| [1] |
ELMUNZER BJ, MARANKI JL, GÓMEZ V, et al. ACG clinical guideline: Diagnosis and management of biliary strictures[J]. Am J Gastroenterol, 2023, 118( 3): 405- 426. DOI: 10.14309/ajg.0000000000002190. |
| [2] |
BANALES JM, MARIN JJG, LAMARCA A, et al. Cholangiocarcinoma 2020: The next horizon in mechanisms and management[J]. Nat Rev Gastroenterol Hepatol, 2020, 17( 9): 557- 588. DOI: 10.1038/s41575-020-0310-z. |
| [3] |
WANG JJ, XIA MX, JIN YB, et al. More endoscopy-based brushing passes improve the detection of malignant biliary strictures: A multicenter randomized controlled trial[J]. Am J Gastroenterol, 2022, 117( 5): 733- 739. DOI: 10.14309/ajg.0000000000001666. |
| [4] |
WANG GX, GE XD, ZHANG D, et al. MRCP combined with CT promotes the differentiation of benign and malignant distal bile duct strictures[J]. Front Oncol, 2021, 11: 683869. DOI: 10.3389/fonc.2021.683869. |
| [5] |
ZHANG YZ, JIANG QW, WANG Q, et al. Predicting malignancy of biliary stricture with a nomogram in patients with a non-malignant endoscopic tissue diagnosis: A retrospective study[J]. Cancer Manag Res, 2021, 13: 7735- 7745. DOI: 10.2147/CMAR.S333333. |
| [6] |
XING HB, WANG J, WANG YL, et al. Diagnostic value of CA 19-9 and carcinoembryonic antigen for pancreatic cancer: A meta-analysis[J]. Gastroenterol Res Pract, 2018, 2018: 8704751. DOI: 10.1155/2018/8704751. |
| [7] |
XIE CC, ALOREIDI K, PATEL B, et al. Indeterminate biliary strictures: A simplified approach[J]. Expert Rev Gastroenterol Hepatol, 2018, 12( 2): 189- 199. DOI: 10.1080/17474124.2018.1391090. |
| [8] |
BOYD LNC, ALI M, KAM L, et al. The diagnostic value of the CA19-9 and bilirubin ratio in patients with pancreatic cancer, distal bile duct cancer and benign periampullary diseases, a novel approach[J]. Cancers, 2022, 14( 2): 344. DOI: 10.3390/cancers14020344. |
| [9] |
MUTTILLO EM, CIARDI A, TROIANO R, et al. Pancreatic ductal adenocarcinoma and distal cholangiocarcinoma: A proposal of preoperative diagnostic score for differential diagnosis[J]. World J Surg Oncol, 2021, 19( 1): 10. DOI: 10.1186/s12957-021-02120-w. |
| [10] |
DRAZILOVA S, VESELINY E, LENARTOVA PD, et al. IgG4-related sclerosing cholangitis: Rarely diagnosed, but not a rare disease[J]. Can J Gastroenterol Hepatol, 2021, 2021: 1959832. DOI: 10.1155/2021/1959832. |
| [11] |
MADHUSUDHAN KS, DAS P, GUNJAN D, et al. IgG4-related sclerosing cholangitis: A clinical and imaging review[J]. AJR Am J Roentgenol, 2019, 213( 6): 1221- 1231. DOI: 10.2214/AJR.19.21519. |
| [12] |
VOIGTLÄNDER T, METZGER J, HUSI H, et al. Bile and urine peptide marker profiles: Access keys to molecular pathways and biological processes in cholangiocarcinoma[J]. J Biomed Sci, 2020, 27( 1): 13. DOI: 10.1186/s12929-019-0599-5. |
| [13] |
MACIAS RIR, MUÑOZ-BELLVÍS L, SÁNCHEZ-MARTÍN A, et al. A novel serum metabolomic profile for the differential diagnosis of distal cholangiocarcinoma and pancreatic ductal adenocarcinoma[J]. Cancers, 2020, 12( 6): 1433. DOI: 10.3390/cancers12061433. |
| [14] |
LE LARGE TYS, MEIJER LL, PALECKYTE R, et al. Combined expression of plasma thrombospondin-2 and CA19-9 for diagnosis of pancreatic cancer and distal cholangiocarcinoma: A proteome approach[J]. Oncologist, 2020, 25( 4): e634- e643. DOI: 10.1634/theoncologist.2019-0680. |
| [15] |
LEE DH, KIM B, LEE ES, et al. Radiologic evaluation and structured reporting form for extrahepatic bile duct cancer: 2019 consensus recommendations from the Korean society of abdominal radiology[J]. Korean J Radiol, 2021, 22( 1): 41- 62. DOI: 10.3348/kjr.2019.0803. |
| [16] |
SHABANIKIA N, ADIBI A, EBRAHIMIAN S. Diagnostic accuracy of magnetic resonance cholangiopancreatography to detect benign and malignant biliary strictures[J]. Adv Biomed Res, 2021, 10: 38. DOI: 10.4103/abr.abr_137_20. |
| [17] |
ZHU Y, JIN HL, MAO YF, et al. Unexplained distal obstructive biliary dilatation: A magnetic resonance cholangiopancreatography(MRCP)-based model to discriminate malignant from benign origins[J]. J Clin Gastroenterol, 2022, 56( 8): 724- 730. DOI: 10.1097/MCG.0000000000001614. |
| [18] |
NAVANEETHAN U, NJEI B, LOURDUSAMY V, et al. Comparative effectiveness of biliary brush cytology and intraductal biopsy for detection of malignant biliary strictures: A systematic review and meta-analysis[J]. Gastrointest Endosc, 2015, 81( 1): 168- 176. DOI: 10.1016/j.gie.2014.09.017. |
| [19] |
KOBAYASHI M, RYOZAWA S, ARAKI R, et al. Investigation of factors affecting the sensitivity of bile duct brush cytology[J]. Intern Med, 2019, 58( 3): 329- 335. DOI: 10.2169/internalmedicine.1551-18. |
| [20] |
ROTH GS, BICHARD P, FIOR-GOZLAN M, et al. Performance of bile aspiration plus brushing to diagnose malignant biliary strictures during endoscopic retrograde cholangiopancreatography[J]. Endosc Int Open, 2016, 4( 9): E997- E1003. DOI: 10.1055/s-0042-108854. |
| [21] |
KATO A, KATO H, NAITOH I, et al. Use of endoscopic scraper and cell block technique as a replacement for conventional brush for diagnosing malignant biliary strictures[J]. Cancers, 2022, 14( 17): 4147. DOI: 10.3390/cancers14174147. |
| [22] |
GONDA TA, VITERBO D, GAUSMAN V, et al. Mutation profile and fluorescence in situ hybridization analyses increase detection of malignancies in biliary strictures[J]. Clin Gastroenterol Hepatol, 2017, 15( 6): 913- 919. e 1. DOI: 10.1016/j.cgh.2016.12.013. |
| [23] |
SINGHI AD, NIKIFOROVA MN, CHENNAT J, et al. Integrating next-generation sequencing to endoscopic retrograde cholangiopancreatography(ERCP)-obtained biliary specimens improves the detection and management of patients with malignant bile duct strictures[J]. Gut, 2020, 69( 1): 52- 61. DOI: 10.1136/gutjnl-2018-317817. |
| [24] |
JANG SI, KWON NH, LIM BJ, et al. New staining method using methionyl-tRNA synthetase 1 antibody for brushing cytology of bile duct cancer[J]. Gastrointest Endosc, 2020, 92( 2): 310- 319. e 6. DOI: 10.1016/j.gie.2019.12.017. |
| [25] |
JANG SI, NAHM JH, KWON NH, et al. Clinical utility of methionyl-tRNA synthetase 1 immunostaining in cytologic brushings of indeterminate biliary strictures: A multicenter prospective study[J]. Gastrointest Endosc, 2021, 94( 4): 733- 741. e 4. DOI: 10.1016/j.gie.2021.04.026. |
| [26] |
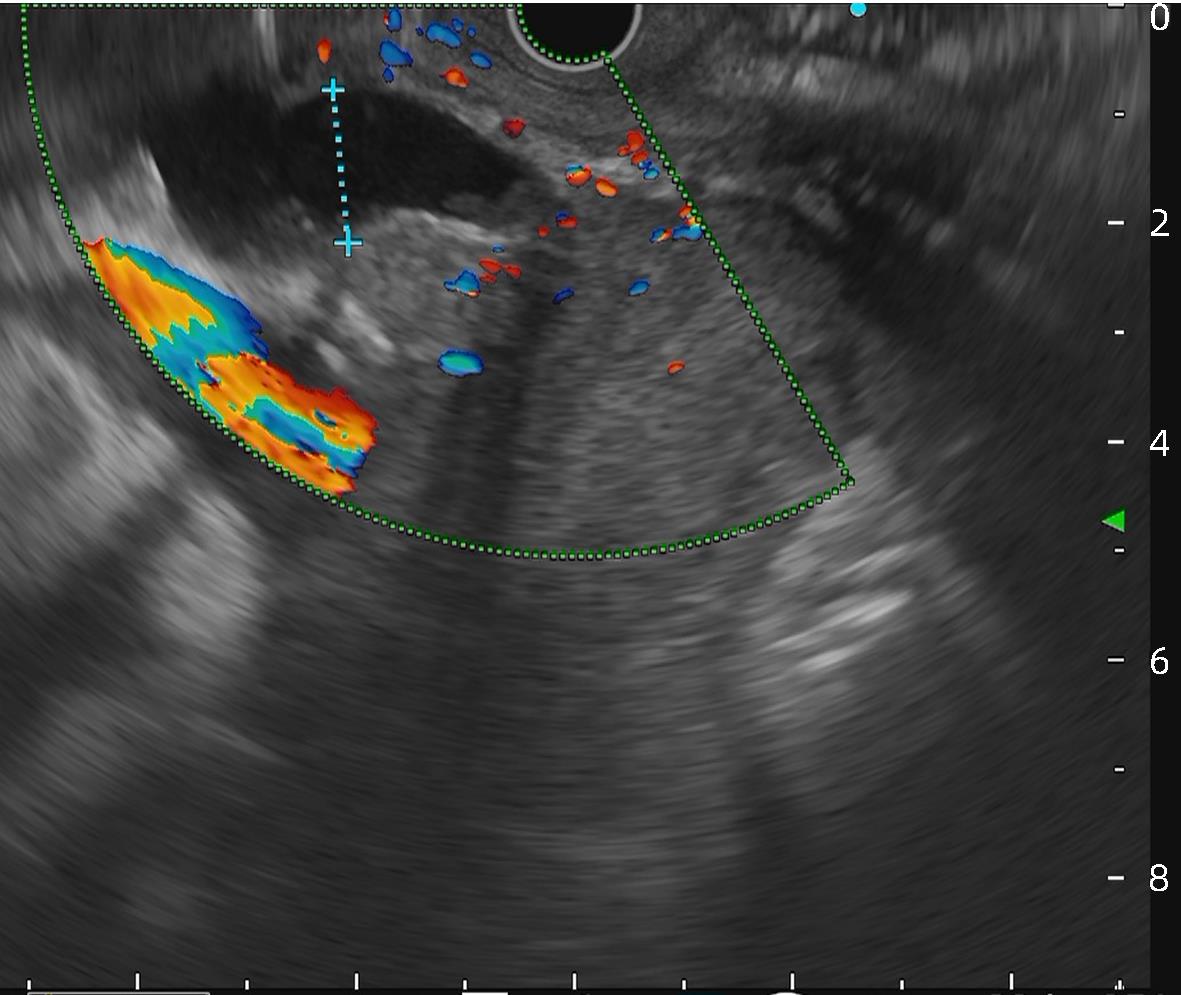
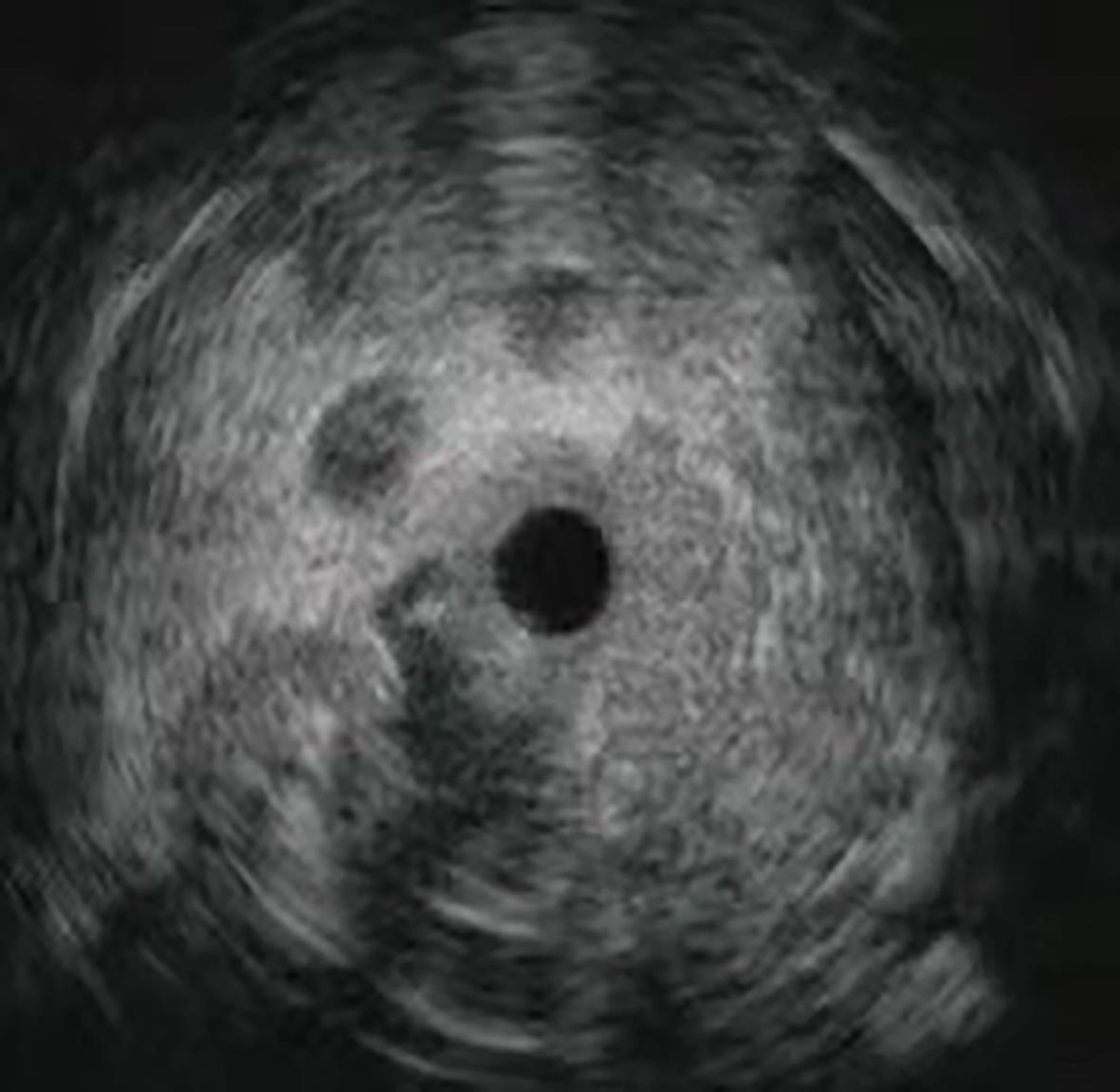
MEISTER T, HEINZOW HS, WOESTMEYER C, et al. Intraductal ultrasound substantiates diagnostics of bile duct strictures of uncertain etiology[J]. World J Gastroenterol, 2013, 19( 6): 874- 881. DOI: 10.3748/wjg.v19.i6.874. |
| [27] |
SEIFERT H, FUSAROLI P, ARCIDIACONO PG, et al. Controversies in EUS: Do we need miniprobes?[J]. Endosc Ultrasound, 2021, 10( 4): 246- 269. DOI: 10.4103/EUS-D-20-00252. |
| [28] |
KIM HS, MOON JH, LEE YN, et al. Prospective comparison of intraductal ultrasonography-guided transpapillary biopsy and conventional biopsy on fluoroscopy in suspected malignant biliary strictures[J]. Gut Liver, 2018, 12( 4): 463- 470. DOI: 10.5009/gnl17205. |
| [29] |
LEE JH, SALEM R, ASLANIAN H, et al. Endoscopic ultrasound and fine-needle aspiration of unexplained bile duct strictures[J]. Am J Gastroenterol, 2004, 99( 6): 1069- 1073. DOI: 10.1111/j.1572-0241.2004.30223.x. |
| [30] |
PAUSAWASDI N, HONGSRISUWAN P, KAMANI L, et al. Diagnostic value of endoscopic ultrasonography for common bile duct dilatation without identifiable etiology detected from cross-sectional imaging[J]. Clin Endosc, 2022, 55( 1): 122- 127. DOI: 10.5946/ce.2021.122. |
| [31] |
MALIKOWSKI T, LEVY MJ, GLEESON FC, et al. Endoscopic ultrasound/fine needle aspiration is effective for lymph node staging in patients with cholangiocarcinoma[J]. Hepatology, 2020, 72( 3): 940- 948. DOI: 10.1002/hep.31077. |
| [32] |
MOURA DTH, de MOURA EGH, MATUGUMA SE, et al. EUS-FNA versus ERCP for tissue diagnosis of suspect malignant biliary strictures: A prospective comparative study[J]. Endosc Int Open, 2018, 6( 6): E769- E777. DOI: 10.1055/s-0043-123186. |
| [33] |
JO JH, CHO CM, JUN JH, et al. Same-session endoscopic ultrasound-guided fine needle aspiration and endoscopic retrograde cholangiopancreatography-based tissue sampling in suspected malignant biliary obstruction: A multicenter experience[J]. J Gastroenterol Hepatol, 2019, 34( 4): 799- 805. DOI: 10.1111/jgh.14528. |
| [34] |
CHIANG A, THERIAULT M, SALIM M, et al. The incremental benefit of EUS for the identification of malignancy in indeterminate extrahepatic biliary strictures: A systematic review and meta-analysis[J]. Endosc Ultrasound, 2019, 8( 5): 310- 317. DOI: 10.4103/eus.eus_24_19. |
| [35] |
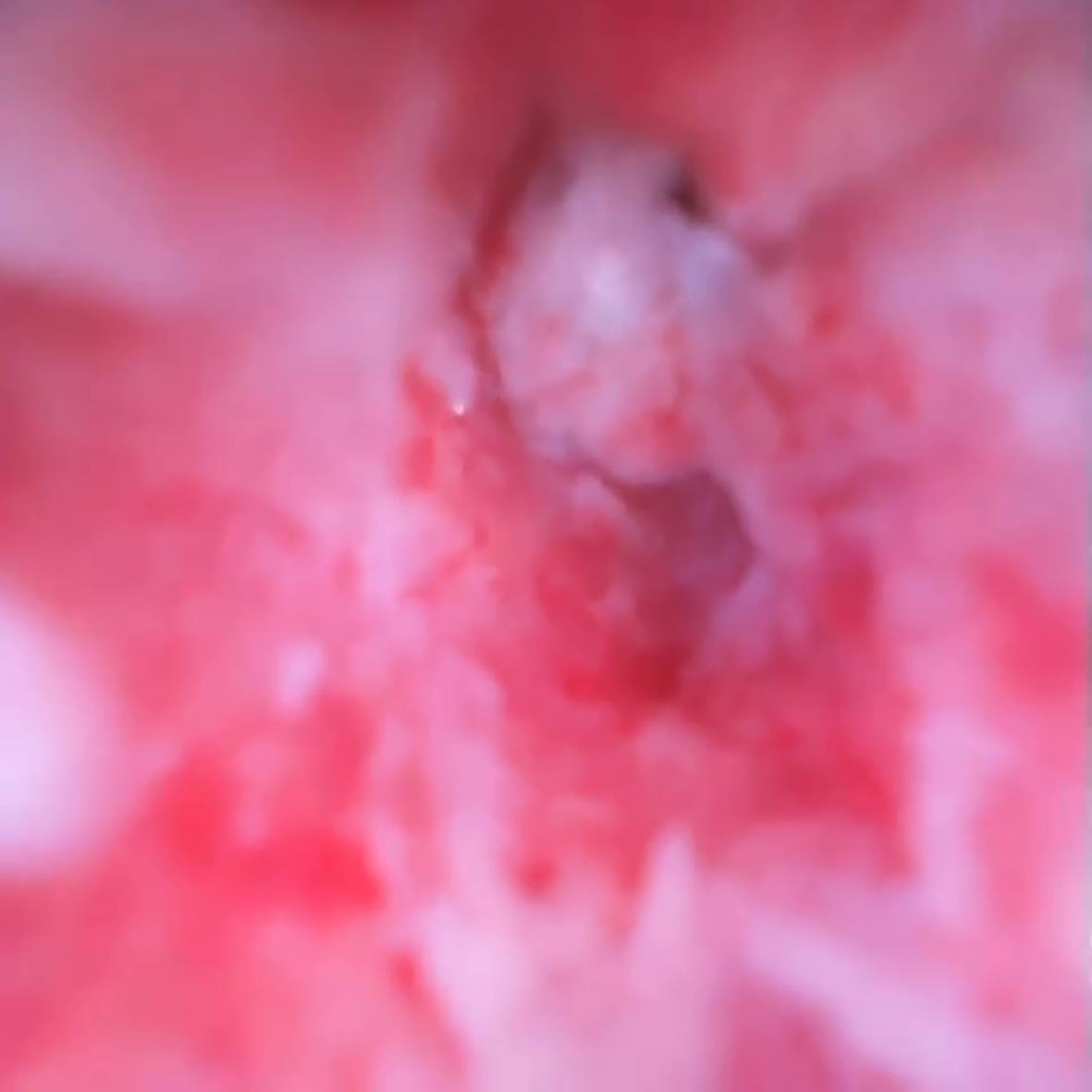
KULPATCHARAPONG S, PITTAYANON R, KERR SJ, et al. Diagnostic performance of digital and video cholangioscopes in patients with suspected malignant biliary strictures: A systematic review and meta-analysis[J]. Surg Endosc, 2022, 36( 5): 2827- 2841. DOI: 10.1007/s00464-021-08571-2. |
| [36] |
JANG S, STEVENS T, KOU L, et al. Efficacy of digital single-operator cholangioscopy and factors affecting its accuracy in the evaluation of indeterminate biliary stricture[J]. Gastrointest Endosc, 2020, 91( 2): 385- 393. e 1. DOI: 10.1016/j.gie.2019.09.015. |
| [37] |
LEE YN, MOON JH, CHOI HJ, et al. Tissue acquisition for diagnosis of biliary strictures using peroral cholangioscopy or endoscopic ultrasound-guided fine-needle aspiration[J]. Endoscopy, 2019, 51( 1): 50- 59. DOI: 10.1055/a-0645-1395. |
| [38] |
CHEN PT, CHANG DW, WU TH, et al. Applications of artificial intelligence in pancreatic and biliary diseases[J]. J Gastroenterol Hepatol, 2021, 36( 2): 286- 294. DOI: 10.1111/jgh.15380. |
| [39] |
YAO X, HUANG X, YANG C, et al. A novel approach to assessing differentiation degree and lymph node metastasis of extrahepatic cholangiocarcinoma: Prediction using a radiomics-based particle swarm optimization and support vector machine model[J]. JMIR Med Inform, 2020, 8( 10): e23578. DOI: 10.2196/23578. |
| [40] |
PENG YT, ZHOU CY, LIN P, et al. Preoperative ultrasound radiomics signatures for noninvasive evaluation of biological characteristics of intrahepatic cholangiocarcinoma[J]. Acad Radiol, 2020, 27( 6): 785- 797. DOI: 10.1016/j.acra.2019.07.029. |
| [41] |
QIAN XL, ZHOU CW, WANG F, et al. Development and validation of combined Ki67 status prediction model for intrahepatic cholangiocarcinoma based on clinicoradiological features and MRI radiomics[J]. Radiol Med, 2023, 128( 3): 274- 288. DOI: 10.1007/s11547-023-01597-7. |
| [42] |
ZHANG X, TANG DH, ZHOU JD, et al. A real-time interpretable artificial intelligence model for the cholangioscopic diagnosis of malignant biliary stricture(with videos)[J]. Gastrointest Endosc, 2023, 98( 2): 199- 210. e 10. DOI: 10.1016/j.gie.2023.02.026. |
| [43] |
SETHI A, TYBERG A, SLIVKA A, et al. Digital single-operator cholangioscopy(DSOC) improves interobserver agreement(IOA) and accuracy for evaluation of indeterminate biliary strictures: The Monaco classification[J]. J Clin Gastroenterol, 2022, 56( 2): e94- e97. DOI: 10.1097/MCG.0000000000001321. |
| [44] |
AHMAD OF, STASSEN P, WEBSTER GJ. Artificial intelligence in biliopancreatic endoscopy: Is there any role?[J]. Best Pract Res Clin Gastroenterol, 2021, 52-53: 101724. DOI: 10.1016/j.bpg.2020.101724. |
| [45] |
RIBEIRO T, SARAIVA MM, AFONSO J, et al. Automatic identification of papillary projections in indeterminate biliary strictures using digital single-operator cholangioscopy[J]. Clin Transl Gastroenterol, 2021, 12( 11): e00418. DOI: 10.14309/ctg.0000000000000418. |
| [46] |
PEREIRA P, MASCARENHAS M, RIBEIRO T, et al. Automatic detection of tumor vessels in indeterminate biliary strictures in digital single-operator cholangioscopy[J]. Endosc Int Open, 2022, 10( 3): E262- E268. DOI: 10.1055/a-1723-3369. |







 DownLoad:
DownLoad: