| [1] |
YOUNOSSI Z, ANSTEE QM, MARIETTI M, et al. Global burden of NAFLD and NASH: Trends, predictions, risk factors and prevention[J]. Nat Rev Gastroenterol Hepatol, 2018, 15(1): 11-20. DOI: 10.1038/nrgastro.2017.109. |
| [2] |
ESTES C, ANSTEE QM, ARIAS-LOSTE MT, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016-2030[J]. J Hepatol, 2018, 69(4): 896-904. DOI: 10.1016/j.jhep.2018.05.036. |
| [3] |
WATT MJ, MIOTTO PM, de NARDO W, et al. The liver as an endocrine organ-linking NAFLD and insulin resistance[J]. Endocr Rev, 2019, 40(5): 1367-1393. DOI: 10.1210/er.2019-00034. |
| [4] |
TILG H, MOSCHEN AR, RODEN M. NAFLD and diabetes mellitus[J]. Nat Rev Gastroenterol Hepatol, 2017, 14(1): 32-42. DOI: 10.1038/nrgastro.2016.147. |
| [5] |
SANTHEKADUR PK, KUMAR DP, SANYAL AJ. Preclinical models of non-alcoholic fatty liver disease[J]. J Hepatol, 2018, 68(2): 230-237. DOI: 10.1016/j.jhep.2017.10.031. |
| [6] |
GIL Á, PLAZA-DIAZ J, MESA MD. Vitamin D: Classic and novel actions[J]. Ann Nutr Metab, 2018, 72(2): 87-95. DOI: 10.1159/000486536. |
| [7] |
CIEBIERA M, WŁODARCZYK M, CIEBIERA M, et al. Vitamin D and uterine fibroids-review of the literature and novel concepts[J]. Int J Mol Sci, 2018, 19(7): 2051. DOI: 10.3390/ijms19072051. |
| [8] |
MARADANA MR, YEKOLLU SK, ZENG B, et al. Immunomodulatory liposomes targeting liver macrophages arrest progression of nonalcoholic steatohepatitis[J]. Metabolism, 2018, 78: 80-94. DOI: 10.1016/j.metabol.2017.09.002. |
| [9] |
LIU XJ, WANG BW, ZHANG C, et al. Vitamin D deficiency attenuates high-fat diet-induced hyperinsulinemia and hepatic lipid accumulation in male mice[J]. Endocrinology, 2015, 156(6): 2103-2113. DOI: 10.1210/en.2014-2037. |
| [10] |
ZHAN ZM, JIANG YQ, HU ZJ, et al. Relationship between serum IL-18 expression level and liver injury in children with fatty liver[J]. Exp Lab Med, 2017, 35(2): 274-275, 283. DOI: 10.3969/j.issn.1674-1129.2017.02.047. |
| [11] |
DENG J, ZHANG YH, DANG SS, et al. The change in the prevalence of fatty liver disease and related influencing factors among Karamay residents in 2009-2016 and related influencing factors[J]. J Clin Hepatol, 2021, 37(7): 1609-1613. DOI: 10.3969/j.issn.1001-5256.2021.07.026. |
| [12] |
National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association; Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: A 2018 update[J]. J Clin Hepatol, 2018, 34(5): 947-957. DOI: 10.3969/j.issn.1001-5256.2018.05.007. |
| [13] |
PLUDOWSKI P, HOLICK MF, GRANT WB, et al. Vitamin D supplementation guidelines[J]. J Steroid Biochem Mol Biol, 2018, 175: 125-135. DOI: 10.1016/j.jsbmb.2017.01.021. |
| [14] |
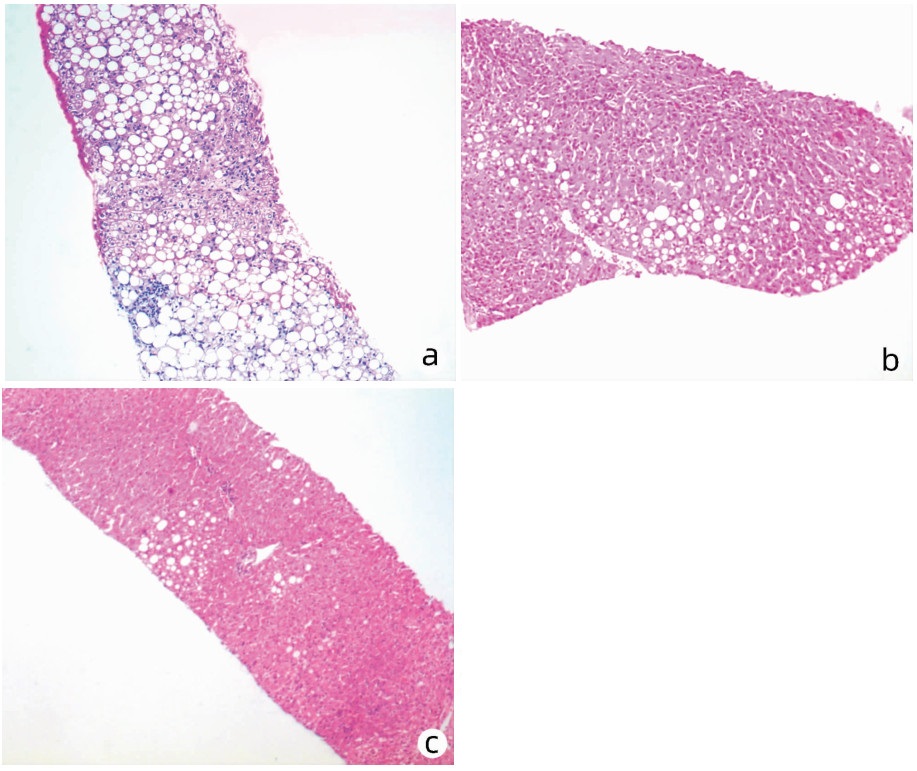
KLEINER DE, BRUNT EM. Nonalcoholic fatty liver disease: Pathologic patterns and biopsy evaluation in clinical research[J]. Semin Liver Dis, 2012, 32(1): 3-13. DOI: 10.1055/s-0032-1306421. |
| [15] |
ZHANG RC, WANG AZ. Experience in the application of diagnostic criteria for nonalcoholic fatty liver (Draft) (With pathological analysis of 30 cases)[J]. Mod Pract Med, 2002, 14(12): 657-658. DOI: 10.3969/j.issn.1671-0800.2002.12.015. |
| [16] |
SIVELL C. Nonalcoholic fatty liver disease: A silent epidemic[J]. Gastroenterol Nurs, 2019, 42(5): 428-434. DOI: 10.1097/SGA.0000000000000443. |
| [17] |
CHAKRAVARTHY MV, WADDELL T, BANERJEE R, et al. Nutrition and nonalcoholic fatty liver disease: Current perspectives[J]. Gastroenterol Clin North Am, 2020, 49(1): 63-94. DOI: 10.1016/j.gtc.2019.09.003. |
| [18] |
YOUNOSSI Z, TACKE F, ARRESE M, et al. Global perspectives on nonalcoholic fatty liver disease and nonalcoholic steatohepatitis[J]. Hepatology, 2019, 69(6): 2672-2682. DOI: 10.1002/hep.30251. |
| [19] |
YEO SC, ONG WM, CHENG K, et al. Weight loss after bariatric surgery predicts an improvement in the non-alcoholic fatty liver disease (NAFLD) fibrosis score[J]. Obes Surg, 2019, 29(4): 1295-1300. DOI: 10.1007/s11695-018-03676-5. |
| [20] |
WONG GL. Update of liver fibrosis and steatosis with transient elastography (Fibroscan)[J]. Gastroenterol Rep (Oxf), 2013, 1(1): 19-26. DOI: 10.1093/gastro/got007. |
| [21] |
SACERDOTE A, DAVE P, LOKSHIN V, et al. Type 2 diabetes mellitus, insulin resistance, and vitamin D[J]. Curr Diab Rep, 2019, 19(10): 101. DOI: 10.1007/s11892-019-1201-y. |
| [22] |
HU TP, TANG SD, YU ZB. Relationship between Vitamin D level in children and adolescents with nonalcoholic fatty liver disease: A Meta-analysis[J]. J Clin Hepatol, 2021, 37(3): 627-631. DOI: 10.3969/j.issn.1001-5256.2021.03.024. |
| [23] |
DABBAGHMANESH MH, DANAFAR F, ESHRAGHIAN A, et al. Vitamin D supplementation for the treatment of non-alcoholic fatty liver disease: A randomized double blind placebo controlled trial[J]. Diabetes Metab Syndr, 2018, 12(4): 513-517. DOI: 10.1016/j.dsx.2018.03.006. |
| [24] |
GEIER A, EICHINGER M, STIRNIMANN G, et al. Treatment of non-alcoholic steatohepatitis patients with vitamin D: A double-blinded, randomized, placebo-controlled pilot study[J]. Scand J Gastroenterol, 2018, 53(9): 1114-1120. DOI: 10.1080/00365521.2018.1501091. |
| [25] |
MARWAHA RK, YENAMANDRA VK, SREENIVAS V, et al. Regional and seasonal variations in ultraviolet B irradiation and vitamin D synthesis in India[J]. Osteoporos Int, 2016, 27(4): 1611-1617. DOI: 10.1007/s00198-015-3427-0. |
| [26] |
SERRANO MA, CAÑADA J, MORENO JC, et al. Solar ultraviolet doses and vitamin D in a northern mid-latitude[J]. Sci Total Environ, 2017, 574: 744-750. DOI: 10.1016/j.scitotenv.2016.09.102. |
| [27] |
HARRISON SA, GOODMAN Z, JABBAR A, et al. A randomized, placebo-controlled trial of emricasan in patients with NASH and F1-F3 fibrosis[J]. J Hepatol, 2020, 72(5): 816-827. DOI: 10.1016/j.jhep.2019.11.024. |
| [28] |
SAKAI N, van SWERINGEN HL, BELIZAIRE RM, et al. Interleukin-37 reduces liver inflammatory injury via effects on hepatocytes and non-parenchymal cells[J]. J Gastroenterol Hepatol, 2012, 27(10): 1609-1616. DOI: 10.1111/j.1440-1746.2012.07187.x. |







 DownLoad:
DownLoad: