| [1] |
GAGNER M, POMP A, et al. Laparoscopic pylorus-preserving pancreatoduodenectomy[J]. Surg Endosc, 1994, 8(5): 408-410. DOI: 10.1007/bf00642443. |
| [2] |
GIULIANOTTI PC, CORATTI A, ANGELINI M, et al. Robotics in general surgery: Personal experience in a large community hospital[J]. Arch Surg, 2003, 138(7): 777-784. DOI: 10.1001/archsurg.138.7.777. |
| [3] |
STANG A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses[J]. Eur J Epidemiol, 2010, 25(9): 603-605. DOI: 10.1007/s10654-010-9491-z. |
| [4] |
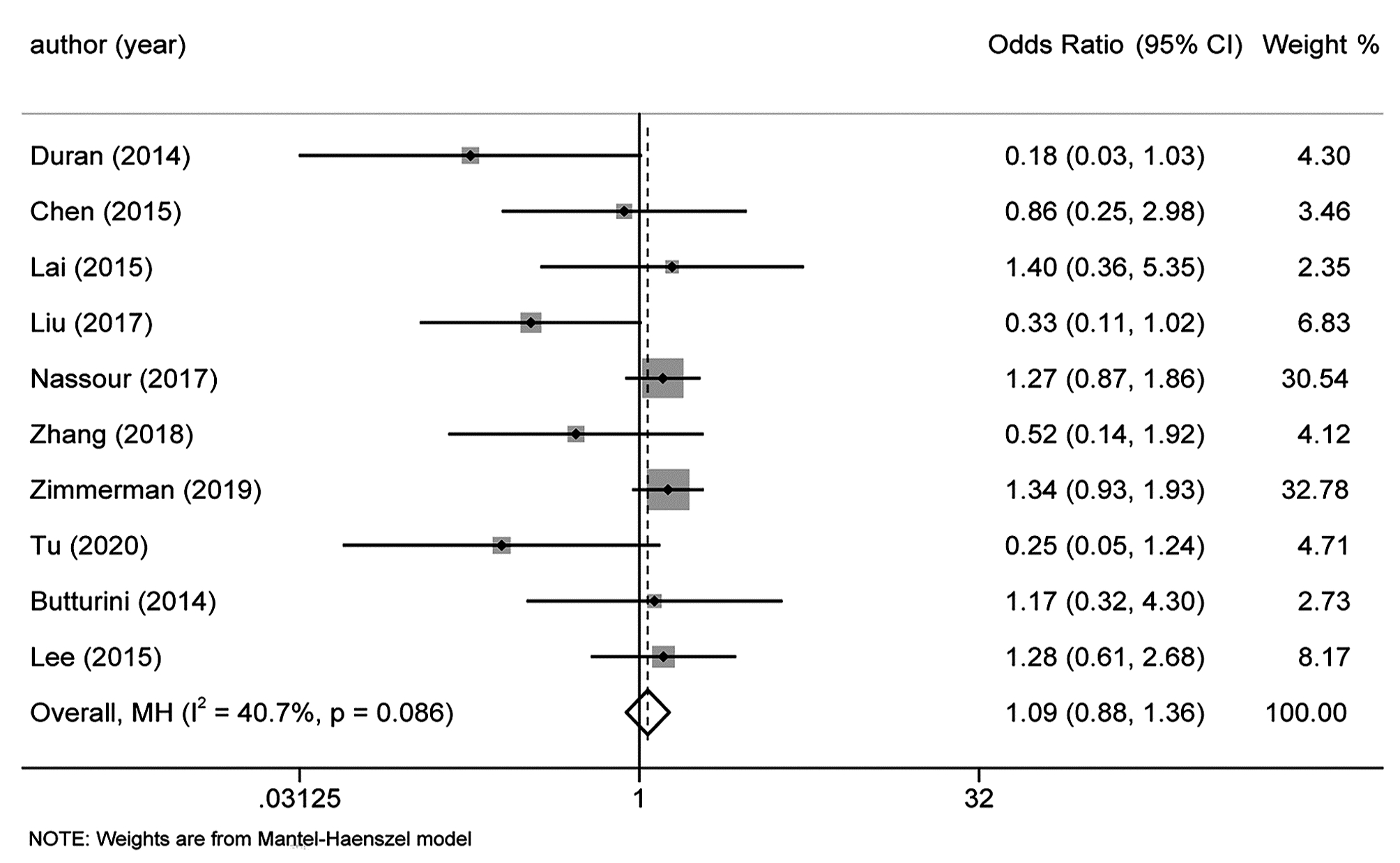
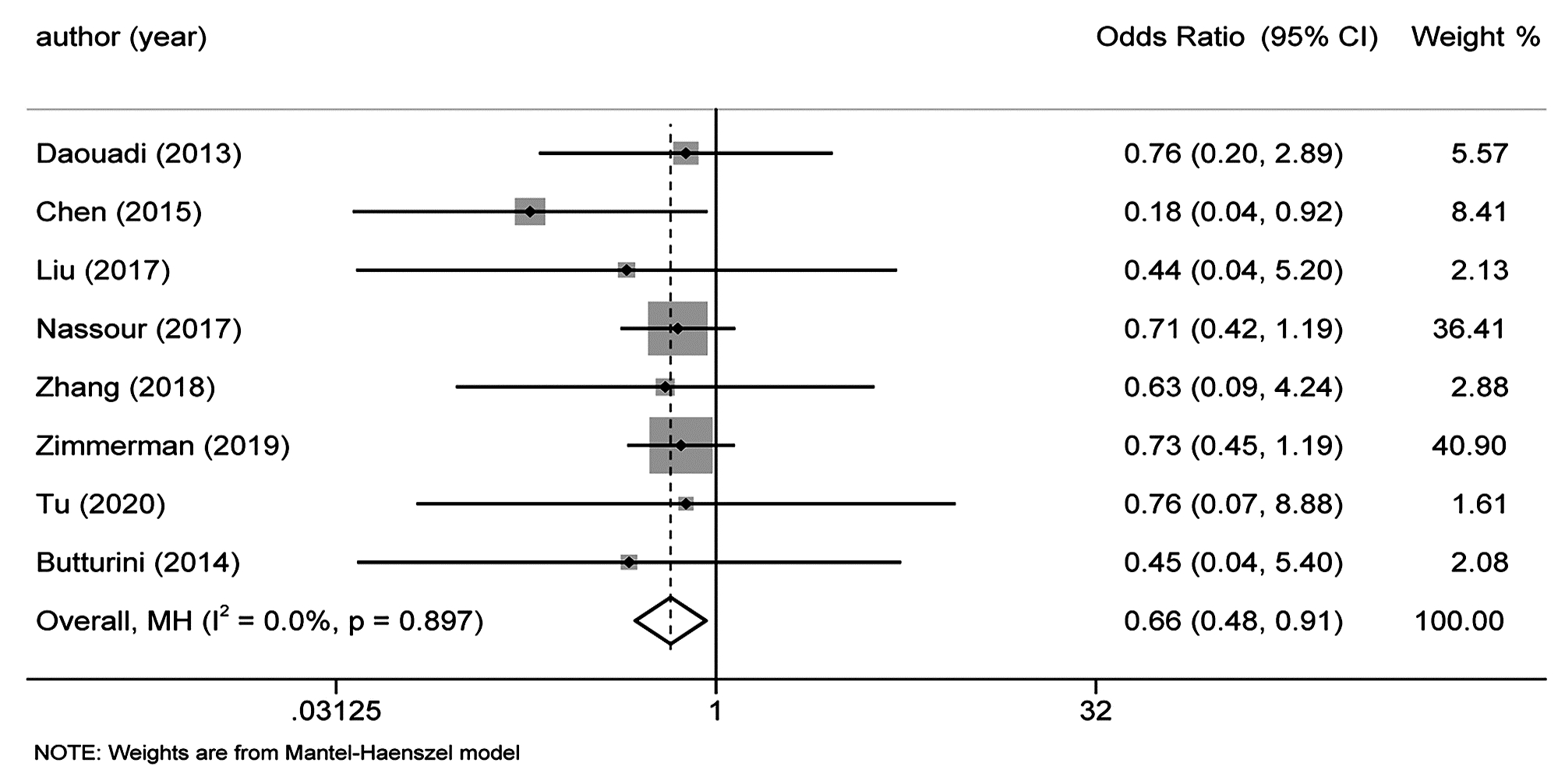
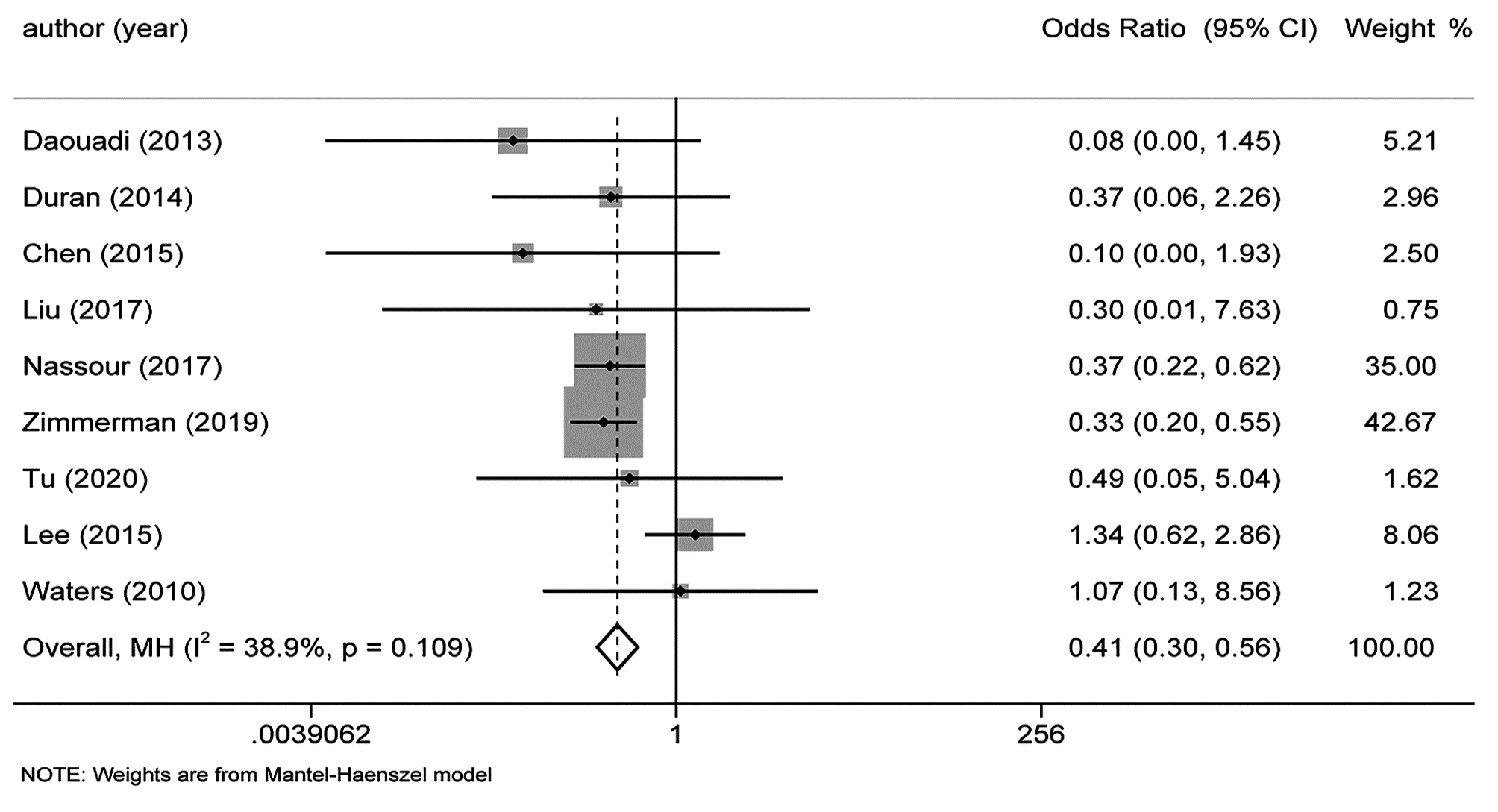
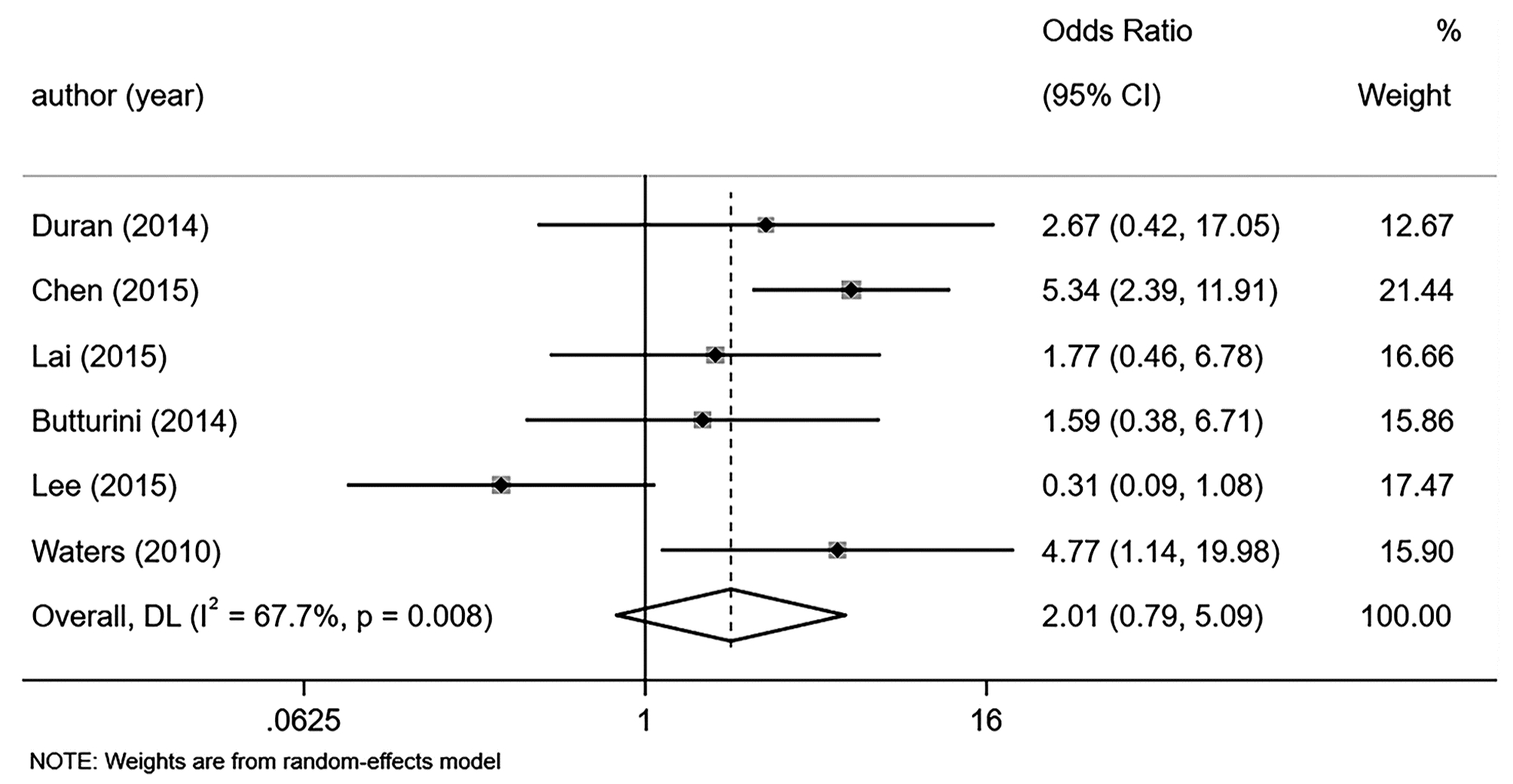
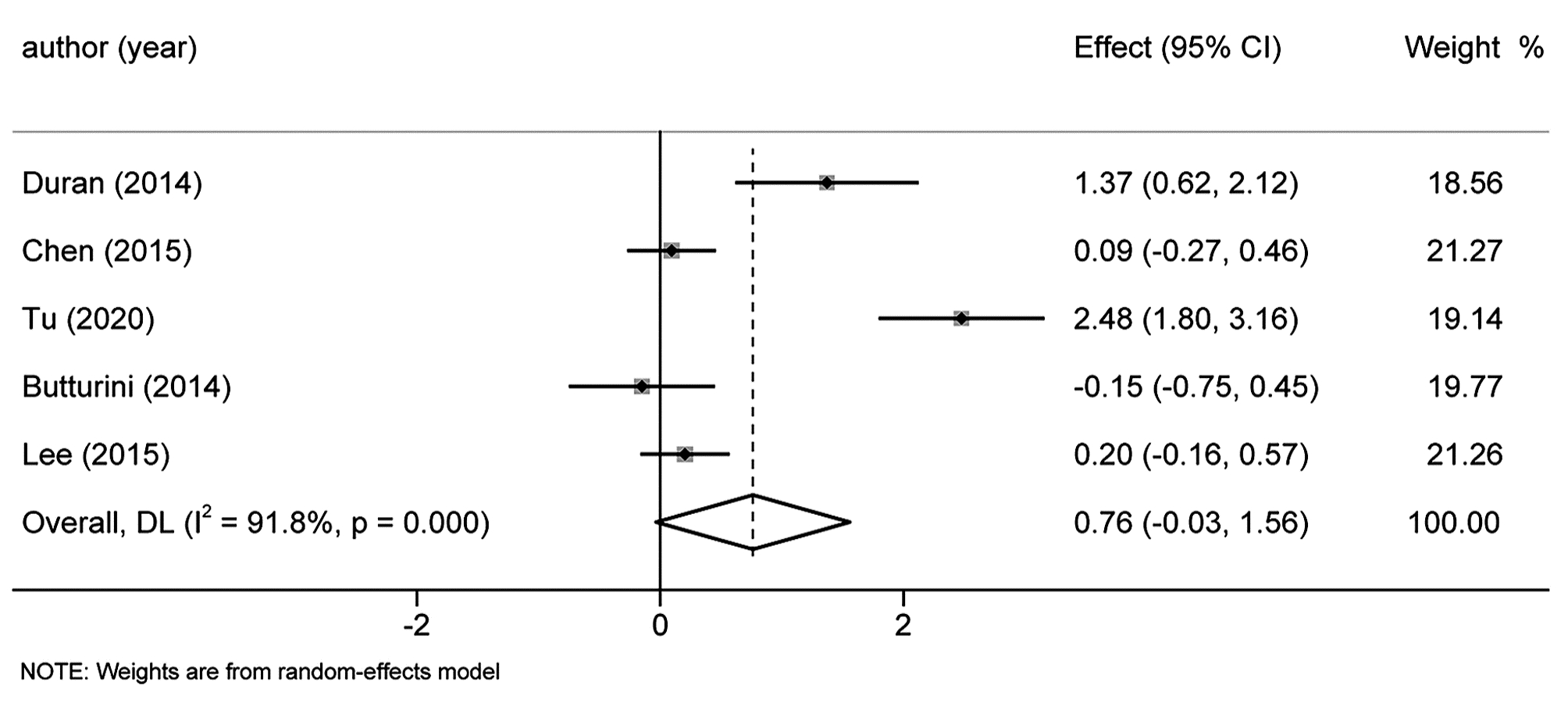
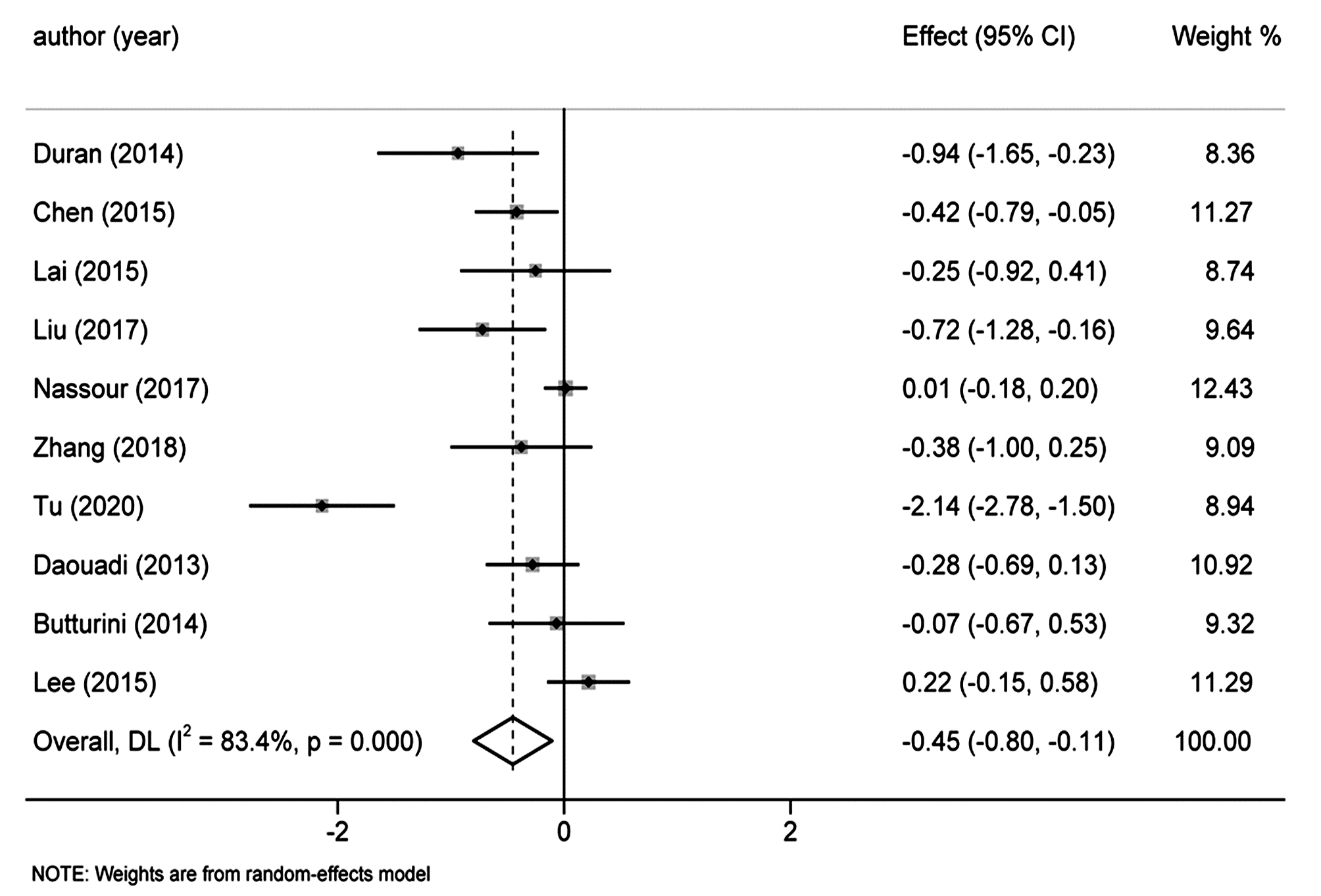
DURAN H, IELPO B, CARUSO R, et al. Does robotic distal pancreatectomy surgery offer similar results as laparoscopic and open approach? A comparative study from a single medical center[J]. Int J Med Robot, 2014, 10(3): 280-285. DOI: 10.1002/rcs.1569. |
| [5] |
CHEN S, ZHAN Q, CHEN JZ, et al. Robotic approach improves spleen-preserving rate and shortens postoperative hospital stay of laparosc opic distal pancreatectomy: A matched cohort study[J]. Surg Endosc, 2015, 29(12): 3507-3518. DOI: 10.1007/s00464-015-4101-5. |
| [6] |
LAI EC, TANG CN. Robotic distal pancreatectomy versus conventional laparoscopic distal pancreatectomy: A comparative study for short-term outcomes[J]. Front Med, 2015, 9(3): 356-360. DOI: 10.1007/s11684-015-0404-0. |
| [7] |
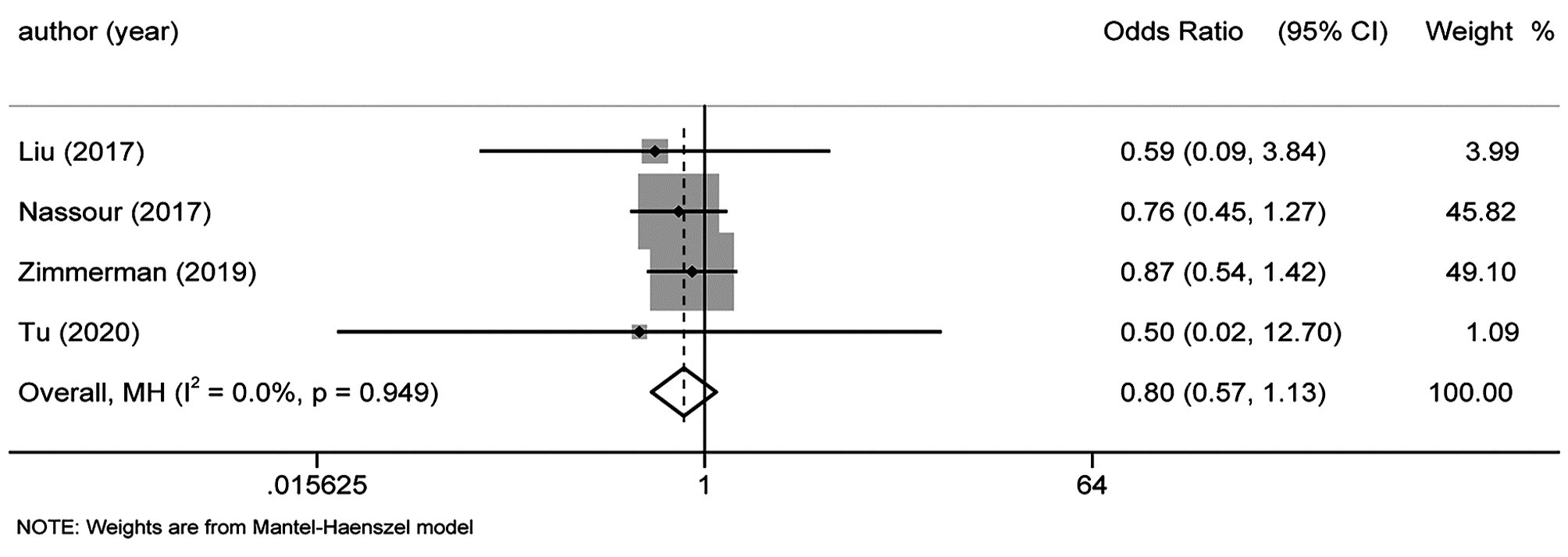
LIU R, ZHANG T, ZHAO ZM, et al. The surgical outcomes of robot-assisted laparoscopic pancreaticoduodenectomy versus laparoscopic pancreaticoduodenectomy for periampullary neoplasms: A comparative study of a single center[J]. Surg Endosc, 2017, 31(6): 2380-2386. DOI: 10.1007/s00464-016-5238-6. |
| [8] |
NASSOUR I, WANG SC, POREMBKA MR, et al. Robotic versus laparoscopic pancreaticoduodenectomy: A nsqip analysis[J]. J Gastrointest Surg, 2017, 21(11): 1784-1792. DOI: 10.1007/s11605-017-3543-6. |
| [9] |
ZHANG Y, HONG D, ZHANG C, et al. Total laparoscopic versus robot-assisted laparoscopic pancreaticoduodenectomy[J]. Biosci Trends, 2018, 12(5): 484-490. DOI: 10.5582/bst.2018.01236. |
| [10] |
ZIMMERMAN AM, ROYE DG, CHARPENTIER KP. A comparison of outcomes between open, laparoscopic and robotic pancreaticoduodenectomy[J]. HPB (Oxford), 2018, 20(4): 364-369. DOI: 10.1016/j.hpb.2017.10.008. |
| [11] |
TU GP, SUN JC, NIE WP, et al. Comparison of efficacy and safety of robotic-assisted versus laparoscopic pancreaticoduodenectomy for pancreatic cancer[J]. Chin J Gen Surg, 2020, 3(29): 269-275. DOI: 10.7659/j.issn.1005-6947.2020.03.003. |
| [12] |
BUTTURINI G, DAMOLI I, CREPAZ L, et al. A prospective non-randomised single-center study comparing laparoscopic and robotic distal pancreatec tomy[J]. Surg Endosc, 2015, 29(11): 3163-3170. DOI: 10.1007/s00464-014-4043-3. |
| [13] |
LEE SY, ALLEN PJ, SADOT E, et al. Distal pancreatectomy: A single institution's experience in open, laparoscopic, and robotic approaches[J]. J Am Coll Surg, 2015, 220(1): 18-27. DOI: 10.1016/j.jamcollsurg.2014.10.004. |
| [14] |
DAOUADI M, ZUREIKAT AH, ZENATI MS, et al. Robot-assisted minimally invasive distal pancreatectomy is superior to the laparoscopic technique[J]. Ann Surg, 2013, 257(1): 128-132. DOI: 10.1097/SLA.0b013e31825fff08. |
| [15] |
WATERS JA, CANAL DF, WIEBKE EA, et al. Robotic distal pancreatectomy: Cost effective?[J]. Surgery, 2010, 148(4): 814-823. DOI: 10.1016/j.surg.2010.07.027. |
| [16] |
ZHANG C, AN L, WANG Y, et al, Impact of different operative approaches for laparoscopic pancreaticoduodenectomy on short-term treatment outcomes[J]. Chin J Hepatobiliary Surg, 2020, 4(26): 286-289. DOI: 10.3760/cma.j.cn113884-20190926-00318. |
| [17] |
ALIP S, KOUKOURIKIS P, HAN WK, et al. Comparing revo-i and da vinci in retzius-sparing robot-assisted radical prostatectomy: A preliminary propensity score analysis of outcomes[J]. J Endourol, 2022, 36(1): 104-110. DOI: 10.1089/end.2021.0421. |
| [18] |
WU CJ, CHEN HH, CHENG PW, et al. Outcome of robot-assisted bilateral internal mammary artery grafting via left pleura in coronary bypa ss surgery[J]. J Clin Med, 2019, 8(4): 502. DOI: 10.3390/jcm8040502. |
| [19] |
GAVRIILIDIS P, LIM C, MENAHEM B, et al. Robotic versus laparoscopic distal pancreatectomy-the first meta-analysis[J]. HPB (Oxford), 2016, 18(7): 567-574. DOI: 10.1016/j.hpb.2016.04.008. |







 DownLoad:
DownLoad: