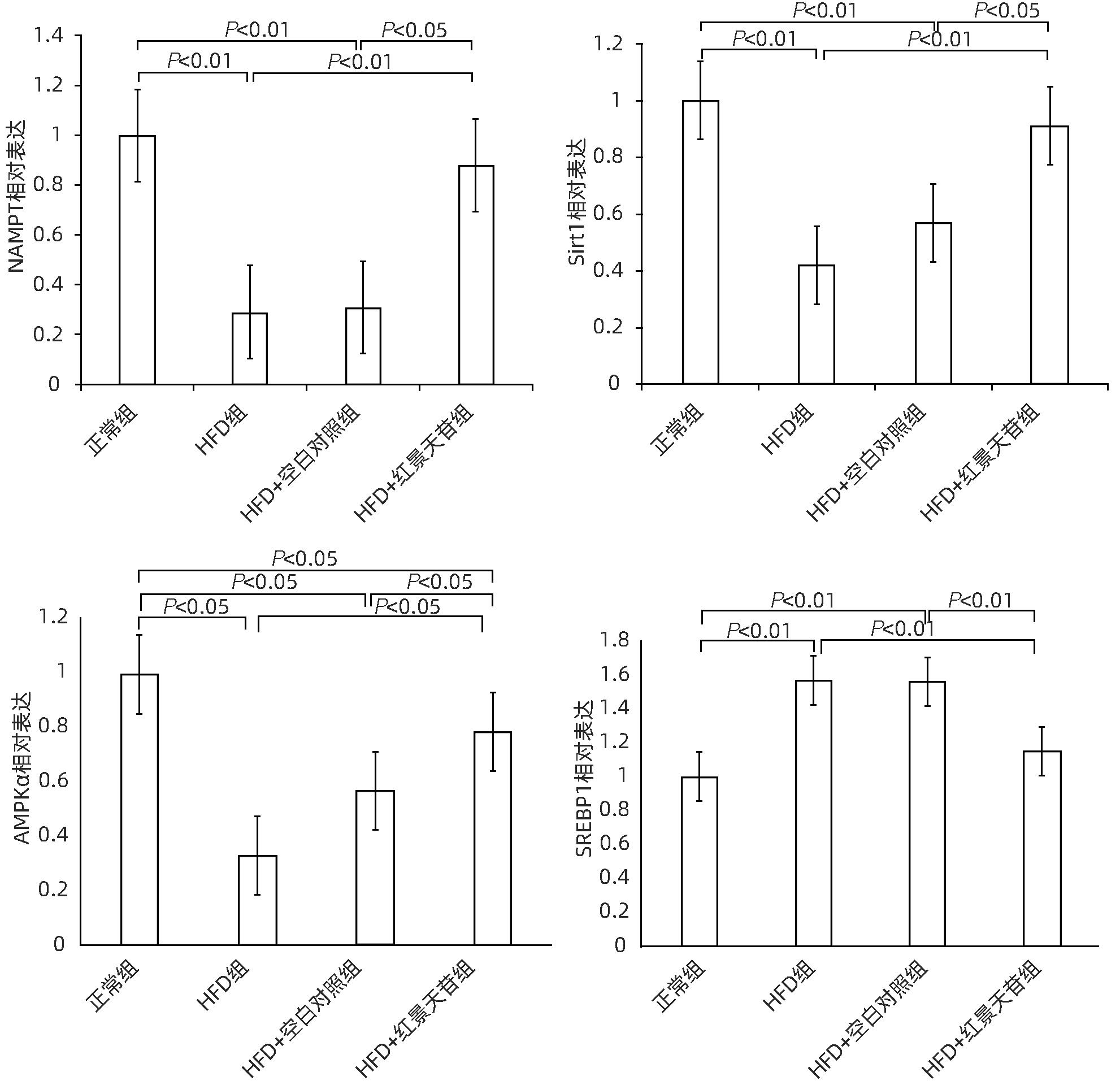
WANG LF, WANG XN, HUANG CC, et al. Inhibition of NAMPT aggravates high fat diet-induced hepatic steatosis in mice through regulating Sirt1/AMPKα/SREBP1 signaling pathway[J]. Lipids Health Dis, 2017, 16( 1): 82. DOI: 10.1186/s12944-017-0464-z. |
| [9] |
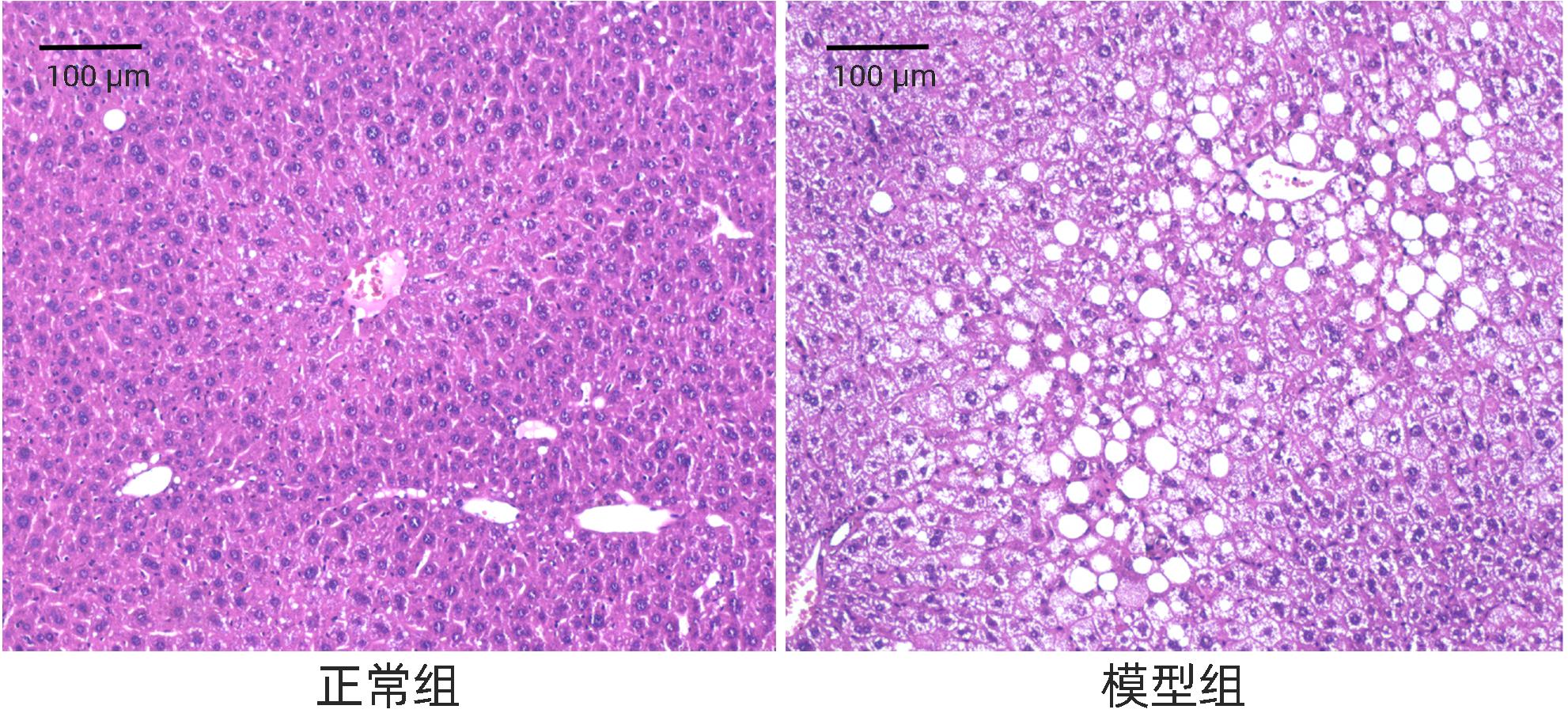
KOBYLIAK N, ABENAVOLI L. The role of liver biopsy to assess non-alcoholic fatty liver disease[J]. Rev Recent Clin Trials, 2014, 9( 3): 159- 169. DOI: 10.2174/1574887109666141216102231. |
| [10] |
ALAMEDDINE A, FAJLOUN Z, BOURREAU J, et al. The cardiovascular effects of salidroside in the Goto-Kakizaki diabetic rat model[J]. J Physiol Pharmacol, 2015, 66( 2): 249- 257.
|
| [11] |
WANG SY, ZHAO XX, YANG SX, et al. Salidroside alleviates high glucose-induced oxidative stress and extracellular matrix accumulation in rat glomerular mesangial cells by the TXNIP-NLRP3 inflammasome pathway[J]. Chem Biol Interact, 2017, 278: 48- 53. DOI: 10.1016/j.cbi.2017.10.012. |
| [12] |
FAN XJ, WANG Y, WANG L, et al. Salidroside induces apoptosis and autophagy in human colorectal cancer cells through inhibition of PI3K/Akt/mTOR pathway[J]. Oncol Rep, 2016, 36( 6): 3559- 3567. DOI: 10.3892/or.2016.5138. |
| [13] |
WANG MH, LUO L, YAO LL, et al. Salidroside improves glucose homeostasis in obese mice by repressing inflammation in white adipose tissues and improving leptin sensitivity in hypothalamus[J]. Sci Rep, 2016, 6: 25399. DOI: 10.1038/srep25399. |
| [14] |
GUO Y, WANG SY, YI JJ, et al. Effect of salidroside on apoptosis of CD71 + nucleated red blood cells in bone marrow in high altitude polycythemia model rats[J]. J Jilin Univ(Med Ed), 2023, 49( 5): 1174- 1181. DOI: 10.13481/j.1671-587X.20230510. |
| [15] |
DAI N, ZOU Y, WANG HF, et al. Inhibitory effect of salidroside on liver oxidative stress in rats with non-alcoholic steatohepatitis[J]. Chin J Pathophysiol, 2013, 29( 9): 1704- 1708. DOI: 10.3969/j.issn.1000-4718.2013.09.030. |
| [16] |
ZHANG XR. The mechanism of salidroside regulating glucose and lipid metabolism in type 2 diabetes mice through microRNA[D]. Changchun: Jilin University, 2016.
张新茹. 红景天苷在2型糖尿病小鼠中通过microRNA改善糖脂代谢的机制研究[D]. 长春: 吉林大学, 2016.
|
| [17] |
WU TF, LIAO XH, ZHONG BH. Epidemiology of nonalcoholic fatty liver disease in some regions of China[J]. J Clin Hepatol, 2020, 36( 6): 1370- 1373. DOI: 10.3969/j.issn.1001-5256.2020.06.039. |
| [18] |
LI YY, XIE ZY. Advances in the etiology and treatment of non-obese nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2021, 37( 2): 452- 457. DOI: 10.3969/j.issn.1001-5256.2021.02.043. |
| [19] |
National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association, Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: A 2018 update[J]. J Clin Hepatol, 2018, 34( 5): 947- 957. DOI: 10.3969/j.issn.1001-5256.2018.05.007. |
| [20] |
RONGVAUX A, SHEA RJ, MULKS MH, et al. Pre-B-cell colony-enhancing factor, whose expression is up-regulated in activated lymphocytes, is a nicotinamide phosphoribosyltransferase, a cytosolic enzyme involved in NAD biosynthesis[J]. Eur J Immunol, 2002, 32( 11): 3225- 3234. DOI: 3.0.CO;2-L">10.1002/1521-4141(200211)32: 11<3225: AID-IMMU3225>3.0.CO;2-L.
|
| [21] |
KOHJIMA M, HIGUCHI N, KATO M, et al. SREBP-1c, regulated by the insulin and AMPK signaling pathways, plays a role in nonalcoholic fatty liver disease[J]. Int J Mol Med, 2008, 21( 4): 507- 511.
|
| [22] |
JEON TI, OSBORNE TF. SREBPs: Metabolic integrators in physiology and metabolism[J]. Trends Endocrinol Metab, 2012, 23( 2): 65- 72. DOI: 10.1016/j.tem.2011.10.004. |







 DownLoad:
DownLoad: