2024, 40(2): 335-342.
DOI: 10.12449/JCH240218
Abstract:
Objective To investigate the intervention mechanism of Dendrobium officinale leaf fermentation fluid in mice with alcoholic hepatitis. Methods A total of 70 healthy male C57BL/6J mice, aged 6-8 weeks, were randomly divided into normal group, model group, liquid feed control group, silybin group, and low-, middle-, and high-dose Dendrobium officinale leaf fermentation fluid groups, with 10 mice in each group. The mice in the normal group were given normal diet, and those in the other groups were given Lieber-DeCarli classic liquid diet for 8 weeks to induce alcoholic hepatitis. During modeling, the mice in the low-, middle-, and high-dose Dendrobium officinale leaf fermentation fluid groups were given Dendrobium liquid manufactured by Warmen Pharmaceutical, and the mice in all the other groups were given pure water; the mice in the normal group, the model group, and the liquid feed control group were given normal saline by gavage, those in the silybin group were given silybin 0.25 mL/10 g by gavage, and those in the low-, middle-, and high-dose Dendrobium officinale leaf fermentation fluid groups were given Dendrobium officinale leaf fermentation fluid at a dose of 0.125 mL/10 g, 0.250 mL/10 g, and 0.375 mL/10 g, respectively, by gavage, once a day. At week 8, chloral hydrate was injected intraperitoneally for anesthesia, and blood samples were collected from the eyeball. After serum was separated, the biochemical method was used to measure the levels of aspartate aminotransferase (AST) and alanine aminotransferase (ALT); HE staining and oil red staining were used to observe liver histopathology and lipid accumulation in mice; multiplex Luminex assay was used to measure the serum levels of interleukin-6 (IL-6), interleukin-1β (IL-1β), tumor necrosis factor-α (TNF-α), and CCL2; quantitative real-time PCR, Western blot, and immunofluorescence assay were used to measure the protein expression levels of NLRP3, caspase-1, caspase-11, gasdermin D (GSDMD), N-terminal gasdermin D (GSDMD-N) in liver tissue. A one-way analysis of variance was used for comparison of continuous data between multiple groups, and the least significant difference t-test was used for further comparison between two groups. Results Compared with the normal group, the model group had significant increases in the serum levels of AST, ALT, IL-6, IL-1β, TNF-α, and CCL2 (all P<0.05), and compared with the model group, the high-dose Dendrobium officinale leaf fermentation fluid group had significant reductions in the serum levels of AST, ALT, IL-6, IL-1β, TNF-α, and CCL2 (all P<0.05). HE staining showed that the model group had disordered structure of hepatic lobules, with a large number of steatosis vacuoles and massive cell necrosis, and compared with the model group, the high-dose Dendrobium officinale leaf fermentation fluid group had alleviation of liver histopathological injury, intact structure of most hepatic lobules, and a small amount of inflammatory cell infiltration. Oil red staining showed that the model group had accumulation of large and small lipid droplets in the liver and a significant increase in liver fat content, and compared with the model group, the high-dose Dendrobium officinale leaf fermentation fluid group had significant alleviation of hepatic steatosis, with the presence of sporadic small lipid droplets. Immunofluorescence assay of liver tissue showed that compared with the normal group, the model group had a significant increase in the ratio of GSDMD-positive staining area in hepatocyte cytoplasm (P<0.001), and compared with the model group, the high-dose Dendrobium officinale leaf fermentation fluid group had a significant reduction in such ratio in hepatocyte cytoplasm (P<0.001). Quantitative real-time PCR showed that compared with the normal group, the model group had significant increases in the protein expression levels of NLRP3, caspase-1, caspase-11, GSDMD, GSDMD-N, interleukin-18 (IL-18), and IL-1β in liver tissue (all P<0.05), and compared with the model group, the high-dose Dendrobium officinale leaf fermentation fluid group had significant reductions in the protein expression levels of NLRP3, caspase-1, caspase-11, GSDMD, GSDMD-N, IL-18, and IL-1 (all P<0.05). Compared with the model group, the high-dose Dendrobium officinale leaf fermentation fluid group had significant reductions in the protein expression levels of caspase-1 and caspase-11 (both P<0.05), with a relative expression level of caspase-1 of 1.757 (reduced by 26.6% compared with the model group) and a relative expression level of caspase-11 of 0.455 (reduced by 70.3% compared with the model group), suggesting that caspase-11 showed a greater reduction than caspase-1. Conclusion Dendrobium officinale leaf fermentation fluid can alleviate alcoholic hepatitis in mice, possibly by inhibiting the non-classical cell pyroptosis pathway mediated by caspase-11.
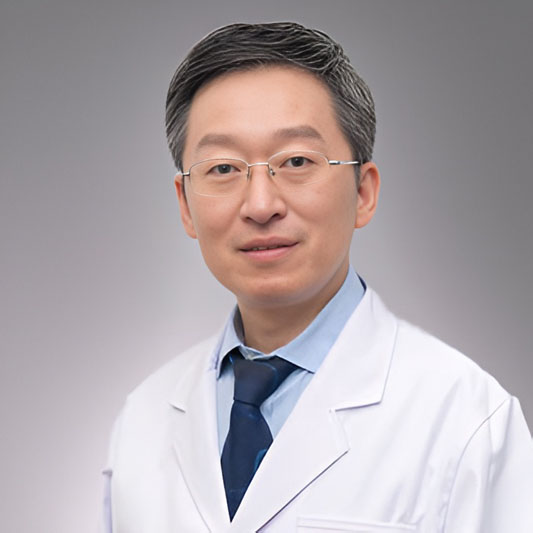
ZHOU XN, LIU YH, QIN YJ, et al. Effect of Dendrobium officinale leaf fermentation fluid on a mouse model of alcoholic hepatitis and its mechanism of action[J]. J Clin Hepatol, 2024, 40(2): 335-342.. doi: 10.12449/JCH240218.

 Abstract
Abstract HTML
HTML PDF (546KB)
PDF (546KB)