| [1] |
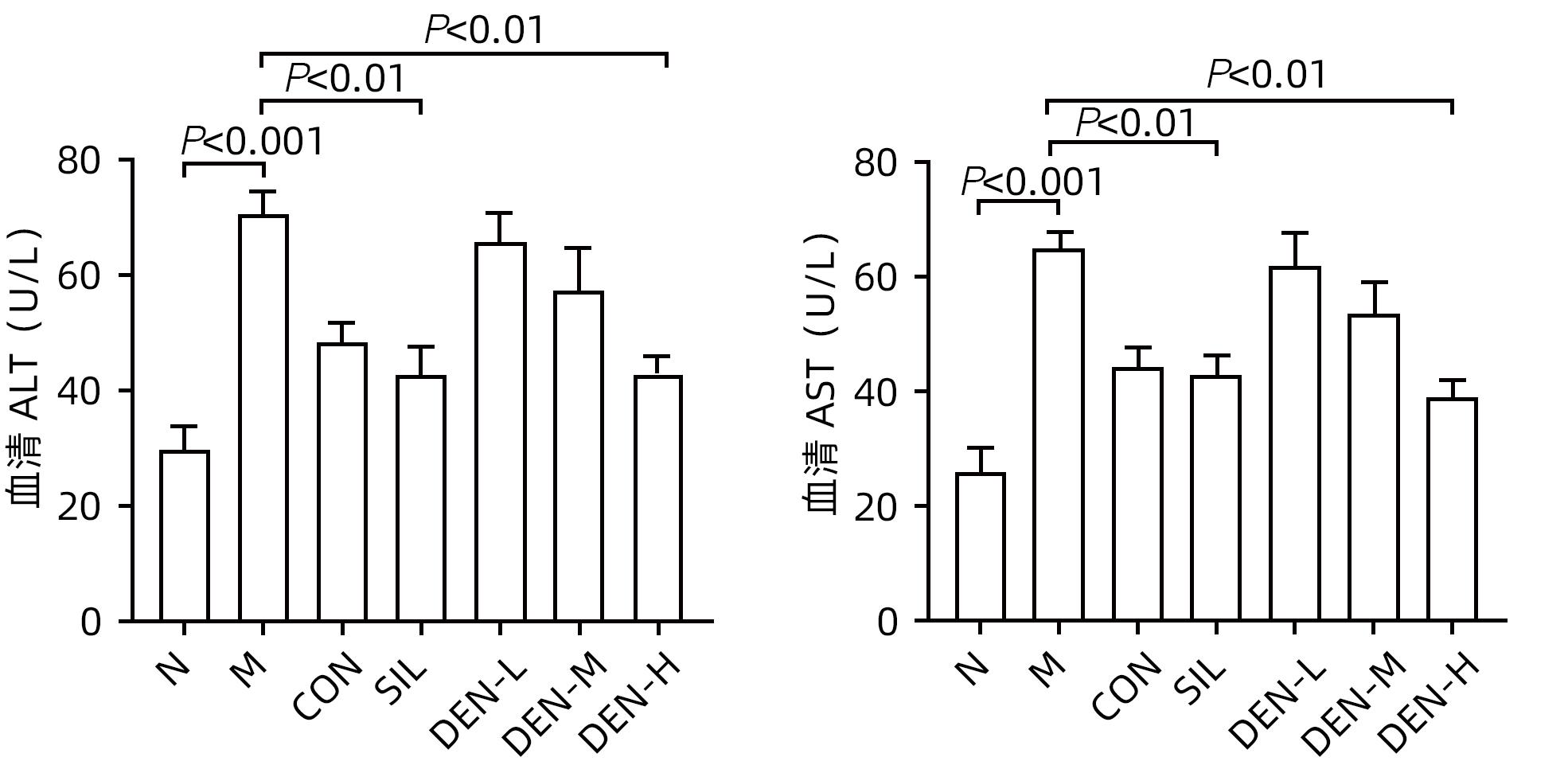
ALTAMIRANO J, BATALLER R. Alcoholic liver disease: Pathogenesis and new targets for therapy[J]. Nat Rev Gastroenterol Hepatol, 2011, 8( 9): 491- 501. DOI: 10.1038/nrgastro.2011.134. |
| [2] |
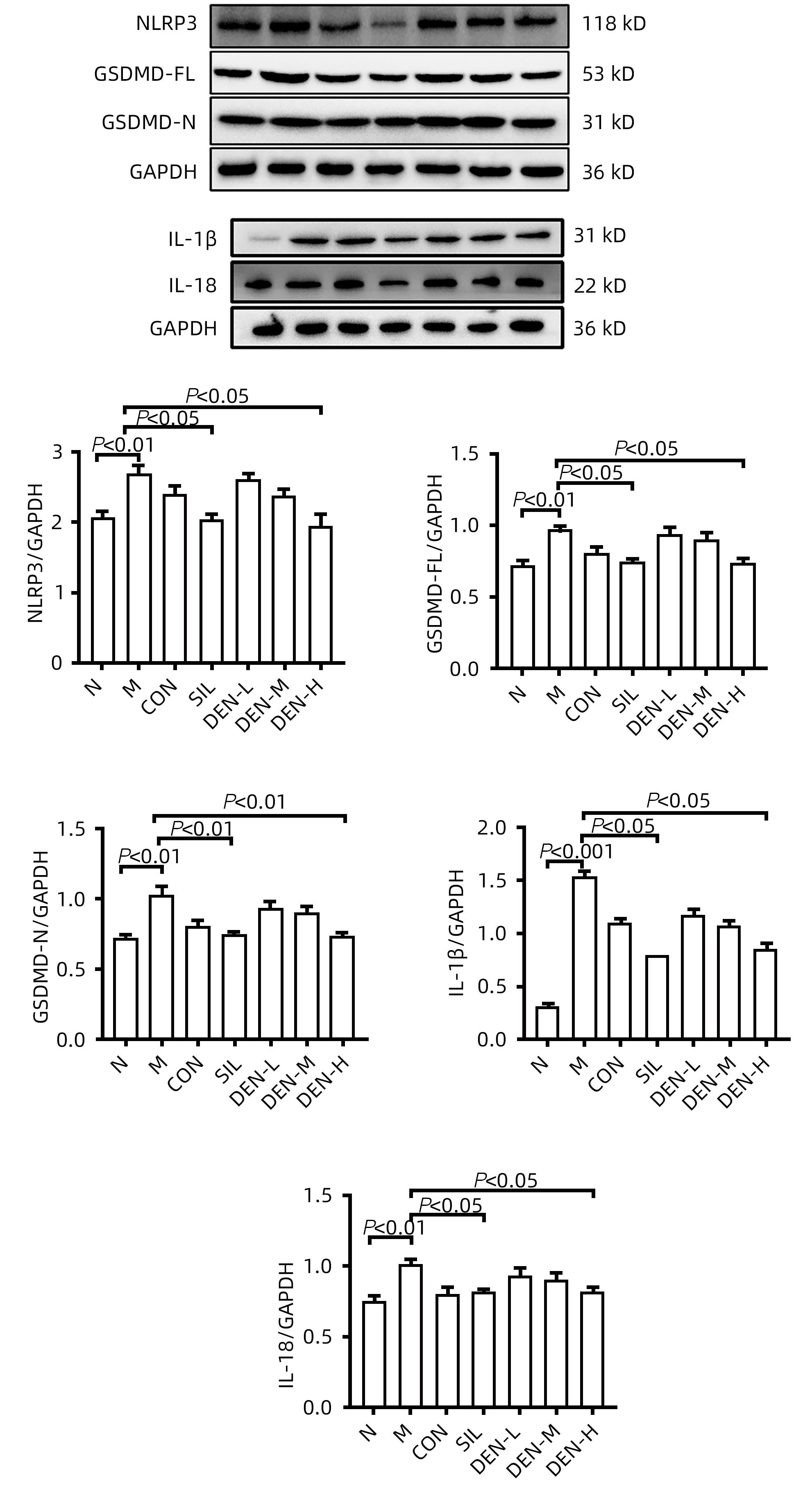
SHI JJ, ZHAO Y, WANG K, et al. Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death[J]. Nature, 2015, 526( 7575): 660- 665. DOI: 10.1038/nature15514. |
| [3] |
LIU X, XIA SY, ZHANG ZB, et al. Channelling inflammation: Gasdermins in physiology and disease[J]. Nat Rev Drug Discov, 2021, 20( 5): 384- 405. DOI: 10.1038/s41573-021-00154-z. |
| [4] |
AMBADE A, LOWE P, KODYS K, et al. Pharmacological inhibition of CCR2/5 signaling prevents and reverses alcohol-induced liver damage, steatosis, and inflammation in mice[J]. Hepatology, 2019, 69( 3): 1105- 1121. DOI: 10.1002/hep.30249. |
| [5] |
|
| [6] |
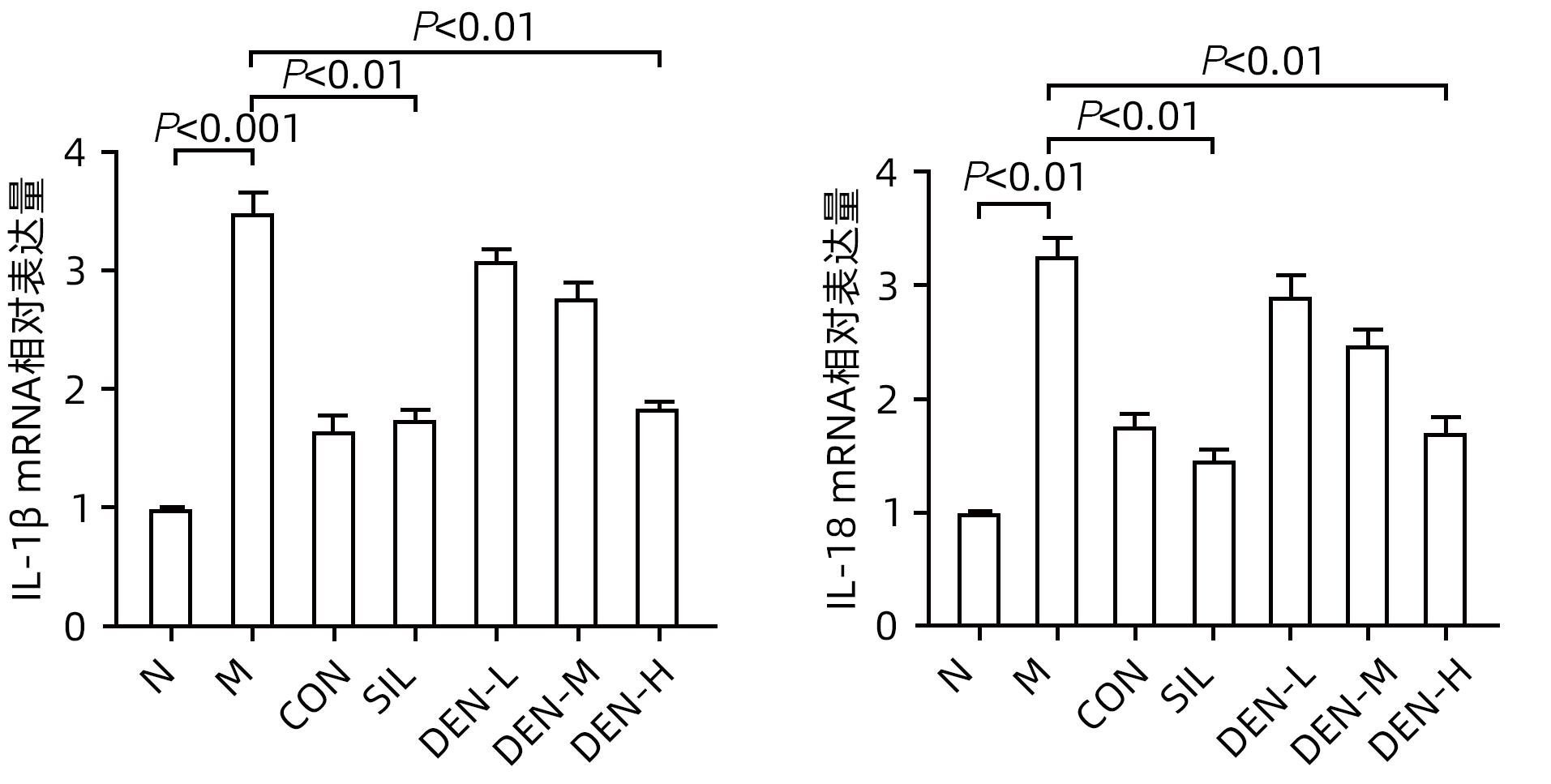
LIU YG, YANG LL, ZHANG Y, et al. Dendrobium officinale polysaccharide ameliorates diabetic hepatic glucose metabolism via glucagon-mediated signaling pathways and modifying liver-glycogen structure[J]. J Ethnopharmacol, 2020, 248: 112308. DOI: 10.1016/j.jep.2019.112308. |
| [7] |
CHU WH, WANG P, MA Z, et al. Ultrasonic treatment of Dendrobium officinale polysaccharide enhances antioxidant and anti-inflammatory activity in a mouse D-galactose-induced aging model[J]. Food Sci Nutr, 2022, 10( 8): 2620- 2630. DOI: 10.1002/fsn3.2867. |
| [8] |
YANG K, ZHAN LH, LU TT, et al. Dendrobium officinale polysaccharides protected against ethanol-induced acute liver injury in vivo and in vitro via the TLR4/NF-κB signaling pathway[J]. Cytokine, 2020, 130: 155058. DOI: 10.1016/j.cyto.2020.155058. |
| [9] |
YUAN C, LIAN QH, NI BB, et al. Screening and bioinformatics analysis of key autophagy-related genes in alcoholic hepatitis[J]. Ogran Transplant, 2024, 15( 1): 90- 101.
袁超, 练庆海, 尼贝贝, 等. 酒精性肝炎自噬关键基因的筛选及生物信息学分析[J]. 器官移植, 2024, 15( 1): 90- 101.
|
| [10] |
XU H, XIAO P, ZHANG F, et al. Epidemic characteristics of alcohol-related liver disease in Asia from 2000 to 2020: A systematic review and meta-analysis[J]. Liver Int, 2022, 42( 9): 1991- 1998. DOI: 10.1111/liv.15312. |
| [11] |
SUNG H, KIM SW, HONG M, et al. Microbiota-based treatments in alcoholic liver disease[J]. World J Gastroenterol, 2016, 22( 29): 6673- 6682. DOI: 10.3748/wjg.v22.i29.6673. |
| [12] |
YI YS. Caspase-11 non-canonical inflammasome: A critical sensor of intracellular lipopolysaccharide in macrophage-mediated inflammatory responses[J]. Immunology, 2017, 152( 2): 207- 217. DOI: 10.1111/imm.12787. |
| [13] |
KHANOVA E, WU R, WANG W, et al. Pyroptosis by caspase11/4-gasdermin-D pathway in alcoholic hepatitis in mice and patients[J]. Hepatology, 2018, 67( 5): 1737- 1753. DOI: 10.1002/hep.29645. |
| [14] |
HEO MJ, KIM TH, YOU JS, et al. Alcohol dysregulates miR-148a in hepatocytes through FoxO1, facilitating pyroptosis via TXNIP overexpression[J]. Gut, 2019, 68( 4): 708- 720. DOI: 10.1136/gutjnl-2017-315123. |
| [15] |
WU YL, HUANG SH, HE CM, et al. Dendrobium officinale flower extraction mitigates alcohol-induced liver injury in mice: Role of antisteatosis, antioxidative, and anti-inflammatory[J]. Evid Based Complement Alternat Med, 2020, 2020: 1421853. DOI: 10.1155/2020/1421853. |
| [16] |
YUAN HQ, LIANG CY, LIANG J, et al. Protection of Dendrobium Officinale against acute alcoholic liver injury in mice[J]. J Jinan Univ Nat Sci Med Ed, 2016, 37( 5): 384- 388. DOI: 10.11778/j.jdxb.2016.05.005. |







 DownLoad:
DownLoad: