| [1] |
PU LZ, SINGH R, LOONG CK, et al. Malignant biliary obstruction: Evidence for best practice[J]. Gastroenterol Res Pract, 2016, 2016: 3296801. DOI: 10.1155/2016/3296801. |
| [2] |
CHEN WW, HUANG K, LIU R, et al. Clinical effect of percutaneous transhepatic cholangial drainage combined with biliary stent implantation in treatment of high malignant obstructive jaundice and the influencing factors for prognosis[J]. J Clin Hepatol, 2019, 35(3): 559-564. DOI: 10.3969/j.issn.1001-5256.2019.03.021. |
| [3] |
BERGQUIST A, VON SETH E. Epidemiology of cholangiocarcinoma[J]. Best Pract Res Clin Gastroenterol, 2015, 29(2): 221-232. DOI: 10.1016/j.bpg.2015.02.003. |
| [4] |
YOSHIDA Y, AJIKI T, UENO K, et al. Preoperative bile replacement improves immune function for jaundiced patients treated with external biliary drainage[J]. J Gastrointest Surg, 2014, 18(12): 2095-2104. DOI: 10.1007/s11605-014-2674-2. |
| [5] |
GUNDRY SR, STRODEL WE, KNOL JA, et al. Efficacy of preoperative biliary tract decompression in patients with obstructive jaundice[J]. Arch Surg, 1984, 119(6): 703-708. DOI: 10.1001/archsurg.1984.01390180065011. |
| [6] |
COATES JM, BEAL SH, RUSSO JE, et al. Negligible effect of selective preoperative biliary drainage on perioperative resuscitation, morbidity, and mortality in patients undergoing pancreaticoduodenectomy[J]. Arch Surg, 2009, 144(9): 841-847. DOI: 10.1001/archsurg.2009.152. |
| [7] |
ZHAO SW, SHEN ZY, WANG JC, et al. Effect of biliary drainage methods on patients with obstructive jaundice undergoing pancreaticoduodenectomy[J]. J Surg Concepts Pract, 2020, 25(4): 301-305. DOI: 10.16139/j.1007-9610.2020.04.007. |
| [8] |
CHOI SH, GWON DI, KO GY, et al. Hepatic arterial injuries in 3110 patients following percutaneous transhepatic biliary drainage[J]. Radiology, 2011, 261(3): 969-975. DOI: 10.1148/radiol.11110254. |
| [9] |
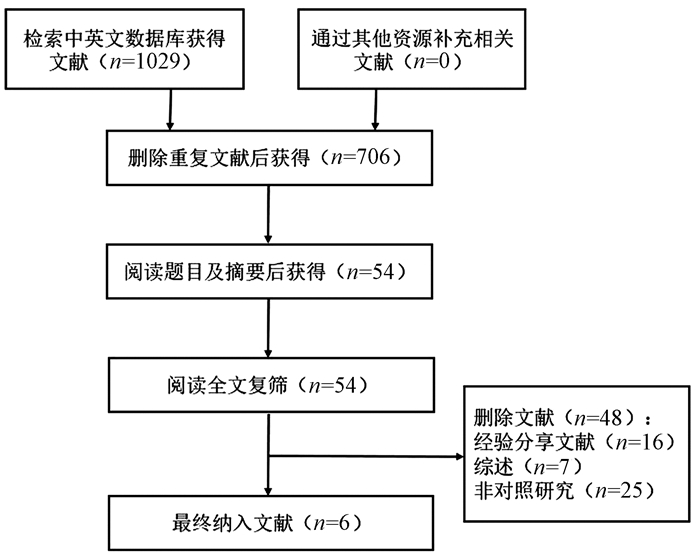
MOHER D, LIBERATI A, TETZLAFF J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement[J]. PLoS Med, 2009, 6(7): e1000097. DOI: 10.1371/journal.pmed.1000097. |
| [10] |
LUCHINI C, STUBBS B, SOLMI M, et al. Assessing the quality of studies in Meta-analyses: Advantages and limitations of the Newcastle Ottawa Scale[J]. World J Meta-Analysis, 2017, 5(4): 80-84. DOI: 10.13105/wjma.v5.i4.80. |
| [11] |
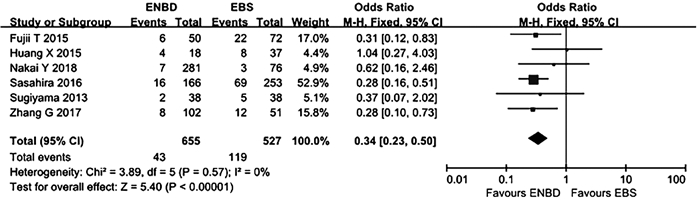
FUJII T, YAMADA S, SUENAGA M, et al. Preoperative internal biliary drainage increases the risk of bile juice infection and pancreatic fistula after pancreatoduodenectomy: A prospective observational study[J]. Pancreas, 2015, 44(3): 465-470. DOI: 10.1097/MPA.0000000000000265. |
| [12] |
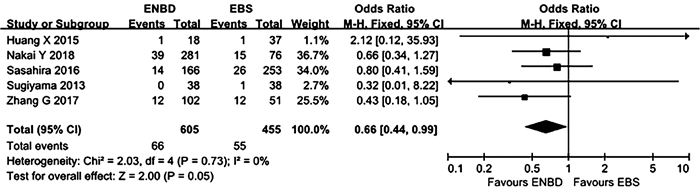
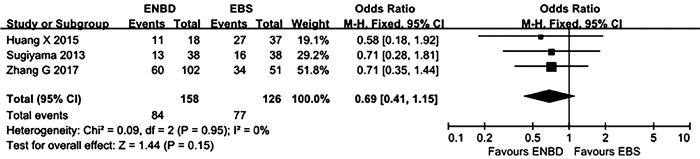
HUANG X, LIANG B, ZHAO XQ, et al. The effects of different preoperative biliary drainage methods on complications following pancreaticoduodenectomy[J]. Medicine (Baltimore), 2015, 94(14): e723. DOI: 10.1097/MD.0000000000000723. |
| [13] |
NAKAI Y, YAMAMOTO R, MATSUYAMA M, et al. Multicenter study of endoscopic preoperative biliary drainage for malignant hilar biliary obstruction: E-POD hilar study[J]. J Gastroenterol Hepatol, 2018, 33(5): 1146-1153. DOI: 10.1111/jgh.14050. |
| [14] |
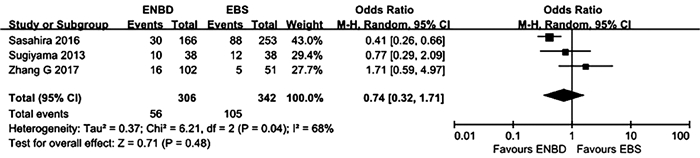
SASAHIRA N, HAMADA T, TOGAWA O, et al. Multicenter study of endoscopic preoperative biliary drainage for malignant distal biliary obstruction[J]. World J Gastroenterol, 2016, 22(14): 3793-3802. DOI: 10.3748/wjg.v22.i14.3793. |
| [15] |
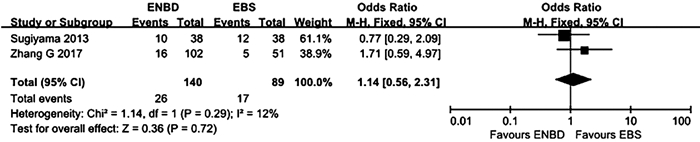
SUGIYAMA H, TSUYUGUCHI T, SAKAI Y, et al. Preoperative drainage for distal biliary obstruction: Endoscopic stenting or nasobiliary drainage?[J]. Hepatogastroenterology, 2013, 60(122): 231-234. DOI: 10.5754/hge12621. |
| [16] |
ZHANG GQ, LI Y, REN YP, et al. Outcomes of preoperative endoscopic nasobiliary drainage and endoscopic retrograde biliary drainage for malignant distal biliary obstruction prior to pancreaticoduodenectomy[J]. World J Gastroenterol, 2017, 23(29): 5386-5394. DOI: 10.3748/wjg.v23.i29.5386. |
| [17] |
van der GAAG NA, RAUWS EA, van EIJCK CH, et al. Preoperative biliary drainage for cancer of the head of the pancreas[J]. N Engl J Med, 2010, 362(2): 129-137. DOI: 10.1056/NEJMoa0903230. |
| [18] |
SEWNATH ME, KARSTEN TM, PRINS MH, et al. A meta-analysis on the efficacy of preoperative biliary drainage for tumors causing obstructive jaundice[J]. Ann Surg, 2002, 236(1): 17-27. DOI: 10.1097/00000658-200207000-00005. |
| [19] |
KARNABATIDIS D, SPILIOPOULOS S, KATSAKIORI P, et al. Percutaneous trans-hepatic bilateral biliary stenting in Bismuth Ⅳ malignant obstruction[J]. World J Hepatol, 2013, 5(3): 114-119. DOI: 10.4254/wjh.v5.i3.114. |
| [20] |
BARKAY O, MOSLER P, SCHMITT CM, et al. Effect of endoscopic stenting of malignant bile duct obstruction on quality of life[J]. J Clin Gastroenterol, 2013, 47(6): 526-531. DOI: 10.1097/MCG.0b013e318272440e. |
| [21] |
YAGIOKA H, HIRANO K, ISAYAMA H, et al. Clinical significance of bile cytology via an endoscopic nasobiliary drainage tube for pathological diagnosis of malignant biliary strictures[J]. J Hepatobiliary Pancreat Sci, 2011, 18(2): 211-215. DOI: 10.1007/s00534-010-0333-x. |
| [22] |
HONG SK, JANG JY, KANG MJ, et al. Comparison of clinical outcome and cost-effectiveness after various preoperative biliary drainage methods in periampullary cancer with obstructive jaundice[J]. J Korean Med Sci, 2012, 27(4): 356-362. DOI: 10.3346/jkms.2012.27.4.356. |
| [23] |
CORTES A, SAUVANET A, BERT F, et al. Effect of bile contamination on immediate outcomes after pancreaticoduodenectomy for tumor[J]. J Am Coll Surg, 2006, 202(1): 93-99. DOI: 10.1016/j.jamcollsurg.2005.09.006. |
| [24] |
YU PH, SU S, CHEN S, et al. Clinical effect of pancreaticoduodenectomy with total mesopancreas excision versus traditional pancreaticoduodenecto-my in treatment of pancreatic head carcinoma and periampullary cancer: A meta-analysis[J]. J Clin Hepatol, 2020, 36(8): 1811-1815. DOI: 10.3969/j.issn.1001-5256.2020.08.026. |
| [25] |
VELANOVICH V, KHEIBEK T, KHAN M. Relationship of postoperative complications from preoperative biliary stents after pancreaticoduodenectomy. A new cohort analysis and meta-analysis of modern studies[J]. JOP, 2009, 10(1): 24-29. http://www.ncbi.nlm.nih.gov/pubmed/19129611 |
| [26] |
KAWAI M, TANI M, HIRONO S, et al. Association of preoperative biliary drainage related complications with postoperative complications after pancreaticoduodenectomy[J]. HPB, 2014, 16: 111-112.
|







 DownLoad:
DownLoad: